request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Prostate Cancer
- Prostate Cancer Treatment
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsProstate Cancer Treatment
Your treatment plan will depend on a variety of factors, including:
- Overall health and well-being
- Age
- Grade and associated risk of your cancer
- Goals for treatment outcomes
Talk with your doctor about which treatments are available and how those treatments may affect you. One or more of the following therapies may be used to treat your cancer.
Active surveillance or watchful waiting
Because prostate cancer usually grows slowly, doctors may recommend some patients not be treated. These patients are typically older and/or have a very low-risk form of prostate cancer.
Instead, these patients can be put on active surveillance, or “watchful waiting.”
This approach involves closely monitoring the cancer without treatment. Prostate biopsy procedures and PSA tests are repeated at set intervals. Treatment may be recommended if the tests show the disease is progressing.
Surgery
Surgery for prostate cancer is known as a radical prostatectomy. During this procedure, the surgeon removes the entire prostate. Lymph nodes near the prostate may also be removed to look for evidence that the disease has spread.
Nearly all prostate cancer surgeries at MD Anderson are minimally invasive procedures performed with surgical robots. These surgeries result in smaller incisions, less blood loss, less pain and shorter hospital stays.
Surgery for prostate cancer usually requires an overnight hospital stay. Patients must wear a catheter for about one week after the procedure. They typically can return to work after two weeks. There are no restrictions on activity after four weeks.
Studies have shown that working with an experienced surgeon increases the odds for a successful procedure with fewer side effects. The surgeons at MD Anderson are among the most experienced and skilled in the world in prostate cancer surgeries.
Radiation therapy
Radiation therapy uses high-energy beams to kill disease cells. Along with surgery, it is one of the two most common primary treatments for prostate cancer. Compared to surgery, it offers better urinary control but is more likely to cause bowel and bladder irritability. Both can cause erectile dysfunction.
There are several different types of radiation therapy doctors recommend to prostate cancer patients. Most treatment plans require daily treatment for a number of weeks.
- Intensity-modulated radiation therapy (IMRT): IMRT focuses multiple radiation beams of different intensities directly on the tumor for the highest possible dose of radiation. Radiation oncologists use special planning software to make sure the patient is properly positioned for the most accurate treatment.
- Stereotactic body radiation therapy (SBRT): Also known as stereotactic ablative radiotherapy (SABR), SBRT administers very high doses of radiation, using several beams of various intensities aimed at different angles to precisely target the tumor. This treatment usually takes around 10 days, making it significantly shorter than other forms of radiation therapy.
- Brachytherapy: Brachytherapy delivers radiation therapy with small pieces of radioactive material (usually about the size of a grain of rice) that are placed inside the patient’s body as close to the tumor as possible. This allows doctors to deliver very high doses of radiation directly to the patient’s tumor while limiting radiation exposure to healthy tissue.
- Proton therapy: This type of therapy is similar to traditional radiation therapy, but it uses a different type of radiation and is much more accurate at targeting tumors.
- Radionuclide therapy: This type of radiation therapy is actually administered through an IV. It is used to treat prostate cancer bone metastases (prostate cancer that has spread to the bones).
MD Anderson has the most advanced radiation therapies and has radiation oncologists who specialize in prostate cancer. This allows us to offer the most effective radiation treatments while minimizing side effects.
Hormone therapy
The majority of prostate cancers are hormone-sensitive, which means male hormones (androgens) such as testosterone fuel the growth of prostate cancer. About one-third of prostate cancer patients require hormone therapy (also known as androgen deprivation therapy). While hormone therapy can reduce tumor size and make cancer grow more slowly, it does not cure the disease.
There are two main types of hormone therapy for prostate cancer patients:
- Antiandrogens: Antiandrogens are medications that block testosterone and other androgens from interacting with the cancer cell. They are taken by mouth every day. Antiandrogens are used most often in combination with androgen synthesis inhibitors.
- Androgen synthesis inhibitors: These drugs reduce levels of testosterone and other androgens produced by the body. A common type of androgen synthesis inhibitor is luteinizing hormone-releasing hormone (LHRH) agonists. Because LHRH agonists are often associated with a temporary increase in testosterone levels, they may be combined with anti-androgen medications. Androgen synthesis inhibitors are delivered by injections, which last from one to six months, or by small pellets implanted under the skin.
Hormone therapy is most often used for late-stage, high-grade tumors with a Gleason score of 8 or higher or in patients with cancer that has spread outside the prostate.
Hormone therapy may be used to treat prostate cancer if:
- Surgery or radiation is not possible
- Cancer has metastasized (spread) or recurred (come back after treatment)
- Cancer is at high risk of returning after radiation
- Shrinking the cancer before surgery or radiation increases the chance for successful treatment
Side effects of hormone therapies for prostate cancer may include:
- Impotence, inability to get or maintain an erection
- Loss of libido (sex drive)
- Hot flashes
- Growth of breast tissue and tenderness of breasts
- Loss of muscle mass, weakness
- Decreased bone mass (osteoporosis)
- Shrunken testicles
- Depression
- Loss of alertness and higher cognitive functions
- Anemia (low red blood cell count)
- Weight gain
- Fatigue
- Higher cholesterol levels
- Increased risk of heart attacks, diabetes and high blood pressure (hypertension)
If you are treated with hormone therapy and have side effects, be sure to mention them to your doctors. Many of these side effects can be treated successfully.
Chemotherapy
Chemotherapy drugs are designed to kill fast-growing cells, including cancer cells. For prostate cancer, chemotherapy is most often used to treat patients with a high-risk disease or whose cancer has recurred or metastasized.
Cryotherapy
Though rarely used, cryotherapy is the best choice for localized prostate cancer where tumors are small and surgery is not an option. During these procedures, a long, thin probe is inserted into the tumor, freezing and killing cancer cells. Intensive follow-up with X-rays or other imaging procedures is used to ensure that the tumor has been destroyed.
Immunotherapy
Immunotherapy recruits a patient's own immune system in the fight against cancer. Patients may be given a type of immunotherapy that involves engineering the immune cells of the body in a lab to recognize prostate cancer. This approach may be especially useful for patients with advanced prostate cancer that does not respond to hormone therapy.
High-intensity focused ultrasound (HIFU)
High-intensity focused ultrasound (HIFU) kills cancer tissue in the prostate with heat generated by focused ultrasound waves. The treatment may offer improved urinary and sexual function to some prostate cancer patients. HIFU is typically offered to patients with early-stage prostate cancer that is low- to intermediate-risk. The tumor must be visible on MRI. It must be confined to the prostate and be confirmed to contain prostate gland cells.
Clinical trials
As one of the world’s leading cancer centers, MD Anderson is home to many clinical trials for prostate cancer patients. Your care team may discuss clinical trials with you if they believe they offer you a better outcome than standard treatments.
Trials are designed to improve prostate cancer survival rates, minimize treatment side effects and support a higher quality of life for patients. They may include new drugs or drug combinations, new approaches to prostate cancer surgery, different forms of radiation therapy, or some combination of all three. Learn more about clinical trials.
Treatment plans for prostate cancer
When prostate cancer is diagnosed, doctors use several different tests to determine the risk of disease progression. Patients in each risk group often get the same general recommendations for treatment.
Low-risk prostate cancer treatment
Many low-risk prostate cancers can go years or even decades without causing any serious health problems. Because of this, doctors often recommend active surveillance for these patients. During active surveillance, a patient is closely monitored for changes to his cancer.
In some cases, low-risk prostate cancer patients do choose to have treatment. A younger patient, for example, may select treatment instead of potentially decades of surveillance. Patients with low-risk disease may also choose treatment if they have certain genetic conditions or a large amount of cancer tissue.
Intermediate-risk prostate cancer treatment
Men with intermediate-risk prostate cancer should be treated in most cases. Treatment options typically are surgery to remove the prostate or radiation therapy. The patient may also get hormone therapy along with radiation therapy.
High-risk prostate cancer treatment
Low- and intermediate-risk prostate cancers are usually considered curable. Some high-risk prostate cancers can be cured. In other cases it is not curable and is treated like a chronic disease that must be managed.
Whether curable or not, high-risk prostate cancer is usually treated with a combination of therapies. Standard options include surgery, radiation therapy, hormone therapy and chemotherapy. Doctors will recommend the combination based on each patient’s specific cancer subtype, its stage, the patient’s age and other factors. They may also recommend a clinical trial if they believe that trial offers the best treatment. Clinical trials can be used to test new therapies or new combinations of existing therapies.
Recurrent prostate cancer treatment
For most patients, initial prostate cancer treatment includes either radiation therapy or surgery. If a patient’s prostate cancer returns, the other treatment option may be used. In addition, doctors may recommend the use of systemic therapies (therapies that travel throughout the body), like hormone therapy and possibly chemotherapy.
In some cases, patients can have what is known as biochemical recurrence. These patients have elevated PSA levels that indicate the disease has returned, but imaging exams do not show any cancer. Patients with biochemical recurrence are given intermittent hormone therapy and are monitored closely for further changes.
Metastatic prostate cancer treatment
If a patient’s prostate cancer has spread beyond the prostate and the surrounding area, he is given systemic therapies like hormone therapy and possibly chemotherapy. While cancer responds to hormone therapy, it is called castrate-sensitive disease. Over time, the disease may become less responsive to hormone therapy and start growing again. This is called castrate-resistant disease. Patients with castrate-resistant disease can be treated with a number of additional therapies. Many are eligible for clinical trials with newer drugs or drug combinations, including immunotherapy.
Some cases of prostate cancer can be passed down from one generation to the next.
Learn more about genetic testing
Learn more about prostate cancer:

What are the top 5 warning signs of prostate cancer?
Prostate cancer is a type of cancer that develops in the prostate, a small walnut-shaped gland in the male reproductive system. It is the second most common cancer among males in the U.S.
Most people with stage I prostate cancer don’t show any symptoms. “For prostate cancer to cause symptoms, it may be at an advanced stage when it becomes harder to cure,” says urologic oncologist Lisly Chéry, M.D. “That’s why prostate cancer screening is so important.”
We spoke with Chéry to learn more about prostate cancer symptoms, screening guidelines and how to lower your risk of developing prostate cancer.
Symptoms of prostate cancer
The top 5 early warning signs of prostate cancer may include:
Blood in urine
If your urine is pink or red, you should see a primary care doctor or urologist.
“This is a ‘do not pass go’ moment,” says Chéry. “Even if there is no pain or it only happens one time, get evaluated to see what’s going on if you have blood in your urine.”
Difficulty urinating
Urinary retention is when you have difficulty urinating or completely emptying your bladder.
“The urethra, or the tube you urinate from, runs through the prostate,” says Chéry. “As prostate cancer grows, it can cause that tube to collapse and make it so the bladder cannot get urine past it. Sometimes, it requires insertion of a catheter to go inside the bladder to remove the urine.”
Pelvic pain
Pain or a sensation in the pelvis can be a sign of advanced prostate cancer.
“As prostate cancer grows, it can start to invade the muscles in the pelvis or rectal wall,” says Chéry. “This can give you the sensation that you’re sitting on a ball because the prostate may be inflamed.”
Frequent urination
You may wake up several times during the night to use the bathroom or go more often during the day.
Weak urine stream
This can include difficulty starting or maintaining a flow of urine.
Other, less common signs include:
Bone pain
Pain in your bones and joints can be an indication that the prostate cancer has metastasized, or spread, to your bones.
Blood in semen
Blood in the semen is rare, but you should see a doctor if it occurs.
Painful or burning urination
You may experience pain or a burning sensation when urinating.
Difficulty holding back urine
This happens when you unintentionally pass urine.
Erectile dysfunction
You may have difficulty having or maintaining an erection.
“It’s very common for men to have problems with their prostate, especially as they age,” says Chéry. “It’s important to know that these symptoms aren’t always associated with prostate cancer.”
Discuss prostate cancer screening with your doctor
If prostate cancer is caught early, it’s easier to treat and cure.
It’s recommended to speak with your primary care physician or urologist about prostate cancer screening at age 45. Men at high risk for prostate cancer can have those discussions as early as age 40.
Risk factors for developing prostate cancer include:
- Age: The average age of diagnosis in the U.S. is 66. It’s uncommon in men under age 50.
- Race: African American men or men of African descent have nearly double the risk of prostate cancer than white men.
- Hereditary cancer syndromes: Certain genetic mutations, like BRCA1 and BRCA2, can increase the risk of prostate cancer.
- Family history: Your risk is higher when a close blood relative (e.g., father or brother) has or had prostate cancer.
A prostate-specific antigen (PSA) screening test is the most common way to detect prostate cancer. PSA is a protein found in the blood in the prostate. If your PSA levels are elevated, it could mean you have prostate cancer – but not always.
“Your PSA can go up for many reasons,” says Chéry. “Just because your PSA is elevated, it doesn’t necessarily mean you have cancer. Your doctor will examine you to figure out what’s going on.”
Prostate cancer screening can also include a digital rectal exam.
“The prostate is positioned right in front of the rectum and the back of the prostate is where cancer most often forms,” explains Chéry. “During a digital rectal exam, a doctor will insert a gloved finger into your rectum to feel for any abnormalities in your prostate.”
You cannot check yourself for prostate cancer, so getting screened for prostate cancer is the best method of detection.
“Knowing your PSA level and staying on top of it year after year has shown to be beneficial in preventing death from prostate cancer,” says Chéry. “If you develop prostate cancer and catch it early, you’ll have more treatment options and a better chance of getting cured. Don’t wait until prostate cancer finds you; find it first by staying on top of your screenings.”
Other medical conditions may mimic prostate cancer symptoms
As men get older, the front of the prostate (where the urethra runs through) will grow. Symptoms caused by this growth may mimic the symptoms of prostate cancer and cause your PSA levels to go up. But most of the time, these conditions will not be prostate cancer.
Two common prostate-related problems are:
- Benign prostatic hyperplasia (BPH): a non-cancerous growth in the prostate, also known as an enlarged prostate
- Prostatitis: an infection of the prostate associated with inflammation that can cause fever, pelvic pain and frequent urination
Be sure to see a doctor if you experience any new or strange symptoms. These non-cancerous conditions can usually be treated with medication.
Lower your risk of prostate cancer
Data shows that following a healthy diet such as the Mediterranean diet may help lower your risk of developing prostate cancer. It can also reduce the risk of recurrence if you already have prostate cancer.
The Mediterranean diet is high in vegetables, whole grains, fruits, legumes and healthy fats. Seeds and nuts are also included.
“Studies show that this type of diet can also lower your risk of heart disease and stroke,” says Chéry. “It’s like a double bang for your buck in that it reduces your risk for prostate cancer and is also good for your heart.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Treatment at MD Anderson
Prostate cancer is treated in our Genitourinary Center and our Proton Therapy Center.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.

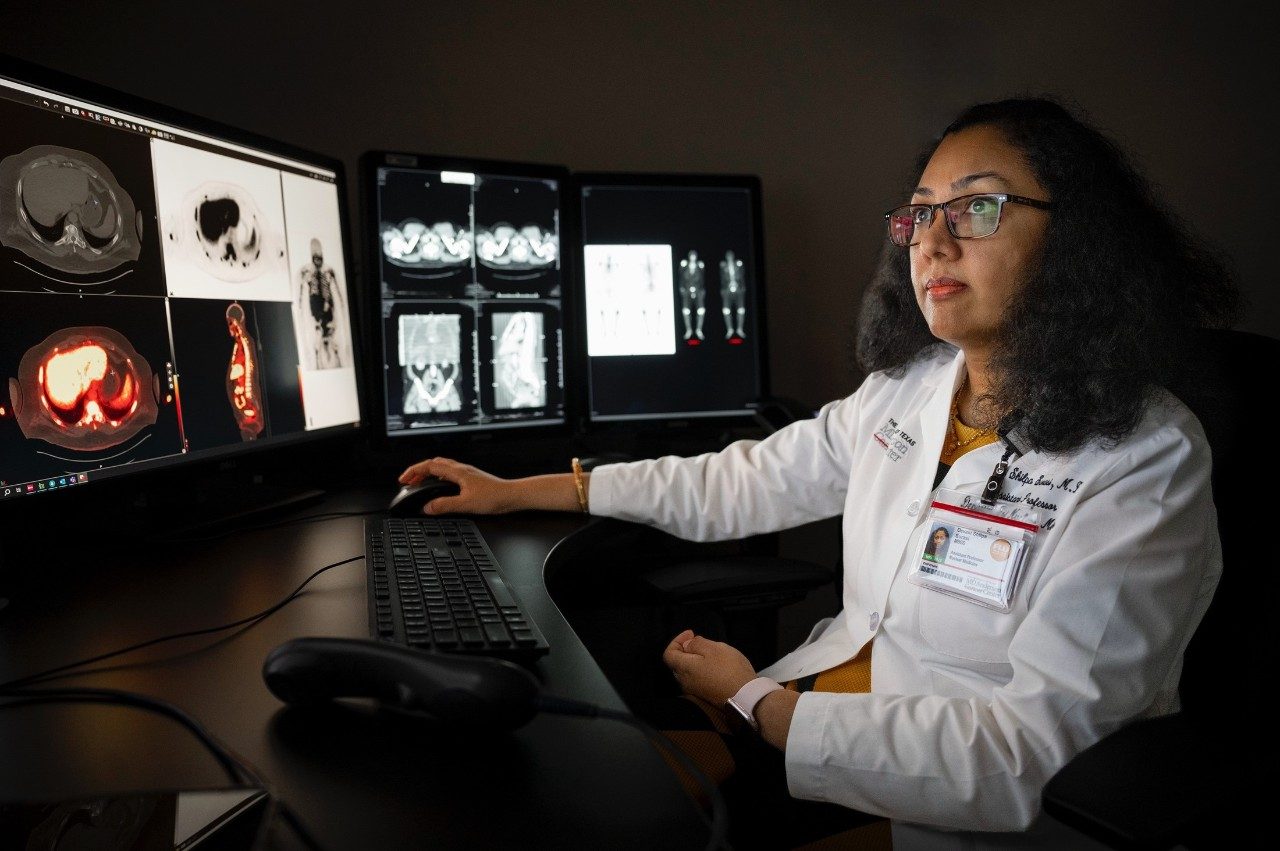
Stereotactic body radiation therapy (SBRT) for prostate cancer: What to know
If you have received a prostate cancer diagnosis, you may be wondering which treatment options are available to you. Prostate cancer treatment options can include surgery, different types of radiation therapy and hormone therapy. Once your doctor identifies if your localized prostate cancer has a low risk, intermediate risk or high risk of the cancer spreading, they can determine the best treatment options for you.
Stereotactic body radiation therapy (SBRT) is a radiation treatment that uses high doses of radiation with several beams of various intensities aimed at different angles to precisely target the tumor. This limits radiation exposure to healthy tissue and offers several benefits to patients undergoing prostate cancer treatment. To better understand SBRT, we spoke with radiation oncologist Karen Hoffman, M.D., who specializes in caring for patients with prostate cancer.
How is stereotactic body radiation therapy for prostate cancer different from other radiation therapies?
Standard external beam radiation therapy for prostate cancer requires 20 to 28 treatments given over 4 to 6 weeks, whereas SBRT requires just five days of treatment. With fewer treatments, there is much less disruption to patients’ lives, especially for those who live far away.
SBRT has been shown in clinical trials to be as effective in controlling prostate cancer as longer-duration radiation for patients with low- and intermediate-risk disease. Patients receiving SBRT for prostate cancer may initially experience more urinary symptoms, but long-term urinary and bowel function is similar to the function you would have after longer duration radiation treatment.
With SBRT, we shorten the duration of treatment by giving larger amounts of radiation each day, using a more focused and precise radiation treatment.
We are now treating patients with SBRT at several of MD Anderson’s Houston locations. This offers patients even more convenience during treatment.
At our Texas Medical Center Campus, we treat patients with SBRT using MR-Linac radiation therapy. MR-Linac delivers precise high-dose radiation to patients inside an MRI machine. The machine constantly obtains images during treatment, providing high-resolution images of the tumor and control of the radiation beam in real time.
This allows your care team to deliver high-dose radiation to tumors that can change shape or move during treatment. Our doctors can get information about not only the tumor but also normal surrounding tissue so they can modify and adapt your treatment plan daily if needed. This new technology keeps the radiation beam directly on target throughout treatment, providing even more precise treatment to protect normal tissues around it.
What can prostate patients expect from a typical SBRT treatment plan?
For prostate cancer, SBRT is an effective short course of radiation that can be given in just five treatments.
Patients first meet with one of our physicians to verify they are a candidate for SBRT. Then, we do a planning appointment, a CT scan and an MRI scan to help map out where the radiation would go. You return one week later to start a typical SBRT treatment plan, which is five days of treatments delivered every other day.
The most common early side effect is more frequent urination. Patients may also experience discomfort while urinating. These side effects can be managed with medication and typically go away after treatment. Most patients can maintain their usual activities during treatment.
Many patients receive SBRT by itself. However, depending on your case, you might receive testosterone suppression with the radiation. You can eat and drink normally during treatment. When you undergo treatment, we typically ask you to have a full bladder and an empty rectum.
What new research is being done for prostate cancer patients receiving SBRT?
As a leader in treating prostate cancers, MD Anderson has clinical trials for patients who have newly diagnosed, recurrent or progressive diseases.
A recent prostate cancer randomized Phase III trial of stereotactic body radiotherapy in localized prostate cancer shows that five-fraction SBRT was non-inferior to control radiation therapy with respect to biochemical or clinical failure and is an effective treatment option for patients with low-to-intermediate-risk localized prostate cancer. Patients treated with SBRT reported more urinary side effects two years after treatment, but differences in urinary symptoms went away by five years.
Given the convenience of SBRT for treating prostate cancer, ongoing clinical trials at MD Anderson are looking to expand patients eligible for this treatment. Hoffman is leading a national trial, the NRG GU013 trial, which is comparing prostate SBRT to traditional multi-week radiation for patients with high-risk prostate cancer.
The PRORAD-5 clinical trial is testing SBRT for patients who need radiation treatment to the pelvic lymph nodes in addition to the prostate. The PRORAD-5 trial is led by Comron Hassanzadeh, M.D., and is only available at MD Anderson.
What advice do you have for prostate cancer patients?
Patients with localized prostate cancer should discuss SBRT options with their care team to determine if they are a candidate for five-treatment radiation.
Choosing the right hospital may be the most important decision you make as a prostate cancer patient. At MD Anderson you will get care and support from the nation’s top-ranked cancer center. If you experience side effects, talk to your care team. We can help you come up with strategies to cope. From a dedicated prostate cancer support group to counseling to integrative medicine care, we have all the services needed to treat not just the disease, but the whole person.
Most importantly, look for a care team that makes you feel comfortable and is experienced to ensure you are getting the best treatment possible for the best possible outcome.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Prostate cancer survivor grateful for high-intensity focused ultrasound (HIFU)
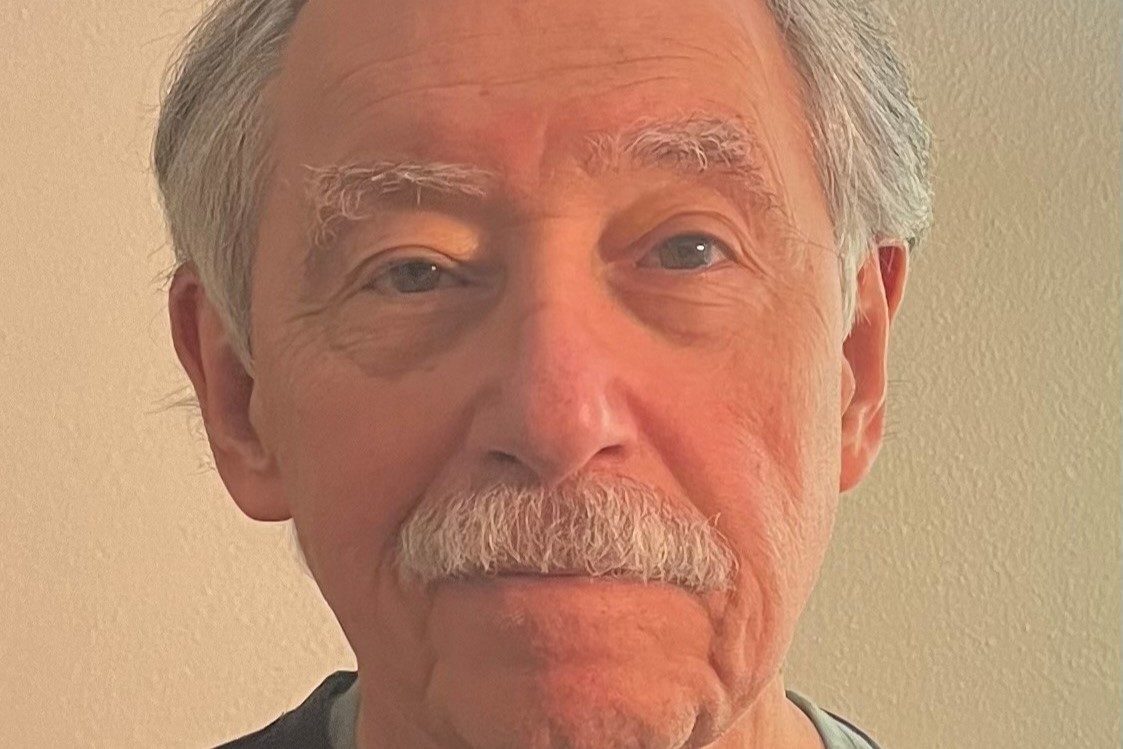
When Howard Walton visited his primary care doctor in August 2022, she was concerned his prostate-specific antigen (PSA) levels were rising too quickly. Later that month, Howard saw his urologist, who found that his PSA levels had risen significantly since he’d last seen Howard.
Howard’s urologist ordered a biopsy, and the results showed he had prostate cancer. He met with doctors at an Ohio hospital; they discussed two options: radiation therapy or surgery. Howard and his wife were already planning to spend the winter with their daughter in Houston, so instead of waiting to start treatment until they were back in Ohio, Howard told his urologist he wanted to go to MD Anderson. He called and got an appointment with John Ward, M.D., in November.
Another treatment option: high-intensity focused ultrasound
At his initial appointment, Ward suggested Howard might be a candidate for high-intensity focused ultrasound (HIFU), a treatment that uses heat generated by focused ultrasound waves to kill cancer tissue in the prostate. Patients who have early-stage prostate cancer with an MRI-identified tumor are typically good candidates for HIFU.
During HIFU treatment, the patient is put under general anesthesia before the doctor places an ultrasound probe in the rectum and takes an image of the prostate. Data from the image is used to create a three-dimensional model of the prostate to determine the exact location, size and shape of the tumor. The probe, under robotic control, then releases focused, high-energy sound waves to the tumor to heat and kill cancer cells.
Howard had never heard of HIFU, but after Ward described the procedure, he was convinced it would be the best option instead of radiation therapy.
“I found the idea of a one-time treatment much more preferable than six or seven weeks of radiation every day,” Howard says. “My mind was made up. I was convinced that if I was eligible, that's what I wanted to have done.”
‘Best decision’ to undergo HIFU
After undergoing an MRI, Howard was determined to be eligible for HIFU. He underwent the procedure in December and went home the same day. At the end of the procedure, Ward inserted a Foley catheter, a soft tube that continuously drains urine from the bladder into a drainage bag. It was removed a week later.
Howard calls undergoing HIFU "the best decision” for him. Even though Ward cautioned that a recurrence of the cancer was possible, Howard says Ward’s confidence in the procedure convinced him to choose HIFU over other treatment options.
“Dr. Ward exuded confidence, and I could feel that,” Howard says. “It made me more comfortable. Everyone I saw in connection with the procedure was so professional, kind and courteous. I have told more people, especially men, how common prostate cancer is. I tell them, ‘If you get prostate cancer, call MD Anderson. There’s no place like it.’”
Request an appointment at MD Anderson online or call 1-877-632-6789.
Prostate cancer survivor grateful for stereotactic body radiation therapy (SBRT)
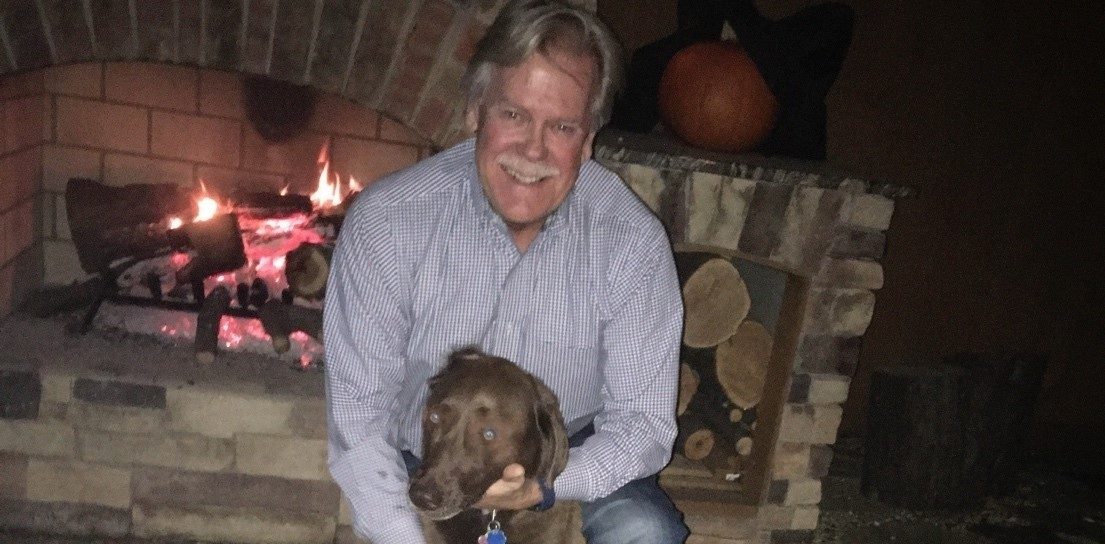
With a family history of prostate cancer, Keith Burchfield did not wait to talk to his doctor about the risks and benefits of early prostate cancer screening.
At his yearly exam, his prostate-specific antigen (PSA) levels had significantly changed since the previous year. There was a 50% chance that he had early-stage prostate cancer. PSA levels show up through a blood test that measures the amount of PSA circulating in the blood. This level is used to assess prostate cancer risk.
Knowing MD Anderson is the top cancer hospital in the nation, he requested an appointment online right away. “I live in the Dallas area and was willing to make the 4-hour drive for the expertise and top treatment options,” says Keith. “I did not want to waste any time.”
Finding expertise and reassurance at MD Anderson
Keith’s first appointment at MD Anderson was scheduled in November 2020, during the COVID-19 pandemic. He met with urologist Justin Gregg, M.D., who ordered an MRI to be done in Dallas so Keith could be close to home.
After the MRI, Gregg confirmed Keith had four lesions. The previous hospital had only detected three. Keith had a biopsy at MD Anderson, then went back to Dallas to wait for his results. Shortly thereafter, Gregg called to let Keith know that the biopsy confirmed he had stage II prostate cancer.
Gregg outlined Keith’s prostate cancer treatment options: surgery, radiation therapy or active surveillance – also known as watchful waiting. “Dr. Gregg answered all my questions with great care. This helped me and my wife, Judy, decide what type of treatment was best for me,” says Keith.
He did not want to postpone treatment by choosing active surveillance. He also didn’t want to face the possibility of side effects from surgery. So, Keith chose radiation therapy. He knew he had a window of opportunity and did not want to wonder if the cancer would become aggressive.
“I was presented with the gift of early detection and wanted to do something as soon as possible,” he says.
Undergoing SBRT for prostate cancer treatment
In February 2021, Keith traveled to Houston to meet with radiation oncologist Karen Hoffman, M.D., and Sarah Todd, her physician assistant at the time.
“Dr. Hoffman and Sarah took the time to explain the types of radiation therapy treatments that I qualified for,” remembers Keith. Each radiation type uses a different number of treatments, either daily radiation for weeks or a short-term radiation for five sessions.
After talking it over with his wife, Keith decided to undergo a short-term radiation therapy called stereotactic body radiation therapy (SBRT). SBRT typically consists of five treatments using a high dose of radiation to treat the tumor’s exact location and shape. A customized treatment plan sets the angles and intensities of the radiation beams.
Keith decided to commute to Houston from Dallas for his five daily SBRT treatments. It happened to be the week of the February 2021 winter storm, an historic winter weather event in Houston resulting in road closures, widespread power outages, loss of heat and broken pipes across Texas.
“I am very thankful that Dr. Hoffman and Sarah are so easy and wonderful to work with. They stayed in continuous communication with me. They made sure I was able to stay on track with my treatments during the bad winter storm – even treating me on a Saturday to make up a missed appointment during the week,” he says.
Keith does not recall experiencing any significant side effects from SBRT. “While every treatment has side effects, I did not notice anything out of the norm from treatment. I had energy to drive back and forth each day,” he says. “And the staff accommodated my travel schedule and arranged my appointments for later in the morning or early afternoon.”
Cherishing every moment after successful SBRT
Three years after treatment, Keith continues to enjoy life after cancer. He meets with Todd every six months to review his PSA levels via a telehealth visit and make sure his prostate cancer stays in remission. In July, he will switch to annual visits.
“My father was diagnosed with stage IV prostate cancer many years ago when they did not have the technology and treatment options available today,” says Keith. “I’m thankful for the advances in radiation therapy.”
Keith is glad he got annual exams to keep an eye on his PSA levels. Most people with stage I or II prostate cancer do not show any symptoms. He tells other men: If you develop prostate cancer and catch it early, you will have more treatment options and a better chance of getting cured.
Not doing active surveillance was an easy decision for Keith. He did not want to have regrets, and he knew the treatment would be more challenging if he was diagnosed with advanced disease.
“Know the prostate cancer warning signs and stay on top of your PSA screenings, especially if you have a family history,” he says. “Early diagnosis is the key to effective treatment.”
Request an appointment at MD Anderson online or call 1-877-632-6789.

Pelvic floor physical therapy: 5 questions answered
Nikki Samms, DPT, knows the region of the body she treats can make people uncomfortable.
As an MD Anderson pelvic floor physical therapist, Samms spends her days helping patients navigate a wide range of pelvic floor issues ranging from trouble using the bathroom to pain with intercourse to organ prolapse.
“Our society puts a lot of taboo on discussing all things pelvis,” she says. “A lot of my patients feel like they're sort of suffering in silence or they're the only human on earth experiencing the problems that they are because we've just put so much shame around our pelvises.”
Thankfully, pelvic floor physical therapy can help those who are experiencing pelvic floor issues. Ahead, Samms answers questions about the pelvic floor and pelvic floor physical therapy, including what treatments are used, who might benefit and what happens during an appointment.
What is the pelvic floor?
First things first: What exactly is the pelvic floor? Where is it? And what does it do?
Samms describes the pelvis as a ‘tight neighborhood’ housing a variety of organs including the bladder, rectum and, for women, the uterus.
There are three layers of muscles at the bottom of the pelvis. These muscles are called the pelvic floor, and they are used for many everyday activities.
“These muscles are very special. They stabilize your spine, they hold up your internal organs, they help you with pooping, peeing, sexual function, potentially being pregnant and giving birth,” Samms says.
How do you know if you need pelvic floor physical therapy?
Because the pelvic floor has so many different roles, there are many reasons someone might need pelvic floor physical therapy.
Samms says these might include:
- urinary or fecal incontinence
- constipation
- pelvic organ prolapses
- tailbone pain
- anal-rectal pain
- pain with intercourse
- pain during vaginal exams
- sacroiliac joint pain
Because other medical concerns can cause symptoms similar to those caused by pelvic floor issues, patients are often screened for other health concerns before being referred to pelvic floor physical therapy.
“We want to be aware of what's within our wheelhouse but appreciate that it's not just muscles. There are organ systems there. We have to say, ‘Hey, what's really happening?’ with a good thorough interview or an examination,” she says.
What happens during the examination at a pelvic floor physical therapy appointment?
Before a pelvic floor physical therapy appointment at MD Anderson, your provider will review your chart to better understand your situation.
At a patient’s first appointment, Samms says she shares information about the pelvic floor muscles before asking patients questions about any pain they may be experiencing, as well as their bladder, bowel and sexual function.
Then, it is time for a physical exam. This may include an external examination of the pelvis during which the provider lightly touches the region to determine if a patient feels pain or tenderness. This may be followed by an internal examination of the vaginal or rectal canal to determine whether there is any pain, tenderness or restrictions. During an internal examination of the pelvic floor, a provider may ask you to activate, or squeeze, certain muscles to better understand how they are functioning.
From there, Samms works with her patients to create a unique care plan that enhances their quality of life.
Success looks different for every patient: some will measure success by their ability to better control their bladder or bowels, others by their ability to have pain-free intercourse.
“We come up with a very individualized, tailored, thorough plan,” Samms says.
What kinds of exercises are used in pelvic floor physical therapy?
Pelvic floor physical therapy might draw to mind pelvic muscle strengthening exercises such as Kegels, or biofeedback, which uses computers to assess the body while a patient performs exercises.
While Samms notes that Kegels and biofeedback are components of pelvic floor physical therapy, it also includes many other exercises and modalities that can be customized for each patient based on their symptoms and goals.
“Those are just such small tools in the toolbox of a pelvic floor practitioner,” she says.
Pelvic floor physical therapy might also include exercise, muscle strengthening or coordination training.
Additionally, Samms uses pain neuroscience to help her patients better understand pain and the role it plays in protecting the body from harm.
Pelvic floor physical therapy also considers nutrition, sleep hygiene and mental health.
"Pelvic floor physical therapy is really best when it is holistic and takes into consideration partners and we're not working in silos and we're considering the whole mind-body machine,” Samms says.
What is the role of pelvic floor physical therapy in cancer treatment?
There are many reasons someone undergoing cancer treatment may be referred to pelvic floor physical therapy. Patients may have preexisting pelvic floor health issues or only begin experiencing them as side effects from cancer treatment such as chemotherapy, radiation or surgery.
Chemotherapy can affect the bladder and urinary system and lead to urinary incontinence.
Additionally, radiation shortens muscles and connective tissue making it harder for them to move. This can cause urinary incontinence, constipation or pain with intercourse.
Surgery can also impact organs in the pelvis and the pelvic floor. For example, if the prostate is removed during prostate cancer treatment, it can alter the body’s anatomy and lead to urinary incontinence.
“If you remove that prostate from underneath that bladder, that urinary support is no longer there. Whereas you did have a star quarterback for you for urinary incontinence, now you have to use your backup players, which are the pelvic floor,” Samms says.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
What’s new in immunotherapy for prostate cancer?
One of the earliest immunotherapies approved by the Food and Drug Administration (FDA) for the treatment of cancer was a vaccine called sipuleucel-T. It’s been used to treat metastatic prostate cancer since 2010.
Since then, the introduction of immune checkpoint inhibitors has revolutionized the field of cancer treatment. And patients with some types of cancer — such as melanoma and lung cancer — have benefitted greatly from that discovery. Others, including those with prostate cancer, have not benefited as much.
At MD Anderson, we are working hard to understand why, and what can we do to change it.
Few T cells in prostate tumors help thwart immune checkpoint inhibitors
A major reason immune checkpoint inhibitors don’t work as well against prostate cancer is that the gland doesn’t contain a lot of T cells, which do much of the immune system’s heavy lifting when it comes to killing cancer.
Melanoma (a skin cancer) and lung cancers generally have more T cells. So, an immune checkpoint inhibitor, which takes the brakes off of T cells and allows them to keep working, is much less effective in a cancer that doesn’t have many T cells to begin with.
New class of immunotherapy makes the most of existing T cells
But a new class of immunotherapy, called T cell bi-specifics, also known as T cell redirectors, could be changing that. These drugs bind one part of themselves to a tumor cell and the other part to a T cell. Forcing the two cells together has yielded some remarkable results.
A recent clinical trial involving an experimental drug called AMG 509/Xaluritamig, saw a reduction in blood levels of prostate-specific antigen (PSA), a tumor marker, in nearly half of participating patients. A quarter of participating patients whose tumors could be measured saw shrinkage on scans. This drug targets a protein called STEAP-1 on prostate tumor cells and an antigen called CD3 on T cells. Several clinical trials involving that drug are now underway at MD Anderson.
Another just-launched study, led by my colleague Sumit Subudhi, M.D., Ph.D. in collaboration with Brian Chapin, M.D., and me, is providing a unique lens to study these drugs. This clinical trial is using a first-in-its-class drug called REGN5678, which binds the prostate-specific membrane antigen (PSMA) on tumor cells and the CD28 protein on T cells.
Patients with prostate cancer who will undergo surgery will receive the experimental drug for six weeks, then have their prostate glands removed. Analyzing the entire gland will help us understand exactly what the drug is doing, how it’s working and how we might be able to combine it with other drugs in the future, to potentially improve effectiveness.
Learning about new therapy’s side effects
We’re also looking at side effects. Immunotherapies can be very effective at attacking tumors. But they can also sometimes cause unwanted side effects, where the immune system starts attacking the body’s tissues and organs.
As with CAR T cell therapy, the two major side effects of T cell bi-specifics are:
- Cytokine release syndrome (CRS): This causes flu-like symptoms such as high fever, fatigue and body aches in milder cases, and blood pressure problems and other issues in more severe cases. We treat CRS with steroids and a drug called tocilizumab.
- ICANS: This side effect, which stands for immune effector cell-associated neurotoxicity syndrome, makes patients confused or disoriented. They may also temporarily lose the ability to speak. Steroids are the most effective treatment.
As T-cell bi-specific drugs are new, we are also seeing new kinds of immune side effects. But we are actively studying how to find a balance between keeping a good immune response to these drugs and separating it from the unwanted side effects. We monitor the patients receiving these treatments very closely.
Our hope for the future of prostate cancer treatment: the possibility of immune memory
Prostate cancer feeds on testosterone. So, we’ve known for more than 70 years that if we reduce or eliminate testosterone levels using hormone-suppressing drugs, prostate cancer will initially shrink. Unfortunately, prostate cancer often learns how to grow despite the absence of testosterone, making it what’s called “castration-resistant.”
The average lifespan of a patient after a diagnosis of metastatic castration-resistant prostate cancer is two to three years. Approximately 30,000 men die of this disease annually.
So, the possibility of immune memory makes this form of therapy exciting. Immune memory is why vaccines work, and why once you’ve had chicken pox, you won’t get it again. Your immune system learns how to fight off certain threats it’s seen before and destroy them if it ever encounters them again.
If we can successfully harness this therapy’s power to create immune memory for our prostate cancer patients, then they might finally be able to achieve long-term benefits. So, this is a really exciting time to be studying immunotherapy.
Clinical trials for prostate cancer are usually only open to patients who have advanced-stage, metastatic disease. That’s where the need is greatest. But there are also studies for patients who have early-stage prostate cancer with a high risk of recurrence. Talk to your oncologist if you’re interested in enrolling to see if one might be a good option for you.
Bilal Siddiqui, M.D., is a medical oncologist who specializes in the treatment of prostate cancer and other genitourinary cancers.
Request an appointment at MD Anderson online or call 1-877-632-6789.

Prostate-specific antigen (PSA) levels by age: What to know
Prostate-specific antigen (PSA) is a protein made by the prostate, a walnut-shaped gland that’s part of the human male reproductive system. It is located inside the pelvis and wrapped around the urethra, the tube leading from the bladder outside the body that drains urine through the penis.
PSA levels can be measured in the bloodstream, and elevated PSA levels can sometimes be a symptom of prostate cancer. So, this antigen gives doctors a starting point to evaluate your risk of having that disease.
But what constitutes a normal PSA level? Why might your PSA levels be elevated? And, is there such a thing as a “dangerously high” PSA level?
Here are answers to these and three more questions I get asked frequently.
What’s a 'normal' PSA level?
Doctors tend to categorize PSA levels in terms of “elevated” or “non-elevated,” rather than “normal” or “abnormal.” That’s because the range of what’s normal varies by age. Technically, someone with any PSA level can have prostate cancer; that’s not the only thing we look at when assessing a patient.
Generally speaking, though, PSA levels for men who are:
- Age 60 or older: should be at or below 4.0 ng/mL
- Age 59 or younger: should be at or below 2.5 ng/mL
The average PSA for men in the younger group is <1.0 ng/mL.
Why are my PSA levels elevated?
Your PSA levels could be elevated for many reasons. For one thing, the size of your prostate continues to grow as you age, so that can increase the amount of antigen it releases. Other common factors that may cause elevated PSA levels include:
- infection
- prostatitis/inflammation
- a recent urological or pelvic procedure, such as a cystoscopy or a colonoscopy
- medications, especially testosterone replacement therapy
Less common factors that may contribute to elevated PSA levels include:
- sexual activity in the last 1-2 days
- riding a bicycle, which puts pressure on the perineum
These last two are not usually the cause for elevated PSA levels in most men, though. So, urologists will typically recheck levels about a month later to confirm that nothing made them go up temporarily.
Is there a threshold PSA level that requires biopsy?
No. But a PSA above 4.0 in anyone over age 60, or above 2.5 in anyone younger than 60, will likely prompt additional testing.
At MD Anderson, that typically means an MRI. These scans are great, non-invasive ways of determining whether someone needs a biopsy, and, if so, what kind. We now can take samples from very specific areas that look abnormal.
What to know about metastatic prostate cancer
Metastatic prostate cancer is prostate cancer that has spread outside of the prostate to other parts of the body. This is also known as stage IV disease.
At MD Anderson, I treat patients with advanced prostate cancer, most of whom have metastatic disease. A lot of our research is focused on how we can better treat metastatic prostate cancer to improve patients’ results.
Here, I’ll answer common questions I get about metastatic prostate cancer, including what MD Anderson is doing to advance treatment.
Where is prostate cancer most likely to spread?
Prostate cancer often spreads to the bones and lymph nodes. It most commonly spreads to bones in the pelvis or spine. Sometimes it spreads to the ribs.
Over time, prostate cancer can spread to other bones, such as the base of the skull. This is usually a sign of very advanced cancer.
How is metastatic prostate cancer treated?
We’ve known since the 1940s that prostate cancer is a hormone-driven disease. Early studies showed that surgically removing the testes in men, which decreases the body’s testosterone, led to improvement in prostate cancer – temporarily, at least.
While we don’t commonly perform those surgeries anymore, we continue to direct treatment at testosterone, the male sex hormone. Surgery is usually not an option for metastatic prostate cancer. At MD Anderson, we work together as a team of specialists to treat stage IV prostate cancer. Patients may receive:
Hormone therapy
Antiandrogens are medications that block the production of testosterone or stop their interaction with cancer cells.
Chemotherapy
Chemotherapy is often used to treat metastatic prostate cancer by destroying cancer cells.
Radiation therapy
Patients who have painful metastases in their bones may receive targeted radiation therapy to those areas.
Supportive care
We work closely with our Supportive Care team to help patients manage pain during treatment.
What is the survival rate for metastatic prostate cancer?
The average length of survival after a new, metastatic prostate cancer diagnosis is about 5 to 6 years. But it’s important to remember that prostate cancer is not a one-size-fits-all disease. Survival rates are averages. Some patients will live longer than the average, and some will live less than the average. Speak with your doctor about your specific prognosis.
Metastatic prostate cancer goes through two phases, and this impacts the length of survival.
Hormone-sensitive prostate cancer
During this phase, treatments directed toward the testosterone hormones are working well to keep the cancer from growing.
Hormone-refractory prostate cancer
Prostate cancer is smart, and eventually, it learns how to grow without testosterone. This is what we call hormone-refractory, or castration-resistant, prostate cancer. On average, metastatic prostate cancer takes 2 to 3 years to become castration-resistant, but it could be longer or shorter depending on the features of the cancer. Once the disease reaches this phase, average survival is another 2 to 3 years.
What are the latest advances in metastatic prostate cancer treatment?
There is a lot of exciting research happening right now. We’re focusing on identifying specific biomarkers to help us select the right treatment for each patient.
In 2022, the Food and Drug Administration (FDA) approved a targeted nuclear medicine therapy called lutetium Lu 177 vipivotide tetraxetan to treat prostate-specific membrane antigen (PSMA) metastatic castration-resistant prostate cancer. It targets the PSMA protein and delivers radiation to those cancer cells.
We have PSMA PET scans that look for PSMA in cancer cells. If the prostate cancer makes this protein, the patient is a good fit for PSMA-targeted treatment. A Phase III clinical trial showed that patients who received lutetium Lu 177 vipivotide tetraxetan lived longer than those in the control arm who received a different treatment. So, we have a new treatment option to offer patients. Eligible patients receive the treatment as an infusion every six weeks.
At MD Anderson, we’re also conducting clinical trials to study how immunotherapy can help treat prostate cancer. Prostate cancer historically hasn’t seen the same success with immunotherapy as other cancers, like melanoma or lung cancer. We’re hoping to change that.
What’s your best advice for men who’ve been diagnosed with advanced prostate cancer and their loved ones?
I always tell people that one of the key reasons for coming to MD Anderson is the wealth of clinical trial opportunities we offer. Of course, there are pros and cons, but that is a conversation we have with each patient.
If you have been diagnosed with prostate cancer, specifically metastatic prostate cancer, I strongly encourage you to ask your oncologist about clinical trials. Ask them, ‘What’s new in the pipeline? What other options beyond the standard treatment do we potentially have?’
We haven’t cured metastatic prostate cancer yet. But we’re moving in the right direction.
Bilal Siddiqui, M.D., is a genitourinary medical oncologist at MD Anderson who specializes in treating advanced prostate cancer.
Request an appointment at MD Anderson online or call 1-877-632-6789.

What is a total pelvic exenteration?
“Exenteration” refers to a complex surgery in which organs, bones and other structures are removed from the pelvis in order to treat cancer. A pelvic exenteration might involve the bladder, rectum, anus and/or sacrum (tailbone), as well as the prostate gland in men and the vagina and/or uterus in women.
While this procedure may sound fairly extreme, it is often the best — and only potentially curative — option for some types of cancer. It also provides the best possible chance of long-term cancer control.
But which cancers does a pelvic exenteration typically treat? What makes you a good candidate for one? How will it affect your sex life and bathroom habits? And, what else should you know about this life-changing operation? Read on for answers.
Which cancers is a total pelvic exenteration used most frequently to treat?
A total pelvic exenteration (TPE) is most commonly used for locally advanced rectal cancer or another type of cancer that involves the rectum. This is because of the way cancer grows and spreads in the rectum. But TPE is also used to treat:
In fact, pelvic exenteration was originally designed to treat recurrent cervical cancer. It originated as an operation for this gynecologic cancer because the cervix is located in the center of the pelvis. In the days before HPV vaccinations prevented most cervical cancers and radiation therapy was used to treat it, cervical cancer often grew into the structures around it. This procedure was seen as a way of clearing it out.
Are there different types of exenterations?
An exenteration used to treat rectal cancer usually involves the removal of the rectum, plus something else. That could be the bladder, the bone behind the rectum (the sacrum), or any of the other structures surrounding it that are not normally removed during rectal surgery. Generally speaking, though, there are three types of exenterations:
Anterior exenteration
In a male, this entails removing the bladder and the prostate, but leaving the rectum intact. In a female, this involves removing the bladder, uterus and possibly the vagina, but leaving the rectum intact.
Posterior exenteration
This involves the removal of the rectum and sacrum, as well as the uterus (if present) and possibly part of the vagina in a female.
Total pelvic exenteration
In a male, this involves removal of the rectum, bladder and prostate. In a female, this normally entails the removal of the rectum, bladder and uterus (if present) and can also include the vagina.
Which patients make the best candidates for an exenteration?
Ideally, we want you to be at your very fittest before an exenteration. That way, you’ll have some strength in reserve if any complications arise. So, any therapies we might recommend before that are all part of a plan to get your body prepared for surgery, not to help you avoid it.
Your best chance for a cure is when we can do a TPE early as a planned part of your treatment, rather than waiting to do it as a last resort when systemic treatments are no longer working. But a TPE is a long and very complex operation, and the recovery can be prolonged. Not all patients will be able to undergo it. So, the first thing we ask is, “Do you have a cancer that’s resectable?” That is: “Can your tumor be removed with surgery? Then, your surgeon will determine if you are fit enough to undergo it.
Unfortunately, a lot of patients are told elsewhere that this type of surgery is impossible, even when their cancer is not metastatic and is still potentially curable. They only come to MD Anderson after other treatments have failed. Other patients are so leery of the procedure itself that they’ll try almost anything to avoid it.
The trouble is that while chemotherapy and radiation therapy can sometimes slow a cancer’s growth, the problems caused by a locally advanced tumor in the pelvis often become worse. These can include severe pain, obstructions, infections, blood supply problems, and nerve damage. All of those may end up becoming much bigger issues than they would’ve been if someone had gotten the surgery earlier.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention and Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
