- Treatment Options
- Ablation Therapy
- Angiogenesis Inhibitors
- Awake Craniotomy
- Brachytherapy
- Breast Reconstruction Surgery
- CAR T Cell Therapy
- Chemotherapy
- Cryoablation
- High-Intensity Focused Ultrasound (HIFU)
- Histotripsy
- Hyperthermic Intraperitoneal Chemotherapy
- Immunotherapy
- Immune Checkpoint Inhibitors
- Integrative Medicine
- Interventional Oncology
- Laser Interstitial Thermal Therapy (LITT)
- Microwave Ablation
- Minimally Invasive Surgery
- MR-Linac Radiation Therapy
- Palliative Care
- Proton Therapy
- Radiation Therapy
- Radiofrequency Ablation
- Stem Cell (Bone Marrow) Transplantation
- Stereotactic Body Radiation Therapy
- Stereotactic Radiosurgery
- Surgery
- Targeted Therapy
- Theranostics
- Y90 Radioembolization
Stereotactic Body Radiation Therapy (SBRT)
Stereotactic body radiation therapy (SBRT) precisely targets tumors with very high doses of radiation. It is also known as stereotactic ablative radiotherapy and stereotactic ablative body radiation (SABR).
SBRT can cure early-stage cancer by destroying the tumor. It can also shrink tumors, stop the spread of disease and even stimulate the body’s immune system to fight cancer.
It is used against smaller tumors and is often a treatment for lung cancer, prostate cancer and kidney cancer.
Doctors also use SBRT to treat other cancers that have spread, or metastasized, to different parts of the body. This includes oligometastatic disease, in which a patient has just a few metastatic growths. In these cases, SBRT may stop the disease from spreading more and extend the patient’s life.
Patients may choose SBRT instead of surgery in some cases. This lets them avoid a hospital stay, a recovery period and other aspects of surgery. The treatment also may be an option for patients who are not healthy enough for surgery.
One common side effect of SBRT is fatigue. Other side effects depend on the tumor’s location. A patient treated for an abdominal tumor may have gastrointestinal side effects. A patient with a tumor near a bone could experience bone damage.
How does SBRT work?
SBRT uses several radiation beams of different strengths that are aimed at the tumor from various angles.
This requires one or more treatment planning sessions. During these sessions, the patient will undergo a CT scan, MRI and/or other imaging exams. Doctors use these images to map the tumor’s exact location and shape. They then create a customized treatment plan that sets the angles and intensities of the radiation beams.
If the tumor is in or near the lungs the care team will also make a video of the patient breathing. The doctor will use the video to factor motion into the treatment plan. Patients may be asked to hold their breath for short periods while the video is being created and during treatment.
The care team will also make a mold of the patient’s body near the tumor. The mold puts the patient in a position that makes treatment most effective. It also holds the patient still during treatment. This ensures the tumor gets the full dose of radiation. Damage to nearby healthy tissue is minimized.
After planning, patients undergo between one and five SBRT sessions. Sessions take place either once a day or once every other day. Most last about 30 minutes.
SBRT at MD Anderson
Radiation therapy is a pillar of cancer treatment. Some radiation oncologists treat cancers all over the body. Radiation oncologists at MD Anderson focus on specific types of cancer. This gives them incredible expertise when caring for patients.
They use this knowledge when treating patients with SBRT. This treatment can have different goals, from curing patients to stopping cancer’s spread. Knowing what is possible is key to a successful treatment.
Once a goal is set, doctors then develop a treatment plan. Our radiation oncologists are experts in the diseases they treat and SBRT itself. They design SBRT plans to limit damage to nearby healthy tissue while fighting the cancer as much as possible.
Our radiation oncologists also partner with surgeons and medical oncologists who focus on the same cancer. They work together to coordinate care and develop treatment plans tailored to each patient.
And at MD Anderson, patients are surrounded by the strength of one of the nation's top-ranked cancer centers. From support groups to physical therapy to integrative medicine care, we have all the services needed to treat the whole person – not just the disease.
Oligometastatic cancer: What patients with stage IV cancer should know
What does it mean when your cancer has spread? Many patients given a cancer diagnosis of metastatic cancer or stage IV cancer do not know to ask if they qualify for oligometastatic treatments.
Oligometastatic cancers occur when cells from the original tumor travel within the body to one or a few sites forming new tumors. Oligometastatic disease is most common in kidney, lung, prostate and colorectal cancers.
We spoke with radiation oncologist Chad Tang, M.D., who specializes in the care of patients with oligometastatic cancer, to learn more.
What is oligometastatic cancer?
Oligometastatic cancer describes an intermediate stage of cancer between localized and widely spread disease. We classify oligometastatic as a subclass of stage IV cancer. If you have oligometastatic cancer, that means cancer has spread to fewer than five sites in your body.
Historically, radiation therapy was not routinely used to treat stage IV cancers, except to manage symptoms. Instead, patients received drug therapy. This is because while local therapies only target a specific part of the body, drug therapies target the entire body.
We can now see the sites of metastatic cancer with every improving diagnostic imaging. This allows us to target these sites with radiation therapy to delay the spread of metastatic disease for certain cancers.
How are oligometastatic cancers treated?
When cancer has spread, targeted therapy and immunotherapy may be effective. Like chemotherapy, targeted therapy drugs can stop or slow the spread of cancer on a cellular level, including sites of disease we can and cannot see.
Once we determine how many spots of the disease patients with stage IV cancer have, we’re able to determine if the cancer is oligometastatic. Based on that information, we may be able to identify additional treatment options.
What are the most common types of oligometastatic cancers, and how are they treated?
Each of the four common types of oligometastatic cancers is treated a little differently:
- Oligometastatic prostate cancer is treated with systemic therapies, like radiation therapy or hormone therapy. Using radiation therapy gives patients a much longer break from hormone therapy. This can improve quality of life with reduced side effects and decrease cardiovascular risks. If patients experience elevated prostate-specific antigen (PSA) levels, they can start back on hormone therapy.
- Oligometastatic non-small cell lung cancer patients often see long-term benefits from using radiation therapy or surgery after some immunotherapy or chemotherapy.
- Oligometastatic kidney cancer can be treated with stereotactic body radiation (SBRT) and other forms of radiation. It provides a good option for stopping further spread of disease in oligometastatic kidney cancer patients and may allow for prolonged breaks from drug therapy.
- Oligometastatic colorectal cancer occurs when colorectal cancer spreads to other sites in the body. The first site is often the liver. When oligometastatic colorectal cancer is limited to the liver, it’s treated most effectively with SBRT, radiofrequency ablation and surgery.
What clinical trials are available for oligometastatic cancers?
As a leader in treating oligometastatic cancers, MD Anderson has clinical trials for patients who have newly diagnosed, recurrent or progressive diseases.
A recent oligometastatic prostate cancer randomized Phase II study called the EXTernal Beam Radiation to Eliminate Nominal Metastatic Disease (EXTEND) shows metastasis-directed radiation therapy improves progression-free survival and allows for time off hormone therapy. This study provides much-needed data on the benefits of combining these newer radiation techniques with hormone therapy to improve outcomes. EXTEND is also testing metastasis-directed radiotherapy for pancreatic, breast, kidney and other cancers.
A recent oligometastatic kidney cancer clinical trial called the MD Anderson RCC Oligometastasis Phase II trial investigated receiving stereotactic body radiation (SBRT) to delay systemic therapy for oligometastatic renal cell carcinoma (RCC). In this study, investigators offer patients additional courses of radiation therapy if one to three sites of metastatic disease appeared. The strategy of repeated radiation was associated with minimum side effects.
These clinical trials focus on keeping options open for patients with oligometastatic genitourinary cancers by using radiation therapy in an attempt to delay the need for drug therapy. By using radiation therapy first, we can buy our patients some high-quality time. I tell my patients we are taking the drug therapy and putting it in their back pockets to be used when necessary.
What advice do you have for patients with a new oligometastatic cancer diagnosis?
Treating oligometastatic cancers accurately requires a multidisciplinary team. Finding the right care team will connect you with the latest clinical trials, the most innovative ways of identifying disease and delivering local therapy and new targeted therapies.
If your doctor says the cancer is stage IV, ask if it is oligometastatic. If you have a limited number of spots, up to five, ask about local treatment options, such as radiation therapy.
If you are experiencing challenging side effects, talk to your care team. We can help you come up with strategies to cope. Our goal is to turn a terminal diagnosis into a chronic disease.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
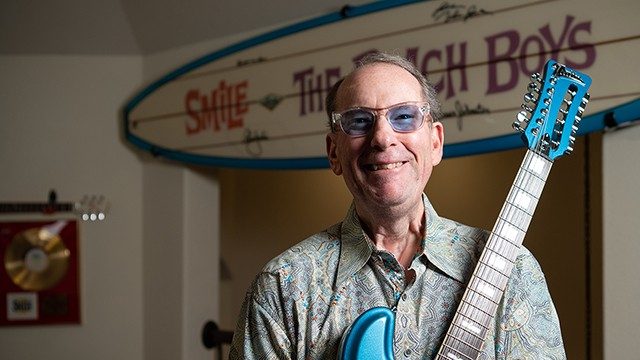
Anaplastic thyroid cancer survivor: I wish I’d gone to MD Anderson first
Everything I have today, I owe to my voice. God granted me a wonderful singing voice at a very young age, and it served me well until I was almost 62. It allowed me to work in the music industry for my entire adult life. And it gave me the opportunity to perform around the world with one of America’s most iconic bands: The Beach Boys.
Three years ago, I underwent thyroid cancer surgery near my home in California. Nerve damage from that surgery paralyzed one of my vocal cords, effectively ending my singing career.
That’s why I’m using my voice today in a different way: to tell people about MD Anderson. Because if it wasn’t for their doctors, I wouldn’t still be here. And I might not have a voice at all.
Life-changing surgery, corrected diagnosis led me to MD Anderson
I came to MD Anderson after the first thyroid surgery changed my life. The realization that I wouldn’t be singing anymore was devastating. But the next bit of news my local doctor delivered was almost worse.
Biopsied tissue revealed that I actually had anaplastic thyroid cancer. And anaplastic thyroid cancer accounts for less than 1% of all thyroid cancer cases diagnosed annually. It’s very aggressive, and there’s no cure.
Unfortunately, my cancer was already fairly advanced. It hadn’t spread to my brain yet, but it had invaded a few of my bones. My local doctors didn’t think I had very long to live. But I wasn’t ready to give up.
Why I joined an immunotherapy clinical trial at MD Anderson
Once we knew I had anaplastic thyroid cancer, my wife and I started researching. The name that kept popping up over and over again was Dr. Maria Cabanillas, an MD Anderson endocrinologist who specializes in anaplastic thyroid cancer.
It turns out, Dr. Cabanillas was conducting a clinical trial with two colleagues — Dr. Naifa Busaidy and Dr. Ramona Dadu — on my exact type of cancer. I was convinced that clinical trial would give me the best possible chance of survival, so I wanted to be on it. Within a week, I was meeting with Dr. Busaidy.
After completing their own examinations and reviewing all of my records and scans, the doctors agreed that I’d be a good candidate for the clinical trial. I joined it right away and started receiving an infusion of an immunotherapy drug called atezolizumab every 14 days and taking two targeted therapy drugs called vemurafenib and cobimetinib in pill form.
I also had stereotactic body radiation therapy to treat the areas in my right hip and breastbone where the cancer had spread.
Six months after I joined the clinical trial, Dr. Mark Zafereo performed a really complex surgery to remove the residual thyroid cancer from my neck and some nearby lymph nodes. It took 12 hours.
Thankful for my three ‘bonus’ years, and any more yet to come
It’s been more than three years now since I joined the clinical trial at MD Anderson. I’m not cancer-free, but most of the suspicious spots on my scans are now stable. So, I consider myself a walking miracle. Because I've survived much longer than my original doctor expected.
I may have lost my singing voice, but that gives me the opportunity now to be a voice for MD Anderson. Had I not lived these three precious “bonus” years, I would not have met my 7-month-old grandson, Domenic. And that’s why I am most grateful.
Join MD Anderson on Thursday, March 24 as we celebrate 80 years of Making Cancer History® with a special anniversary concert featuring musical guests The Beach Boys, Todd Rundgren, Christopher Cross, Generation Radio, the Commodores and more.
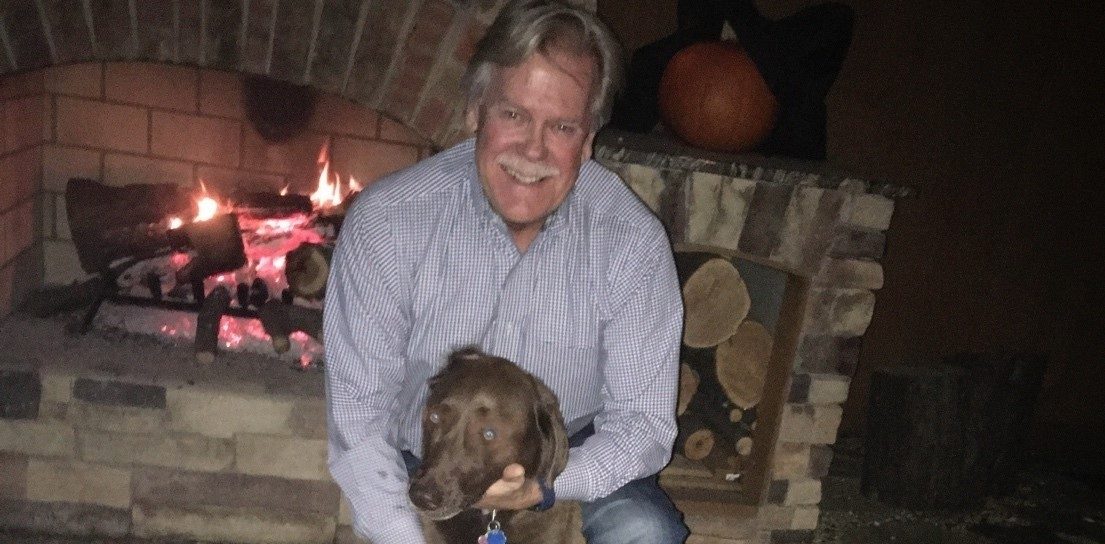
Prostate cancer survivor grateful for stereotactic body radiation therapy (SBRT)
With a family history of prostate cancer, Keith Burchfield did not wait to talk to his doctor about the risks and benefits of early prostate cancer screening.
At his yearly exam, his prostate-specific antigen (PSA) levels had significantly changed since the previous year. There was a 50% chance that he had early-stage prostate cancer. PSA levels show up through a blood test that measures the amount of PSA circulating in the blood. This level is used to assess prostate cancer risk.
Knowing MD Anderson is the top cancer hospital in the nation, he requested an appointment online right away. “I live in the Dallas area and was willing to make the 4-hour drive for the expertise and top treatment options,” says Keith. “I did not want to waste any time.”
Finding expertise and reassurance at MD Anderson
Keith’s first appointment at MD Anderson was scheduled in November 2020, during the COVID-19 pandemic. He met with urologist Justin Gregg, M.D., who ordered an MRI to be done in Dallas so Keith could be close to home.
After the MRI, Gregg confirmed Keith had four lesions. The previous hospital had only detected three. Keith had a biopsy at MD Anderson, then went back to Dallas to wait for his results. Shortly thereafter, Gregg called to let Keith know that the biopsy confirmed he had stage II prostate cancer.
Gregg outlined Keith’s prostate cancer treatment options: surgery, radiation therapy or active surveillance – also known as watchful waiting. “Dr. Gregg answered all my questions with great care. This helped me and my wife, Judy, decide what type of treatment was best for me,” says Keith.
He did not want to postpone treatment by choosing active surveillance. He also didn’t want to face the possibility of side effects from surgery. So, Keith chose radiation therapy. He knew he had a window of opportunity and did not want to wonder if the cancer would become aggressive.
“I was presented with the gift of early detection and wanted to do something as soon as possible,” he says.
Undergoing SBRT for prostate cancer treatment
In February 2021, Keith traveled to Houston to meet with radiation oncologist Karen Hoffman, M.D., and Sarah Todd, her physician assistant at the time.
“Dr. Hoffman and Sarah took the time to explain the types of radiation therapy treatments that I qualified for,” remembers Keith. Each radiation type uses a different number of treatments, either daily radiation for weeks or a short-term radiation for five sessions.
After talking it over with his wife, Keith decided to undergo a short-term radiation therapy called stereotactic body radiation therapy (SBRT). SBRT typically consists of five treatments using a high dose of radiation to treat the tumor’s exact location and shape. A customized treatment plan sets the angles and intensities of the radiation beams.
Keith decided to commute to Houston from Dallas for his five daily SBRT treatments. It happened to be the week of the February 2021 winter storm, an historic winter weather event in Houston resulting in road closures, widespread power outages, loss of heat and broken pipes across Texas.
“I am very thankful that Dr. Hoffman and Sarah are so easy and wonderful to work with. They stayed in continuous communication with me. They made sure I was able to stay on track with my treatments during the bad winter storm – even treating me on a Saturday to make up a missed appointment during the week,” he says.
Keith does not recall experiencing any significant side effects from SBRT. “While every treatment has side effects, I did not notice anything out of the norm from treatment. I had energy to drive back and forth each day,” he says. “And the staff accommodated my travel schedule and arranged my appointments for later in the morning or early afternoon.”
Cherishing every moment after successful SBRT
Three years after treatment, Keith continues to enjoy life after cancer. He meets with Todd every six months to review his PSA levels via a telehealth visit and make sure his prostate cancer stays in remission. In July, he will switch to annual visits.
“My father was diagnosed with stage IV prostate cancer many years ago when they did not have the technology and treatment options available today,” says Keith. “I’m thankful for the advances in radiation therapy.”
Keith is glad he got annual exams to keep an eye on his PSA levels. Most people with stage I or II prostate cancer do not show any symptoms. He tells other men: If you develop prostate cancer and catch it early, you will have more treatment options and a better chance of getting cured.
Not doing active surveillance was an easy decision for Keith. He did not want to have regrets, and he knew the treatment would be more challenging if he was diagnosed with advanced disease.
“Know the prostate cancer warning signs and stay on top of your PSA screenings, especially if you have a family history,” he says. “Early diagnosis is the key to effective treatment.”
Request an appointment at MD Anderson online or call 1-877-632-6789.
request an appointment online.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.

