How does cancer immunotherapy work?
- Treatment Options
- Ablation Therapy
- Angiogenesis Inhibitors
- Awake Craniotomy
- Brachytherapy
- Breast Reconstruction Surgery
- CAR T Cell Therapy
- Chemotherapy
- Cryoablation
- High-Intensity Focused Ultrasound (HIFU)
- Histotripsy
- Hyperthermic Intraperitoneal Chemotherapy
- Immunotherapy
- Immune Checkpoint Inhibitors
- Integrative Medicine
- Interventional Oncology
- Laser Interstitial Thermal Therapy (LITT)
- Microwave Ablation
- Minimally Invasive Surgery
- MR-Linac Radiation Therapy
- Palliative Care
- Proton Therapy
- Radiation Therapy
- Radiofrequency Ablation
- Stem Cell (Bone Marrow) Transplantation
- Stereotactic Body Radiation Therapy
- Stereotactic Radiosurgery
- Surgery
- Targeted Therapy
- Theranostics
- Y90 Radioembolization
CAR T Cell Therapy
Chimeric antigen receptor (CAR) T cell therapy is a type of cellular immunotherapy that changes T cells so they are able to recognize and attack cancer.
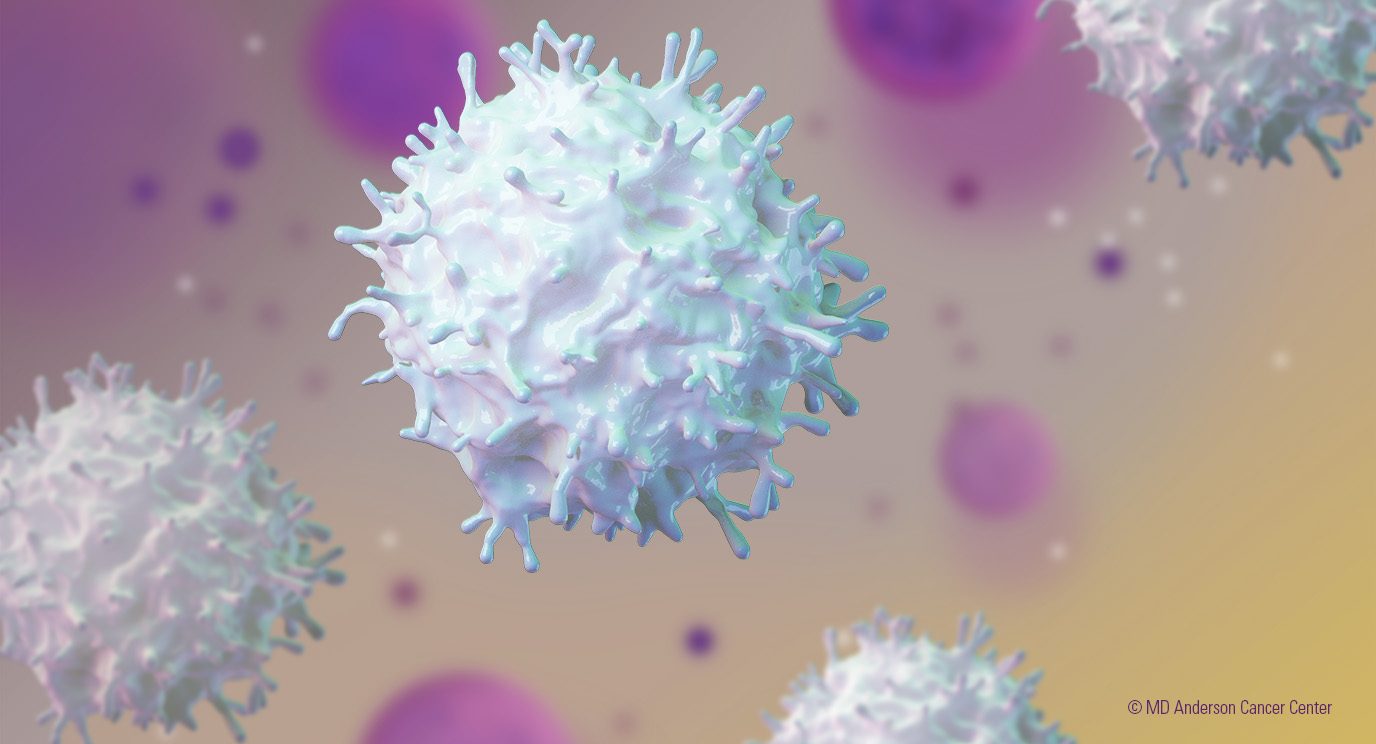
T cells are immune system cells that play several key roles in the body’s fight against disease. They help the immune system respond to disease and directly kill abnormal cells. Unfortunately, naturally occurring T cells in patients with cancer are not good at recognizing and fighting cancer cells.
CAR T cell therapy has been extremely effective in many patients. In some cases, the treatment has eliminated all signs of cancer.
However, CAR T cell therapy doesn’t work for every patient. Some have benefited for a short time before relapsing. Doctors are studying the reasons for these different responses.
How does CAR T cell therapy work?
Several CAR T cell therapies have been approved by the U.S. Food and Drug Administration (FDA). All approved products use T cells taken from the patient. Some clinical trials use T cells taken from donors.
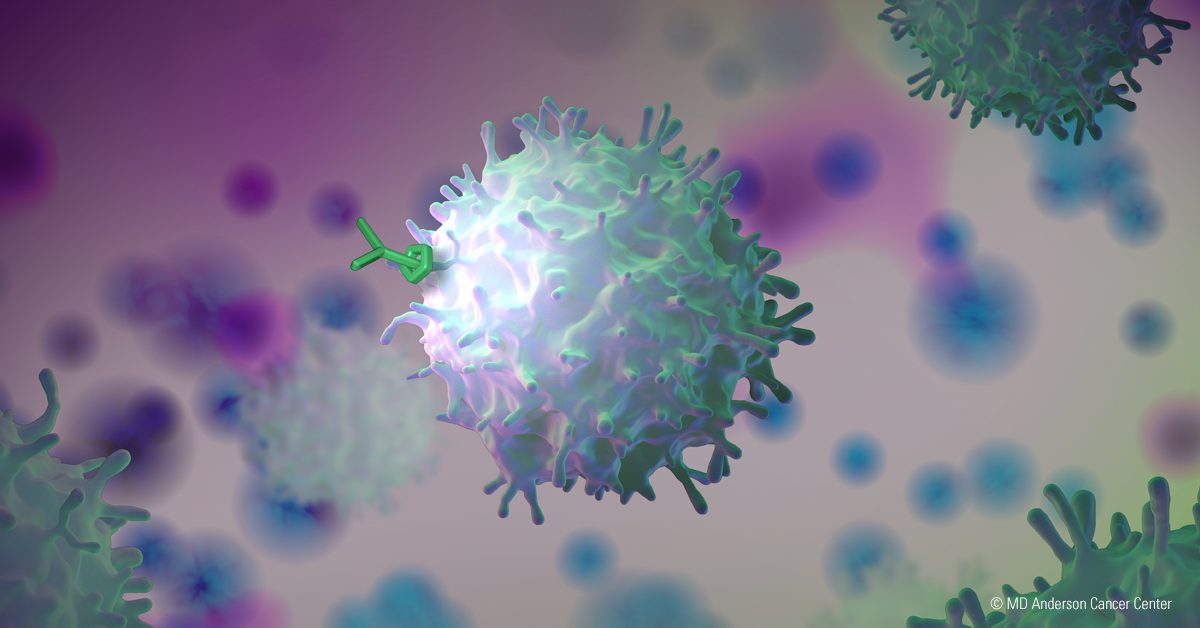
In both cases, the T cells are sent to a lab. There, scientists genetically modify these cells to produce a protein (called a receptor) that recognizes another protein (called an antigen) on the surface of cancer cells. This recognition allows the modified T cells to identify and attack the cancer.
The modified T cells are multiplied by the hundreds of millions and then infused into the patient to fight the disease.
What cancers can be treated with CAR T cell therapy?
There are several different types of CAR T cell therapy produced by different drug companies. FDA-approved CAR T cell therapies treat the following diseases:
- B cell acute lymphoblastic leukemia for pediatric and adult patients
- Certain B cell lymphoma subtypes, including but not limited to:
- high-grade B cell lymphoma
- follicular lymphoma
- primary mediastinal large B cell lymphoma
- Mantle cell lymphoma
- Multiple myeloma
MD Anderson is also conducting CAR T cell therapy clinical trials for a number of other cancers. These include additional subtypes of leukemia and lymphoma; multiple myeloma; and solid tumors such as breast cancer, lung cancer, pancreatic cancer and prostate cancer. Call our CAR therapy line at 833-368-6392 for information on CAR clinical trials.
What is CAR T cell therapy like for patients?
After the T cells are collected, modifying and multiplying them for infusion usually takes a few weeks. Patients may undergo other cancer treatments during this time.
When the CAR T cells are ready for use, they are sent to the hospital for infusion. Before infusion, patients are given a short course of chemotherapy. This weakens their existing immune system, giving the engineered T cells a better chance of expanding and fighting the cancer.
The infusion of the modified T cells is quick, typically lasting less than an hour.
After infusion, patients must remain near the hospital for at least four weeks. Depending on the patient’s type of cancer, condition and specific treatment, this time may be spent as an outpatient or a mix of both inpatient and outpatient. All patients must have a caregiver with them at all times to help care for them and monitor for side effects.
What are the side effects of CAR T cell therapy?
CAR T cell therapy’s side effects can range from mild to serious and even life-threatening if left untreated. Learn more about the side effects of CAR T cell therapy.
Other CAR therapies
CAR T cell therapy is the only CAR-based therapy that has been approved by the FDA. Others are in clinical trials. These include treatments that target more than one antigen on the surface of cancer cells and therapies that use natural killer (NK) cells (another type of immune system cell) instead of T cells. The treatment process and side effects for these therapies are similar to FDA-approved CAR T cell therapies.
Call our CAR therapy line at 833-368-6392 for information on CAR clinical trials.
CAR T Cell Therapy
Accreditation
MD Anderson’s CARTOX Program, which oversees care for the hospital’s CAR T cell therapy patients, is the first stand-alone immune effector cellular therapy program to earn accreditation from the Foundation for the Accreditation of Cellular Therapy.
Interested in CAR T Cell Therapy?
For more information on CAR T cell therapy, CAR clinical trials and how to become an MD Anderson CAR therapy patient, please call 833-368-6382.
Related Care Centers
The following care centers offer or support CAR-based treatments. Additional care centers may be involved in these therapies through clinical trials and as new treatments become available.
Featured Articles

CAR T cell therapy for pediatric patients: What parents should know
Optimizing CAR T cell therapy with bridging radiation therapy
What’s new in CAR T cell therapy? Solid tumor advances

Helping cancer patients navigate CAR T cell therapy
Need CAR T cell therapy? Here’s what to expect

6 things we’ve learned about CAR T cell therapy

CAR T cell therapy put me into complete remission after a non-Hodgkin lymphoma diagnosis

COVID-19 revaccination needed after stem cell transplants and CAR T cell therapy
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.


