request an appointment online.
- Diagnosis & Treatment
- Care Centers & Clinics
- Cancer Prevention Center
Developing healthy lifestyle habits and getting regular screening exams can greatly reduce your risk for some types of cancer.
MD Anderson's Lyda Hill Cancer Prevention Center offers a range of services to help you learn how to reduce your cancer risk or to detect cancer early - when it’s most treatable. Cancer screening exams are based on age, gender and disease risk. We also offer risk assessment, risk reduction and diagnostic evaluation services.
Cancer Screening FAQs
What type of screenings does MD Anderson offer?
MD Anderson offers the following cancer screenings:
- Breast
- Cervical
- Colon
- Liver
- Lung
- Ovarian
- Prostate
- Skin
View information about recommended screenings, as well as a cancer risk assessment.
What are the advantages of coming to MD Anderson for screening?
MD Anderson's Lyda Hill Cancer Prevention Center offers a range of services to help you learn how to reduce your cancer risk or to detect cancer early - when it’s most treatable. Cancer screening exams are based on age, gender and disease risk. We also offer risk assessment, risk reduction and diagnostic evaluation services.
When should I start getting screened?
Cancer screening exams are medical tests done when you’re healthy, with no signs of illness. They help find cancer early, when the chances for successfully treating the disease are greatest. Find out what screening exams are right for you, based on age, gender and family history.
How much will the screening cost and will my insurance cover my visit?
Screening costs vary from insurance to insurance. If you are enrolled in a managed care plan (HMO, PPO or POS), your screening at MD Anderson may be covered by insurance. Check our list of currently accepted insurance plans here. If you don’t see your plan listed or you have insurance questions, call 877-632-6789.
Do you offer genetic testing?
Yes. If you think you might be at risk for an inherited cancer, it's a good idea to meet with a genetics counselor. He or she will review your family medical history, talk to you about the role of genetics in cancer and perform a hereditary cancer risk assessment. This assessment will cover:
- Your chances of having a genetic mutation
- Personalized genetic testing recommendations
- A general estimate of your personal cancer risks
- Individualized cancer screening and prevention recommendations
Contact Us
Hours
Monday through Friday
8 a.m. to 5 p.m.
Phone
713-745-8040 (current patients)
877-632-6789 (new patients)
Our Locations
The Cancer Prevention Center offers care in three locations:
- Duncan Building, Floor 2
- Fannin Tower, 6624 Fannin Street
- Mays Clinic, Floor 8
Get directions to and around MD Anderson on the MD Anderson Directions app, available on the Apple App Store and the Google Play Store.
Cancer Screenings
-
Breast Cancer
A clinical breast exam and screening mammogram can help detect early breast cancers.
-
Cervical Cancer
Human papillomavirus (HPV) testing identifies women at risk of cervical cancer due to an infection with the virus.
-
Colorectal Cancer
Conventional and virtual colonoscopies
-
Prostate Cancer
A digital rectal exam and PSA blood test
-
Skin Cancer
A thorough examination of the skin is performed. A skin biopsy may be performed for suspicious lesions.
-
Lung Cancer
For former and current heavy smokers who meet screening criteria, we offer a low-dose CT scan.
Clinics & Programs
-
Undiagnosed Breast Clinic
Screening and second opinion services are available if you find a lump or have an abnormal mammogram or ultrasound.
-
Undiagnosed Dermatology Clinic
We offer biopsies and head-to-toe evaluations for skin cancer, as well as education on how to reduce your risk.
-
Healthy Living Clinic
Our staff provides detailed guidance on how to reduce your cancer risk through diet and exercise.
MD Anderson Resources
Cancer Screening
Screening exams can find cancer early, when it's most treatable.
Prevention & Screening
8 ways to reduce your cancer risk
Medical physicist: Why I get my cancer screenings at MD Anderson
I’ve never been diagnosed with cancer, but I still get screened at MD Anderson for both breast cancer and skin cancer every year. And I tell everyone I know to do the same.
One reason is that cancer runs in my family. At least five of my relatives have been diagnosed with some type of cancer in the last 15 years.
The second reason is that I have a number of personal risk factors. I’m very fair-skinned and had several severe sunburns as a child.
The third reason is that I work at MD Anderson as a medical physicist in the division of Radiation Oncology. My job is to make sure that radiation therapy is delivered appropriately to our patients. And while my efforts have shifted more toward research now, I did spend several years as a part of our radiation therapy team for breast cancer patients. So, I saw first-hand the difference that early detection can make, both in my patients and among my own family members.
Why I started getting my own skin checked annually
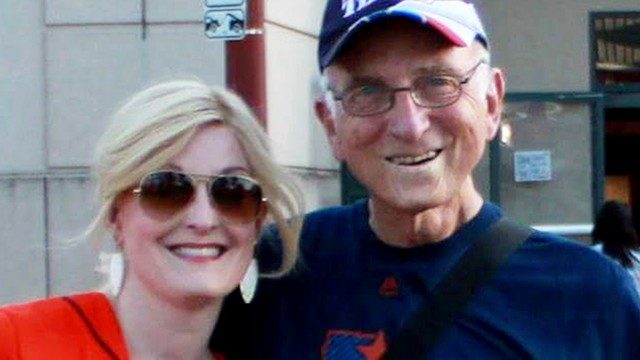
I began getting annual skin checks after my father was diagnosed with a type of skin cancer called squamous cell carcinoma. It was on his lower lip and fairly advanced, so he had a very intense course of radiation therapy to treat it. That kept the cancer at bay for a little while. Unfortunately, it returned a few years later, and required surgery to remove several lymph nodes in his neck and chest, followed by another high-dose course of radiation therapy.
As a result, my father has experienced several treatment-related side effects, including dental cavities, loss of taste, and dry mouth. These have significantly impacted his quality of life. And while both he and my family are obviously happy and very grateful he’s still around to be with us, it’s hard not to think about how different things might be today if his cancer had been diagnosed earlier, when it would’ve required less aggressive treatment.
It’s also really difficult knowing that many of the issues he’s dealing with now — including difficulty chewing, swallowing, eating, and generating saliva — are related not to treatment for an oral cancer or even a throat cancer, but to a skin cancer that has its own prevention protocol.
Why I’ll keep getting my cancer screenings at MD Anderson
I plan to continue getting my screenings at MD Anderson — primarily because it’s the only place I would even consider being treated.
I strongly believe that we are the best place in the world in terms of cancer diagnosis and treatment. So, why would I go someplace different for my screenings? To me, it just makes more sense to have continuity of care. Our cancer prevention and screening teams, including our highly specialized radiologists and pathologists, are exceptional. And our surgical oncology, medical oncology, and radiation oncology teams have unparalleled expertise.
Another way I’m managing my risk factors
I’m also planning to pursue more genetic testing. I want to better understand my risk factors by seeing if I carry any inheritable mutations that might make me more likely to develop certain cancers.
I had genetic testing done more than a decade ago to look for the BRCA mutation, after several relatives were diagnosed with breast cancer. Those results came back negative. But many other markers have since been identified, so I plan to talk with my primary care physician at my next checkup to see if it makes sense to run a new test panel.
Why early detection is so important
So far, I haven’t had anything really worrisome crop up during a mammogram, though I do have very dense breast tissue. That can make it challenging to get clear images, so I have to have an ultrasound-guided biopsy occasionally. And last year, I needed a breast MRI as well as a mammogram.
With skin checks, I haven’t been as lucky. This year, I had to have a precancerous lesion frozen off of my forehead. And last year, I had a larger lesion on my neck that went deep enough to require a minor in-office surgery to remove it completely. Fortunately, the biopsy from that procedure was negative.
Still, I’m very aware that both of these procedures are inconsequential compared to what my dad went through. That’s why genetic marker or no genetic marker, I’m never skipping a cancer screening. Because I know that any cancer detected early is by definition easier to treat. And if you detect skin cancer early enough, its removal is just an office procedure.
Rebecca Howell, Ph.D., is director of Radiation Dosimetry Service and the Late Effects Research Group.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
5 things women should know about cancer screening
When it comes to cancer screenings, some women might think, “Well, I don’t have any symptoms, so I don’t need them.” But that’s actually when you should get them.
Cancer screenings should only be done when you display no symptoms. Otherwise, it’s not a screening test anymore; it’s a diagnostic test. That’s why you shouldn’t wait until you have a lump in your breast or blood in your stool. Because by the time you’re actually showing symptoms, the cancer might not be in its earliest, most treatable stages anymore.
Read on to find out which tests you need and how frequently you should get them, and get answers to other screening questions I often hear at MD Anderson’s Lyda Hill Cancer Prevention Center.
What screenings do I need, and when should I start getting them?
For the average-risk woman (as opposed to those at high risk of developing cancer), we recommend:
- Starting at age 21: A Pap test to check for cervical cancer. If the results are normal, you should be tested every three years. Pap tests are no longer recommended every year for average-risk women of any age.
- Starting at age 30: If you get a Pap test and an HPV test at the same time, and both are negative, you can move to an every-five-year testing schedule. If you only get the Pap test, you should stay on the three-year schedule.
- Starting at age 40: A yearly breast exam and mammogram to check for breast cancer.
- Starting at age 50: A colonoscopy every 10 years, a virtual colonoscopy every five years, or a fecal test (fecal occult blood test [FOBT] or fecal immunochemical test [FIT]) every year to check for colorectal cancer. If you’re African American, you should start this screening process at age 45.
Do I really need all of these screenings? Can’t I delay or put them off?
Yes, you do need them. So, no, you shouldn’t put them off. Women are less likely to die of cancer if they are screened regularly and at the ages specified. Cancer prevention experts selected the recommended starting times and intervals specifically to give doctors the best possible chance of catching cancer early, when it’s the most treatable. A woman’s risk of developing breast cancer, for instance, starts increasing at age 40, so that’s why that age was chosen.
When should I look into my family’s cancer history?
As soon as possible. Having that information available is very helpful, particularly during your first visit, because your family history can change your doctor’s screening recommendations going forward.
For instance, let’s say you’re a woman whose mother was diagnosed with breast cancer at age 45, and her mother -- your maternal grandmother -- was diagnosed with breast cancer at age 52. Because of your mother’s early age of diagnosis, we’d definitely want to talk to you about genetic testing.
We’d also consider you “high risk,” which would mean that we would start your screenings 10 years earlier than the age the youngest person in your family was when they were diagnosed with cancer. We’d probably recommend you start getting breast MRIs, too, on an alternating six-month schedule with mammograms. And we’d talk to you about preventive medications such as tamoxifen, a drug that can cut your chances of developing breast cancer in half.
Should I be tested for inheritable cancer syndromes?
Not necessarily. Genetic testing is most informative when it’s done on someone who actually has the disease. So, in the above scenario, we’d want to talk to your mother first about getting tested. If she is unavailable or unwilling to be tested, and your grandmother is no longer alive, you could be tested for genes that increase the risk of breast cancer.
The reason for this is a negative test result is not considered a “true” negative in a patient who doesn’t actually have cancer, because we haven’t identified the potential cause of the breast cancer in your family. But if your mother’s test is negative, then that is considered a “true” negative; it also means you couldn’t have inherited a genetic mutation that causes cancer from her.
Why should I come to MD Anderson for my cancer screenings?
First, because you’ll be seeing clinicians whose sole focus is cancer prevention. That is all they do -- all day, every day -- so they are the experts. When seen for evaluation, you will have your risk of developing cancer assessed, be counseled regarding a healthy lifestyle as well as other ways to reduce cancer risk (e.g., medications), and receive screening recommendations based on your individualized cancer risk.
Expertise in cancer prevention does not just apply to the clinicians you’ll see, but also to the nurses who have the knowledge to address your cancer concerns, breast imaging technologists who have unparalleled expertise to perform your mammogram, and breast radiologists who have fellowship training in interpreting images of the breast.
At MD Anderson’s Cancer Prevention Center, we see high-risk women multiple times every day; the average physician may see only a few in their entire career. And while some other hospitals do have dedicated breast imaging specialists, in most imaging facilities, the radiologist who’s looking at your mammogram is also looking at chest X-rays, back MRIs, and brain CT scans, among other things. So, they’re not specialized in looking at mammograms or other images of the breast, like our dedicated breast imagers are.
But the best reason to come to MD Anderson for cancer screenings is that we make recommendations women don’t often get elsewhere. For instance, it used to be that women had never even heard of -- much less been asked about -- genetic testing before they came to see us. It’s a bit more common now, but still not universal. Studies suggest that as many as 50% of women who should undergo genetic testing never receive a recommendation to do so. They are more likely to get this recommendation if seen at MD Anderson.
Women at increased risk of breast cancer -- whether due to a breast cancer gene mutation, a family history of the disease or a personal history of a high-risk breast lesion -- typically do not receive a recommendation from their primary care doctor for high-risk screening with breast MRI. If eligible, we commonly recommend high-risk screening with breast MRI.
Many women are also not told about medications like tamoxifen that can reduce their risk of breast cancer, which we might recommend based on their personal risk factors. We also offer our patients opportunities to participate in research studies that advance cancer science. In fact, one clinical trial is looking at the effectiveness of applying tamoxifen gel to the surface of the breast. It may or may not show the same benefit as taking that drug in pill form, but if it does, participating women are receiving cutting-edge therapy right now that may also reduce their side effects.
Therese Bevers, M.D., is medical director of MD Anderson’s Cancer Prevention Center.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.