request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Colorectal Cancer
Colorectal cancer forms in either the colon, a five-foot section of the large intestine, or the rectum, which connects the colon to the anus and holds waste, called stool, before it is expelled.
Colorectal cancer forms in either the colon, a five-foot section of the large intestine, or the rectum, which connects the colon to the anus and holds waste, called stool, before it is expelled.
Colon cancer and rectal cancer start the same way and share many risk factors and symptoms. The two are often referred to together as colorectal cancer. There are some significant differences between them, though.
Colon cancer that has not spread to distant parts of the body is usually treated with surgery, if feasible. If surgery is performed, doctors determine whether the patient needs additional treatments like chemotherapy.
Rectal cancer that has not spread to distant parts of the body is also treated with surgery. For some patients, radiation therapy and chemotherapy are used to decrease the risk of the cancer returning after treatment. In some cases, radiation therapy and chemotherapy can reduce the need for surgery. Rectal cancer surgery can be more complex than colon cancer surgery.
How does colorectal cancer start?
Colorectal cancer usually starts as a polyp. Polyps are small overgrowths in the tissue lining the colon or rectum. Polyps are not cancer.
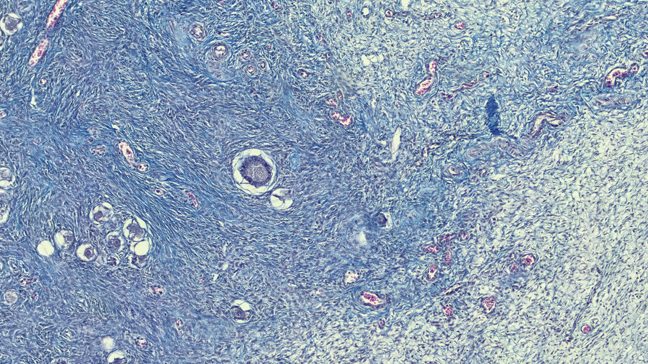
Some polyps can turn into cancer over time. Most of these polyps are adenomas, which begin in mucus-producing gland cells that line the intestine and other organs. Adenomas are considered pre-cancerous growths.
It can take several years for an adenoma to develop into cancer. When it does, the cancer is called adenocarcinoma. This is the most common type of colorectal cancer.
There are other, rarer types of colorectal cancer, including colorectal neuroendocrine tumors and rectal cancers that involve the cells of the anus.
There are more than 150,000 colorectal cancer diagnoses in the U.S. each year. As of 2018, the disease’s five-year survival rate is about 65%. This figure does not include people diagnosed more recently, who could benefit from new treatments.
Colorectal cancer symptoms
Colorectal cancer usually starts in small polyps (overgrowth of tissue) in the colon or rectum. These polyps may not produce any symptoms, especially in the early stages. As the disease progresses, more symptoms may appear.
Symptoms of colorectal cancer may include:
- Diarrhea or constipation that does not go away
- Change in normal bowel habits, such as size, shape and frequency
- Discomfort or the urge to have a bowel movement when there is no need
- Discomfort or pain during bowel movements
- Discomfort when sitting
- Abdominal pain or cramping pain in your lower stomach
- Bloating or full feeling
- Change in appetite
- Rectal bleeding
- Blood in the stool or toilet after a bowel movement
- Excessive fatigue
- Weight loss without dieting
In the later stages of colorectal cancer, the polyp may metastasize (spread) to other parts of the body. This can cause other symptoms, depending on where cancer has spread.
These symptoms usually do not mean you have colorectal cancer. However, any time you notice unexplained changes and they persist for more than two weeks, don’t assume they will just go away. See your doctor.
Young-onset colorectal cancer
Historically, most cases of colorectal cancer have been in people over age 55. In recent years, there has been an increase in diagnoses among people under age 55. MD Anderson’s Young-onset Colorectal Cancer Program offers specialized services for these patients. Services include fertility care, genetic testing and counseling, as well as support groups for young adults.
Colorectal cancer screening
Most precancerous polyps produce few, if any, symptoms. It is important to get screened regularly for colorectal cancer. Colorectal cancer screenings allow doctors to find and remove polyps before they turn into cancer. Screening can prevent most cases of colorectal cancer. It can also catch colorectal cancer early, when treatments are more likely to be successful.
- Learn more about colorectal cancer screenings
Colorectal cancer risk factors
Anything that increases your chance of getting colorectal cancer is a risk factor. Colorectal cancer risk factors include:
- Age: More than 75% of colorectal cancer cases are diagnosed in patients age 55 and older. The median age at diagnosis is 66 years old. However, the rate of colorectal cancer diagnosed in adults less than 55 years old has increased in recent years.
- Race: African Americans have the highest rate of colorectal cancer among all racial groups in the United States.
- Family history: People whose relatives have had colorectal cancer or colorectal polyps have an increased risk of colorectal cancer.
- Inflammatory bowel disease: Patients with conditions that include Crohn’s disease or chronic ulcerative colitis are more likely to develop colon cancer. Learn more about inflammatory bowel disease and colorectal cancer.
- Personal history of colorectal cancer or polyps: People who have previously had colorectal cancer or colon polyps are at an increased risk of developing colorectal cancer.
- Hereditary cancer syndromes: Some genetic changes can be inherited and increase your risk for certain types of cancer. Inherited syndromes including hereditary nonpolyposis colorectal cancer, or Lynch syndrome, and familial adenomatous polyposis may put you at higher risk for developing colorectal cancer. Learn more about hereditary cancer syndromes.
- Diet: A diet heavy in red meat, processed meats, or meats cooked at very high heat can increase a person’s colon cancer risk.
- Obesity: Obesity increases a person’s chance of developing many different diseases, including colorectal cancer.
- Sedentary lifestyle: A lack of movement and exercise is a risk factor for colorectal cancer.
- Tobacco: Tobacco use, including cigarettes and chewing tobacco, is a colorectal cancer risk factor.
- Drinking too much alcohol: Heavy drinkers are at an increased risk for colorectal cancer.
For patients concerned about inherited family syndromes that cause colorectal cancer, we offer advanced genetic testing and counseling to help understand your risk.
Colorectal cancer prevention
Lifestyle choices that may decrease your risk of getting colorectal cancer include:
- Regular screening tests
- Staying at a healthy weight
- Regular exercise
- Eating a healthy diet with lots of fruits and vegetables
- Avoiding cigarette smoking
- Drinking alcohol only in moderation
Learn more about colorectal cancer:
Learn more about clinical trials for colorectal cancer.
MD Anderson is #1 in Cancer Care
Colorectal cancer screening: At what age should I get a colonoscopy?
Colorectal cancer screening can detect cancer early, giving you the greatest chance for successful treatment. While colonoscopy is the gold standard for colorectal cancer screening, you may be wondering when you should get your first test.
We spoke with gastroenterologist Mazen Alasadi, M.D., about the recommended age for colonoscopies.
Most people should get their first colonoscopy at age 45
Current guidelines suggest that you should get your first colonoscopy at age 45 if you are at average risk for colorectal cancer. If no polyps are found during your initial colonoscopy, then you wouldn’t need your next colonoscopy for another 10 years.
Regular screenings are recommended from age 45 through 75.
High-risk groups should start screening earlier
Individuals at higher risk for colorectal cancer should begin getting a colonoscopy earlier than age 45.
If you have a first-degree relative (e.g., parent or sibling) with a history of colorectal cancer, you should get your first colonoscopy at age 40, or 10 years younger than the age at which the family member was diagnosed, whichever is earlier.
Other groups who may need a colonoscopy sooner include those with:
- inflammatory bowel disease or
- inherited genetic changes, such as Lynch syndrome and familial adenomatous polyposis (FAP). Colonoscopy screening for people with FAP can begin as early as age 10.
Consult your doctor about colorectal cancer screening after age 75
While colonoscopies are still recommended for some people older than 75, speak with your doctor to determine if you should continue colorectal cancer screening after age 75.
Your body changes as you age, and for some people, a colonoscopy after age 75 isn’t recommended.
“Having a colonoscopy at age 45 is different than having one at age 75,” says Alasadi. “We consider it on a case-by-case basis.”
For example, some individuals over age 75 want to have another colonoscopy because their doctor found precancerous polyps during their previous colonoscopy. Or a patient could have a family history of colorectal cancer.
Or maybe you’ve begun to develop colorectal cancer symptoms.
“Let’s say you’ve been doing fine and suddenly at age 76, you begin to notice blood in your stool,” says Alasadi. “We don’t know if this could be related to hemorrhoids, diverticulosis or colorectal cancer. We might recommend a colonoscopy, so we can determine the cause of the bleeding.”
Older patients are also more likely to have comorbidities, meaning they have two or more diseases or medical conditions at the same time. For example, a patient older than 75 with heart disease, high blood pressure, diabetes and on blood thinners would need to disclose these conditions as well as current medications to their doctor.
“If a patient is on blood thinners, they have to stop taking that medication before receiving a colonoscopy,” says Alasadi. “I always get this cleared by the patient’s cardiologist or hematologist before the procedure.”
There’s also a greater risk to older people while undergoing anesthesia, so it’s important to consider the anesthesia administered during a colonoscopy.
“We always discuss the risks and benefits of the colonoscopy with each patient,” says Alasadi. “Once we explain all of these things, the patient signs a consent form before we proceed with the colonoscopy.”
MD Anderson doesn’t recommend colorectal cancer screening for people older than 85.
“If you don’t have any more problems or symptoms, you don’t need to have any more colonoscopies,” says Alasadi.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
What are the risk factors for colorectal cancer?
Colorectal cancer is a type of cancer that develops in the colon or the rectum. It is the fourth most common cancer diagnosed in the U.S.
Here, I’ll discuss what makes you more likely to develop colorectal cancer and what you can do to lower your risk.
What are colorectal cancer risk factors?
Several things can increase your chances of getting colorectal cancer. These risk factors include:
Age
Most people diagnosed with colorectal cancer are older than 50. However, in recent years, we have seen a rise in colorectal cancer cases in young adults.
Family history
If you have a first-degree relative (e.g., parent, sibling or child) with a history of colorectal cancer or colorectal polyps, you are more likely to develop colorectal cancer.
Hereditary cancer syndrome
Some people inherit genetic changes that increase their risk for colorectal cancer. The most common hereditary cancer syndromes linked to colorectal cancer are Lynch syndrome and familial adenomatous polyposis (FAP).
Up to about 20% of colorectal cancer patients under age 50 may have a hereditary cancer syndrome. We recommend genetic counseling and genetic testing for these patients.
Obesity
Individuals with a body mass index (BMI) that is above average have a higher chance of developing many diseases, including colorectal cancer. A healthy BMI is 19-24.
Tobacco use
If you use tobacco, including smoking cigarettes and chewing tobacco, you’re more likely to develop colorectal cancer.
Diet
Eating a lot of red meat, processed meat and grilled/charred meat can increase your risk for colorectal cancer.
Inflammatory bowel disease
You have a much greater risk for colorectal cancer if you have a history of inflammatory bowel disease, like Crohn’s disease or ulcerative colitis.
Race
Black men and women have the highest rate of colorectal cancer among all racial groups in the U.S.
Personal history of colorectal cancer or colorectal polyps
If you’ve had colorectal cancer or colorectal polyps before, you’re more likely to develop colorectal cancer. The number of polyps and type of polyps can help determine what your future colorectal cancer risk may look like.
Heavy alcohol use
If you drink a lot of alcohol, that can raise your risk for colorectal cancer. While no alcohol is best, women who choose to drink should have no more than one drink a day, and men no more than two drinks a day.
Lack of physical activity
A sedentary lifestyle increases the risk of colorectal cancer. Staying active throughout the day and getting regular exercise can help lower your risk for colorectal cancer and other diseases. Aim for at least 150 minutes of moderate exercise, like brisk walking, or 75 minutes of vigorous exercise, like running, each week.
What is a high-risk feature for colon cancer?
We often use the phrase “high-risk feature” when talking about the prognosis for stage II and stage III disease. High-risk features are things pathologists look for on colon cancer tumors that help us identify if there is a high risk for relapse, or the cancer coming back. The size of the tumor is one example of a high-risk feature.
For example, a person with stage II colon cancer may have tumors with high-risk features that make the cancer more likely to relapse compared to another person with stage II disease with tumors that do not have these features.
How can you lower your colorectal cancer risk?
There are several things you can do to help decrease your risk of getting colorectal cancer. These include:
Get regular colorectal cancer screenings
Colorectal cancer is preventable and easier to treat when it’s found early. Colonoscopy is considered the gold standard for colorectal cancer screening, but other tests are available.
It’s important to get your first colonoscopy at age 45 if you’re at average risk for colorectal cancer, and then every 10 years after that, if no polyps are found.
During a colonoscopy, doctors can remove precancerous polyps so that they don’t turn into cancer later on. Additionally, screening tests can find colorectal cancer early, when it’s easier to treat.
Check with your doctor to determine when and how often you should get screened. People at higher risk for colorectal cancer often need to start screening earlier and be screened more frequently.
Make healthy lifestyle choices
A healthy diet and regular exercise can help lower your chances of developing colorectal cancer.
Eat meals rich in whole grains, vegetables, fruits, beans, nuts and seeds. Limit red meat, processed meat and meat cooked at high temperatures.
Regular physical activity can help you maintain a healthy weight, which can reduce your risk for colorectal cancer.
For cancer prevention, it’s best not to drink alcohol. If you stop drinking, the risk of alcohol-related cancer declines over time.
If you use tobacco, stop. There are resources to help you quit, including MD Anderson research studies.
While there are certain factors that can increase your risk for colorectal cancer, remember: there are steps you can take to lower your risk and find the disease early.
Jason Willis, M.D., Ph.D., is a gastrointestinal medical oncologist at MD Anderson.
Request an appointment at MD Anderson online or call 1-877-632-6789.
Mother and son survivors share inspiration, passion for cancer prevention
William Lindley has been watching his mother, Faye Wright, deal with cancer for more than 25 years. He was only a teenager when she was diagnosed with stage IV adenoid cystic carcinoma (ACC) in her right breast. This rare head and neck cancer usually appears in the salivary glands.
Since then, William has seen his mother face three different recurrences. He’s also watched her undergo radiation therapy and multiple major surgeries to keep the cancer at bay.
Now, he is drawing inspiration from his mother’s experiences as he faces his own stage IV colorectal cancer diagnosis.
“In a weird way, it’s been a blessing to see her navigate it,” William says. “Her journey was so rigorous, but she’s a strong woman and a warrior. I knew if she could do it, I could do it.”
Faye also draws strength from her son. “It’s been hard to watch him suffer,” she admits. “But it’s so inspiring to see him come through it. I consider it a blessing that we’re experiencing this together.”
Coincidences and choices led to cancer treatment at MD Anderson
Though no common thread or genetic mutation links their diseases, both William and Faye learned that they had cancer at the same time of year and when they were about the same age. William had turned 38 a few months before his diagnosis in January 2022, while Faye was 39 at the time of her diagnosis in January 2000.
Both deliberately sought treatment at MD Anderson: William from gastrointestinal medical oncologist Christine Parseghian, M.D., and his mother from orthopedic surgical oncologist Valerae Lewis, M.D.
“I told William he would meet some of the most important people in his life at MD Anderson,” recalls Faye. “Nobody knew what to do about adenoid cystic carcinoma near our home in Mississippi. But Dr. Lewis has given me the best possible outcome with every surgery. I can still do anything I want to now, except maybe run. And, I’m still here, 25 years later. So, I really can’t say enough good things about MD Anderson.”
Learning from each other
Before William’s cancer diagnosis, the most important advice his mother ever gave him was to listen to his body. That’s what finally prompted him to investigate the change in bowel habits that was making his job in law enforcement difficult.
“I was having to go to the bathroom quite a bit,” William recalls. “Otherwise, I was pretty healthy. So, I tried to dismiss my symptoms as irritable bowel syndrome. Eventually, I had to do something about it. So, I tell everyone now to pay attention and advocate for themselves. You’re the only person who truly knows what’s going on inside of you.”
After each of William’s surgeries, Faye also advised him to become active as quickly as possible, so that he would heal faster. “Don’t just sit there,” he recalls her saying. “Get up and start walking.”
Faye, meanwhile, has started eating healthier, inspired by the dietary changes she’s watched her son and his family make to reduce his risk of the cancer coming back. “He’s been a lot faster on the lifestyle stuff than I have,” she admits. “So, I’m actually learning from him these days.”
Paying it forward
William has shown no evidence of disease since January 2025. Faye is currently exploring treatment options for a small new cluster of tumors discovered recently beneath her right breast. But both are determined to keep spreading the word about body awareness and prevention.
William’s diagnosis has already led four of his colleagues to get colorectal cancer screenings. Another is about to have a colonoscopy.
“It’s great to know that my journey is helping others,” says William.
“I was too young to have regular screening mammograms at the time of my diagnosis,” adds Faye. “But you can bet that I started getting them afterward. Now, I get so many scans per year that it would be hard for something to slip by. Still, I don’t put anything off. If a screening protocol exists for a particular disease, I get checked out as soon as I can. And, I tell everyone else to do the same.”
Request an appointment at MD Anderson online or call 1-877-632-6789.
Diagnosis & Treatment
Diagnosis
Colorectal cancer can be identified during a routine screening. Everyone with an average risk for colorectal cancer should start getting regular colorectal screenings starting at age 45.
People who have symptoms of colorectal cancer should be tested regardless of their age. This is considered a diagnostic test.
The following tests may be used as screening and/or diagnostic tests for colorectal cancer. They can also show if the cancer has spread and monitor how the disease is responding to treatment.
Endoscopic screening and diagnostic tests
Endoscopic tests are the most effective tests for colorectal cancer. They can be used for routine screening that everyone should have starting at age 45. They are also used for patients who have colorectal cancer symptoms and need a diagnostic test.
These tests generally are performed under some form of sedation so that you do not feel any discomfort. Endoscopic tests allow your doctor to see the inside of your colon clearly.
Endoscopic tests may include:
- Colonoscopy: A tiny camera on flexible plastic tubing (colonoscope) is inserted into the rectum and advanced through the colon. This gives the doctor a view of the entire colon. Colonoscopies are used for routine screening and to diagnose people with colorectal cancer symptoms.
- Sigmoidoscopy: Sigmoidoscopy is similar to colonoscopy but is a shorter examination of the rectum and lower colon. It is used to monitor people with confirmed cases of cancer in the rectum or the last section of the colon. By examining just the rectum and lower colon, doctors can track the disease’s progress and how it is responding to treatment. A sigmoidoscopy combined with a stool-based test can also be used for routine colorectal cancer screening.
Biopsy: If doctors remove any polyps during a colonoscopy, they will be examined under a microscope for the presence of cancer cells. The process of removing and examining suspected disease tissue is called a biopsy.
At-home screening tests
There are several types of non-invasive colorectal cancer screening tests that can be taken at home. These do not provide a definitive diagnosis for colorectal cancer, but they can indicate that other, more accurate tests should be used. They are typically not offered to patients who have symptoms of colorectal cancer and are referred for a diagnostic test.
There are several types of at-home screening tests, including:
- Fecal DNA test (FDNA), which identifies DNA changes in the cells of a stool sample
- Fecal immunochemical test (FIT), which identifies blood proteins in stool
- Fecal occult blood test (FOBT), which identifies blood in the stool
Additional diagnostic tests
If you have symptoms of colorectal cancer, or if you have an abnormal screening test result, your doctor may recommend additional tests. These tests may include:
Blood tests: At present, no blood test can definitively diagnose colorectal cancer. However, they can provide your doctor with additional information.
- Standard blood tests can provide information about kidney and liver function and blood counts.
- A blood test for the carcinoembryonic antigen (CEA) protein, made by some tumors, can reveal if the tumor is growing, responding to treatment, or has come back after treatment.
- Patients who have been successfully treated for colorectal cancer can be tested for circulating tumor DNA (ctDNA). This test can help catch recurring cancer early, before it shows up in an imaging exam.
Imaging tests: Imaging tests can help to provide detailed information about the size or location of colorectal cancer and if it has spread to other parts of the body. Common imaging tests are:
- CT scan: A computed tomography, or CT, scan uses an X-ray machine to take several pictures from different angles, providing a highly detailed image.
- MRI scan: Magnetic Resonance Imaging, or MRI, uses magnetic fields and radio waves to generate pictures of the body’s soft tissue and organs. MD Anderson offers a specialized type of MRI used specifically to evaluate and help plan care for rectal cancer patients.
- PET/CT (positron emission tomography) scan: PET/CT scans are not routinely part of colorectal cancer diagnosis. They are generally used to further evaluate abnormal findings on CT or MRI scans or to monitor patients who have a confirmed case of advanced colorectal cancer.
Learn more about imaging tests.
Colorectal cancer testing can also include these other tests, which are used less often:
- Virtual colonoscopy or CT (computed tomography) colonoscopy: A focused CT scan of your abdomen and pelvis to create 3D images.
- Endoscopic ultrasound (EUS) or endosonography: A flexible tube with an ultrasound device attached to the tip is inserted through the rectum into the colon. The device sends out ultrasound waves to generate images of the colon and nearby tissue.
- Double contrast barium enema (DCBE): Barium is a chemical that allows the bowel lining to show up on an X-ray. A barium solution is given by enema, and then a series of X-rays are taken.
Treatment at MD Anderson’s Gastrointestinal Center combines the latest technology and research with a multidisciplinary team approach tailored to your unique needs.
Our team of surgeons use minimally invasive techniques, including advanced robotic surgery, that reduce recovery time and maximize quality of life. MD Anderson also offers clinical trials for patients at every disease stage, from newly diagnosed small tumors to patients with stage IV cancer.
Treatment
Treatment at MD Anderson’s Gastrointestinal Center combines the latest technology and research with a multidisciplinary team approach tailored to your unique needs.
Our team of surgeons use minimally invasive techniques, including advanced robotic surgery, that reduce recovery time and maximize quality of life. MD Anderson also offers clinical trials for patients at every disease stage, from newly diagnosed small tumors to patients with stage IV cancer.
Colorectal cancer treatment plans
Colon cancer that has not spread to distant parts of the body is usually treated with surgery. Some patients then receive chemotherapy or, less commonly, radiation therapy to kill any remaining cancer cells.
Rectal cancer that has not spread is usually treated with surgery. These patients may receive chemotherapy or radiation therapy before the procedure. They may also undergo these treatments after surgery to kill any remaining cancer cells.
If colorectal cancer has spread, or metastasized, to distant parts of the body, some patients can still be cured. With new treatments, colorectal cancer that has spread can often be managed like a chronic condition and care is meant to prolong life and preserve quality of life. Treatments for all patients with metastatic colorectal cancer can include surgery, radiation therapy, cryotherapy, microwave ablation, and cancer drugs like chemotherapy, targeted therapy and immunotherapy.
Surgery
Surgery is the most common treatment for colorectal cancer, especially if it has not spread. Surgery for colorectal cancer is most successful when done by a surgeon with a great deal of experience in the procedure. At MD Anderson, these procedures are performed by surgeons who specialize in colorectal cancer surgery and are national and international leaders in the field. Surgeons around the country often refer their patients to MD Anderson surgeons for their expertise, especially for the most difficult cases.
The type of surgery depends on the stage and location of the tumor. Visit the colon cancer treatment page or rectal cancer treatment page to learn about the surgical procedures for each disease.
Chemotherapy
Chemotherapy drugs kill cancer cells, control their growth or relieve disease-related symptoms. Chemotherapy may involve a single drug or a combination of two or more drugs, depending on the type of cancer and how fast it is growing.
Targeted Therapy
Targeted therapy drugs are designed to stop or slow the growth or spread of cancer. This happens on a cellular level. Cancer cells need specific molecules (often in the form of proteins) to survive, multiply and spread. These molecules are usually made by the genes that cause cancer, as well as the cells themselves. Targeted therapies are designed to interfere with, or target, these molecules or the cancer-causing genes that create them.
Radiation therapy
Radiation therapy uses powerful, focused beams of energy to kill cancer cells. There are several different radiation therapy techniques. Doctors can use these to accurately target a tumor while minimizing damage to healthy tissue.
Radiation therapy is frequently used to treat rectal cancer. For colon cancer, it is used only in very limited situations.
Cryoablation
Cryoablation, also known as cryotherapy or cryosurgery, uses cold to kill tumor cells. During the procedure, a special probe is inserted into the tumor and then cooled to temperatures well below freezing. A ball of ice forms at the tip of the probe, freezing and destroying cancerous tissue. Cryotherapy is not as invasive as surgery and can sometimes be performed as an outpatient procedure.
Microwave ablation
Microwave ablation uses heat to kill cancer cells. During the procedure, a probe delivers microwaves directly to the tumor, heating the tissue until it is destroyed. Microwave ablation is not as invasive as surgery and can sometimes be performed as an outpatient procedure.
Immunotherapy
The immune system finds and defends the body from infection and disease. Cancer is a complex disease that can evade and outsmart the immune system. Immunotherapy improves the immune system’s ability to eliminate cancer.
There are two types of immunotherapy currently used to treat colon cancer:
- Immune checkpoint inhibitors stop the immune system from turning off before cancer is completely eliminated.
- Monoclonal antibodies attach to specific proteins on the surface of cancer cells or immune cells. They either mark the cancer as a target for the immune system or boost the ability of immune cells to fight the cancer.
Angiogenesis inhibitors
Angiogenesis is the process of creating new blood vessels. Some cancerous tumors are very efficient at this process. New blood vessels increase blood supply to a tumor, allowing it to grow rapidly. Angiogenesis inhibitors, or anti-angiogenic therapy, disrupt the creation of these blood vessels.
Clinical trials
Clinical trials are a key component of MD Anderson's mission to end cancer. Patients may volunteer to participate in these research studies, which help doctors improve cancer prevention, diagnosis and treatment.
Some clinical trials allow patients to receive experimental medications or treatments, though not all patients are eligible.
Why choose MD Anderson for your colorectal cancer treatment?
At MD Anderson's Gastrointestinal Center, your colorectal cancer treatment is personalized to provide the best outcomes, while focusing on your quality of life. We offer leading-edge treatments for colorectal cancer, including:
- advanced minimally invasive surgeries that provide successful treatment while helping you to recover more quickly.
- sphincter-preserving surgeries that can avoid the need for a colostomy bag.
- curative surgeries not available anywhere else for complex or advanced cancers through our multidisciplinary team of surgical experts.
Multidisciplinary Team Approach
Colorectal cancer treatment at MD Anderson is provided by a team of experts, including medical oncologists, surgeons, radiation oncologists, gastroenterologists, radiologists, clinical nurses and mid-level providers. They discuss your case and develop a treatment designed to attack your cancer while minimizing side effects.
Supplementing your clinical care, MD Anderson also provides nutrition counseling, pain management, psychological support, wound management and other services.
Younger patients can also receive specialized support through our Young-onset Colorectal Cancer Program. This program offers services like genetic counseling and testing, fertility preservation and young-adult support groups.
In addition, our advanced knowledge in cancer genetics can help diagnose and treat inherited family syndromes that may increase your risk of colorectal cancer. This expertise also helps us work with you to plan the most effective treatment for your specific condition.
For patients who have been successfully treated for colorectal cancer and are being monitored for recurrence, our tumor Intercept program also offers circulating tumor DNA testing. Patients may even be matched with clinical trials to monitor for or prevent the cancer’s return. This test can help doctors diagnose a recurrence long before it shows up in an imaging exam.
Leading-Edge Advancements
As one of the world’s largest cancer research centers, MD Anderson is a leading center for the investigation into new methods of colorectal cancer treatment and diagnosis. Through our clinical trials, this research can give patients access to treatments and procedures not found anywhere else.
And at MD Anderson you'll also be surrounded by the strength of one of the nation's largest and most experienced cancer centers. From support groups to counseling to integrative medicine care, we have all the services needed to treat not just the disease, but the whole person.
Be in touch with your body. If something feels new or weird, please don’t wait to see the doctor.
Annie Speck
Survivor
Treatment at MD Anderson
Colorectal cancer is treated in our Gastrointestinal Cancer Center.
Featured Articles

When to worry about blood in your stool (rectal bleeding)

The pill and cancer: Is there a link?

Processed meat and cancer: What you need to know
Neoplasms 101: What they are and how they’re treated

Breast cancer survivor-volunteer and colorectal cancer patient share unique friendship

Do sugary drinks increase colorectal cancer risk?

Colorectal cancer nurse inspired by patients every day
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.



