request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Colon Cancer
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsColon cancer is cancer that begins in the colon. The colon makes up about five to six feet of the large intestine. It is part of the digestive tract and moves waste, called stool, to the rectum, where it is held before being expelled through the anus.
Colon cancer is cancer that begins in the colon. The colon makes up about five to six feet of the large intestine. It is part of the digestive tract and moves waste, called stool, to the rectum, where it is held before being expelled through the anus.
Colon cancer that has not spread to distant parts of the body is usually treated with surgery, if feasible. If surgery is performed, doctors determine whether the patient needs additional treatments like chemotherapy.
Because of its location in the body and the location of nearby structures, colon cancer is slower than rectal cancer to spread to nearby organs as it grows.
How does colon cancer start?
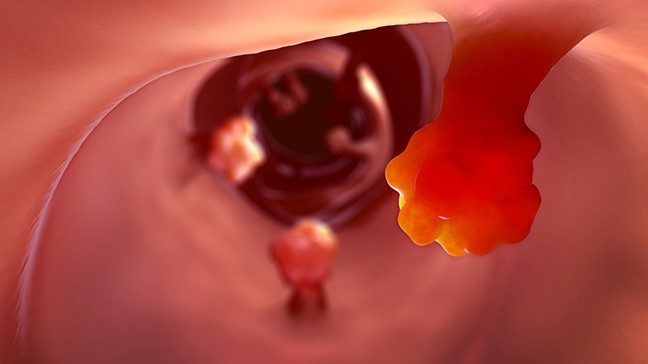
Colon cancer usually starts as a polyp. Polyps are small overgrowths in the tissue lining the colon or rectum. Polyps are not cancer.
Some polyps can turn into cancer over time. Most of these polyps are adenomas, which begin in mucus-producing gland cells that line the intestine and other organs. Adenomas are considered pre-cancerous growths.
It can take several years for an adenoma to develop into cancer. When it does, the cancer is called an adenocarcinoma. This is the most common type of colon cancer.
There are other, rarer types of colon cancer, including colon neuroendocrine tumors.
There are more than 150,000 combined colon and rectal cancer diagnoses in the United States each year. As of 2018, the disease’s five-year survival rate was about 65%. This figure does not include people diagnosed more recently, who could benefit from new treatments.
Young-onset colorectal cancer
Historically, most cases of colorectal cancer have been in people over age 55. In recent years, there has been an increase in diagnoses among people under age 55. MD Anderson’s Young-onset Colorectal Cancer Program offers specialized services for these patients. Services include fertility care, genetic testing and counseling, as well as support groups for young adults.
Colon cancer screening
Most precancerous polyps produce few, if any, symptoms, so it is important to get screened regularly for rectal cancer. Colon cancer screenings allow your doctor to find and remove polyps before they turn into cancer. Screening can prevent most cases of colon cancer. It can also catch colon cancer early, when treatments are more likely to be successful.
To learn more about colon cancer screenings, visit our Colorectal Cancer Screening Exams page.
Colon cancer risk factors
Anything that increases your chance of getting colon cancer is a risk factor. Colon cancer risk factors include:
- Age: More than 75% of colorectal cancer cases are diagnosed in patients age 55 and older. The median age at diagnosis is 66 years old. However, the rate of colorectal cancer diagnosed in adults less than 55 years old has increased in recent years.
- Race: African Americans have the highest rate of colorectal cancer among all racial groups in the United States.
- Family history: People whose relatives have had colorectal cancer or colorectal polyps have an increased risk of colorectal cancer.
- Inflammatory bowel disease: Patients with conditions that include Crohn’s disease or chronic ulcerative colitis are more likely to develop colon cancer. Learn more about inflammatory bowel disease and colorectal cancer.
- Personal history of colorectal cancer or polyps: People who have previously had colorectal cancer or colon polyps are at an increased risk of developing colorectal cancer.
- Hereditary cancer syndromes: Some genetic changes can be inherited and increase your risk for certain types of cancer. Inherited syndromes including hereditary nonpolyposis colorectal cancer, or Lynch syndrome, and familial adenomatous polyposis may put you at higher risk for developing colorectal cancer. Learn more about hereditary cancer syndromes.
- Diet: A diet heavy in red meat, processed meats, or meats cooked at very high heat can increase a person’s colon cancer risk.
- Obesity: Obesity increases a person’s chances of developing many different diseases, including colorectal cancer.
- Sedentary lifestyle: A lack of movement and exercise is a risk factor for colorectal cancer.
- Cigarette smoking: Tobacco use, including cigarettes and chewing tobacco, is a colorectal cancer risk factor.
- Drinking too much alcohol: Heavy drinkers are at an increased risk for colorectal cancer.
For patients concerned about inherited family syndromes that cause colorectal cancer, we offer advanced genetic testing and counseling to help understand your risk.
Colon cancer prevention
Lifestyle choices that may decrease your risk of getting colon cancer include:
- Regular screening tests
- Staying at a healthy weight
- Regular exercise
- Eating a healthy diet with lots of fruits and vegetables
- Avoiding cigarette smoking
- Drinking alcohol only in moderation
Learn more about colon cancer:
Learn more about clinical trials for colon cancer.
MD Anderson is #1 in Cancer Care
What are polyps?
You may already have heard about colon polyps. These abnormal cell growths are more likely to develop as we age. They occur in the colon and are removed during colonoscopies. The most common type resembles broccoli, with a stalk and a bulbous growth at the end.
But can polyps form anywhere else? What causes them? And, are polyps cancerous?
Read on to learn the answers to these questions and more.
Where can polyps appear in the body?
Polyps can form in any organ that has a hollow space where they can grow. This means polyps may develop virtually anywhere along your gastrointestinal, urinary or respiratory tracts, as well as in the female reproductive organs. This includes the:
- esophagus
- stomach
- gallbladder
- small intestine
- colon
- nasal cavity
- trachea (windpipe)
- vocal cords
- lungs
- kidneys
- ureters
- bladder
- urethra
- fallopian tubes
- uterus
- cervix
- vagina
Polyps can’t form in the liver because that organ is not hollow and its tissue is too dense. But the gallbladder has room, despite being filled with bile.
What causes polyps?
A polyp is an abnormal cluster of cells that multiplies and heaps up on itself in response to some kind of stimulus. That stimulus could be either environmental or genetic.
If the source is environmental, it’s usually connected to inflammation. Nasal polyps, for instance, often develop due to chronic irritation, whether that’s because of allergies or repeated exposure to inhaled chemicals.
If the source is genetic, though, it could be due to an inherited condition, including:
- Lynch syndrome
- Familial adenomatous polyposis
- MUTYH-associated polyposis
- Peutz-Jeghers syndrome
But mutations in many genes can cause or fail to suppress polyp formation. So, polyps aren’t always related to one of these disorders.

Colon cleanse: Health or hype?
You’ve probably heard that flushing out your colon can improve your health.
Ads for colon cleansing claim health benefits such as weight loss, energy boosts, improvements to the immune system and removal of toxins. Some even claim the practice reduces your risk for colon cancer.
But there’s little scientific proof to support these claims.
So, before you consider any type of colon cleanse, here’s what you should know.
Your colon already keeps you healthy
Your colon, or large intestine, is a long, muscular tube, and it is a key part of your digestive system. It removes water, salt and nutrients from the food you eat. The remaining solid waste forms stool.
Your colon then moves the stool along its walls to be expelled. This process rids the body of food waste and toxins. It also helps your colon maintain a healthy bacterial composition, known as your microbiome. Your microbiome plays a crucial role in protecting your body from infections, and it may even protect against colon cancer.
Colon polyps: 10 things to know
If you’re age 45 or older, your doctor may have already talked to you about the need to start getting a colonoscopy to check for polyps.
But what are colon polyps? Who gets them? And why do they need to be removed? We checked in with gastroenterologist David Richards, M.D.
What is a colon polyp?
I usually describe it as a little growth that develops in the lining of the large intestine, or colon.
Who typically gets colon polyps?
Men are more likely to develop colon polyps than women. But getting older is also a risk factor for developing polyps, which is why it’s recommended that people start having colorectal cancer screenings at age 45. Colonoscopy is the preferred method of screening for colorectal cancer.
Certain genetic syndromes can also predispose people to developing colon polyps and colorectal cancer. So, patients with Lynch syndrome or familial adenomatous polyposis will require earlier and more frequent follow-up. A significant family history of colon polyps, particularly pre-cancerous polyps, may also result in more frequent monitoring, and potentially earlier monitoring, than average-risk patients.
What do colon polyps look like?
Colon polyps can appear in a number of ways:
- Pedunculated: A little ball of tissue on the end of a stalk, like a broccoli floret or a mushroom.
- Sessile: A smooth bump or a gradually sloping “hill” on the lining of the colon.
- Flat: These are often very hard to see, as they may have no visibly raised portion at all.
- Depressed: In rare cases, patients may have a small dip or depression in the lining of the colon.
Is a colon polyp the same thing as a hemorrhoid?
No. Though they can bulge out of the colon wall when inflamed, too, hemorrhoids are just veins in the anal or rectal area that get swollen or irritated.
Are all colon polyps pre-cancerous?
No. Some abnormal growths can actually be benign. And there are several different kinds of colon polyps. Not all of them will turn into cancer. Even those that could turn into cancer someday aren’t necessarily guaranteed to. They just have the potential. That’s why they’re considered “pre-cancerous,” and looking for them during a colonoscopy is a standard part of colorectal cancer screening.
Which types of colon polyps are considered the most concerning?
Certain colon polyp features are more worrisome than others, but shape is not generally among them. The three things we tend to focus on most are:
- Size: Anything bigger than about 1 cm, or the width of a AAA battery
- Number: The more pre-cancerous polyps someone has, the higher their risk will be. So, someone with 1 or 2 small polyps is at less risk than someone with 3-9. And so on.
- Histology: This just means the way a polyp’s cells appear under a microscope. We examine their shape, as well as the order and way in which they grow, to look for abnormalities.
Do colon polyps cause any symptoms?
The vast majority of people with polyps have no symptoms at all. But polyps can sometimes cause bleeding, which ranges from microscopic levels that only show up as iron-deficiency anemia, to black tarry stools, to bright red blood. In rare cases, they might also cause some minor rectal discomfort or large amounts of mucus to be passed.
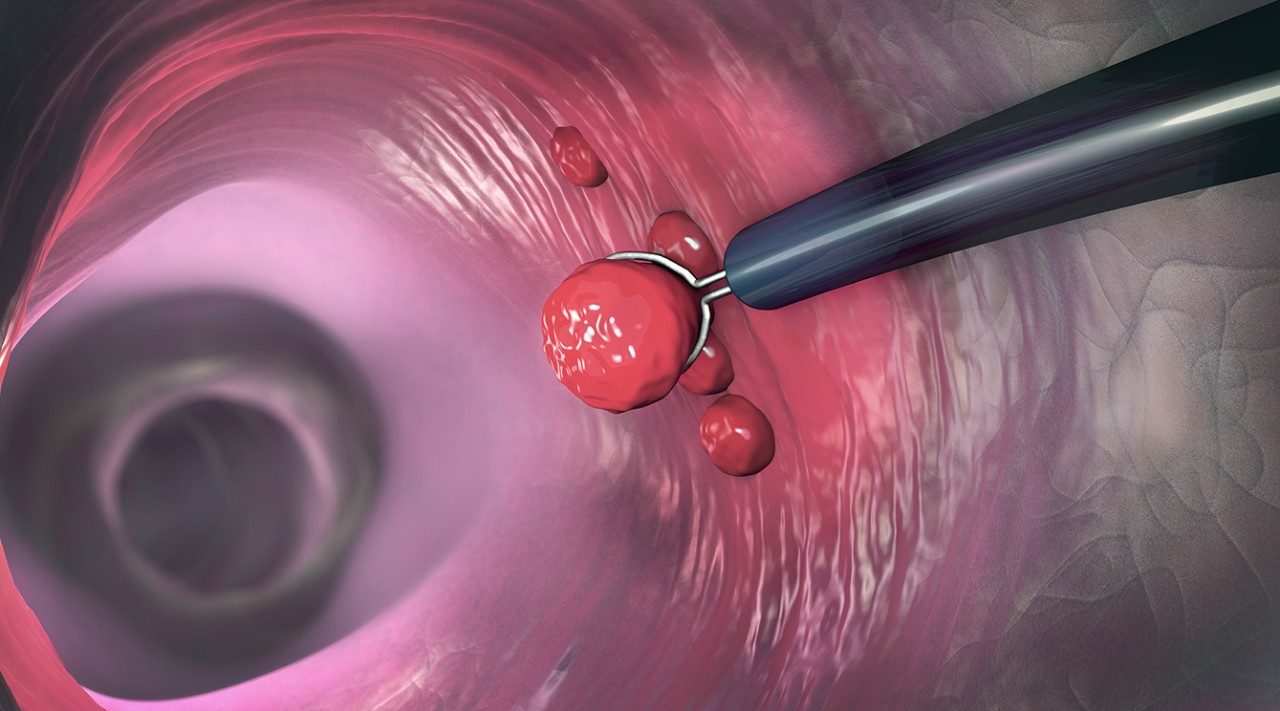
How are colon polyps removed?
Most colon polyps can be removed during a colonoscopy. That’s one reason doctors like colonoscopies so much. We can actually see the growths with our own eyes and remove them on the spot. And we’ve gotten so good at removing polyps with scopes now that very, very few patients need surgery to accomplish that.
Most polyps are removed with simple devices such as forceps or snares, which are introduced through the scope itself. If those methods aren’t feasible, polyps can be removed using a procedure called endoscopic mucosal resection.
Polyps can also be removed with a highly specialized procedure called endoscopic submucosal dissection. One of my colleagues, Dr. Phillip Ge, performs that technique quite a bit. It requires significant expertise, and is good for removing large polyps and early-stage colorectal cancers, too.
Which procedure is called for depends entirely on each patient and their unique situation. But the really cool thing about endoscopic submucosal dissection is that doctors are actually able to burrow underneath a polyp, getting between the colon lining and the muscles, and cut it out from below. That way, doctors can take out really big polyps in one chunk, rather than multiple fragments. And that’s important, because any time something is being taken out in pieces, rather than as a whole, there’s a small chance that a cell or two might be left behind where it could grow back.
How will the discovery of colon polyps impact my follow-up screening schedule?
If you have a lot of polyps, or they’re very large or pre-cancerous, you might need to be scoped more often. But it really depends on what kind of polyps are found and what their cells look like under a microscope.
If you had a really big polyp removed using endoscopic mucosal resection, you would also need to be followed much more closely. So, your doctor might recommend being scoped more frequently.
What’s the one thing you want people to remember about colon polyps?
Polyps themselves are not cancer. Some just have the potential to develop into it. We remove them so they never have that chance.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Why choose MD Anderson for colon cancer treatment?
At MD Anderson's Gastrointestinal Center, your colon cancer treatment is personalized to provide the best outcomes, while focusing on your quality of life. We offer leading-edge treatments for colon cancer, including advanced minimally invasive surgeries that provide successful treatment with less impact on you.
MD Anderson is also uniquely experienced in sphincter-preserving surgeries, eliminating the need for a colostomy.
Multidisciplinary Team Approach
Colonl cancer treatment at MD Anderson is provided by a team of experts, including medical oncologists, surgeons, radiation oncologists, gastroenterologists, radiologists, clinical nurses and mid-level providers. They discuss your case and develop a treatment designed to attack your cancer while minimizing side effects.
Supplementing your clinical care, MD Anderson also provides nutrition counseling, pain management, psychological support, wound management and other services.
Younger patients can also receive specialized support through our Young-onset Colorectal Cancer Program. This program offers services like genetic counseling and testing, fertility preservation and young-adult support groups.
In addition, our advanced knowledge in cancer genetics can help diagnose and treat inherited family syndromes that may increase your risk of rectal cancer. This expertise also helps us work with you to plan the most effective treatment for your specific condition.
For patients who have been successfully treated for rectal cancer and are being monitored for recurrence, our tumor Intercept program also offers circulating tumor DNA testing. Patients may even be matched with clinical trials to monitor for or prevent the cancer’s return. This test can help doctors diagnose a recurrence long before it shows up in an imaging exam.
Leading-Edge Advancements
As one of the world’s largest cancer research centers, MD Anderson is a leading center for the investigation into new methods of colon cancer treatment and diagnosis. Through our clinical trials, this research can give patients access to treatments and procedures not found anywhere else.
And at MD Anderson you'll also be surrounded by the strength of one of the nation's largest and most experienced cancer centers. From support groups to counseling to integrative medicine care, we have all the services needed to treat not just the disease, but the whole person.
Be in touch with your body. If something feels new or weird, please don’t wait to see the doctor.
Annie Speck
Survivor
Treatment at MD Anderson
Colon cancer is treated in our Gastrointestinal Center.
Featured Articles
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.

