We are MD Anderson
Health Care Provider Resource Center
The faculty at MD Anderson collaborates with and serves as a resource for health care providers within our community, across the nation, and around the world to provide the latest advances in cancer care.
The cancer control contiuum typically begins and ends with patients in the primary care setting that rely on the trusted relationship established with their provider. With this in mind, we continue to build upon referral access pathways to provide seamless transitions of care and deliver meaningful communication to referring providers about their patients.
By partnering with our commuities, MD Anderson is able to expand our impact on cancer through clincial trials, technology and education.
Referral Access Pathways
Patient-Centered Oncology Care and Your Practice
Cancer information developed specifically for health care providers to ensure patients are matched with the treatment options best suited for their unique cancer. Click to view or download.
Provider Profile
Update practice information; phone, fax and email.
Houston-Area Locations
Cancerwise Blog
Our blog features cancer research, treatment strategies and patient stories.
New understanding of why kidney cancers become metastatic discovered by MD Anderson researchers
Researchers at The University of Texas MD Anderson Cancer have engineered a new model of aggressive renal cell carcinoma (RCC), highlighting molecular targets and genomic events that trigger chromosomal instability and drive metastatic progression.
The study, published today in Nature Cancer, demonstrates that the loss of a cluster of interferon receptor (IFNR) genes plays a pivotal role in allowing cancer cells to become tolerant of chromosomal instability. This genomic feature may be used to help clinicians predict a tumor’s potential to become metastatic and treatment resistant.
Researchers led by Luigi Perelli, M.D., Ph.D., postdoctoral fellow of Genitourinary Medical Oncology, and Giannicola Genovese, M.D., Ph.D., professor of Genitourinary Medical Oncology, used CRISPR/Cas9 gene editing to create a model that faithfully represents RCC in humans, using cross-species analyses to provide further insights into the mechanisms involved in aggressive kidney cancer evolution.
“Until now, there haven’t been effective experimental models for metastatic renal cancer progression, but we introduced specific mutations that closely mimic the early stages of human cancers to see how tumors evolve and metastasize,” Genovese said. “These tumors become extremely genomically unstable, and, to tolerate this instability, they tend to lose genetic material at a specific site where the interferon genes are located. These insights can help clinicians identify tumors that have the genomic potential to become aggressive.”
Renal cell carcinoma is the most common type of kidney cancer, and patients often are treated effectively with surgery, targeted therapy, immunotherapy or a combination of these treatments. However, up to one-third of these patients will have aggressive disease progression, highlighting a need to understand specific mechanisms that drive metastasis in order to identify more effective therapeutic strategies and to predict treatment responses.
One hallmark of cancer is chromosomal instability, which is associated with resistance to many types of therapy and a poor prognosis. However, it is unclear if specific types of chromosomal abnormalities are involved in driving metastasis and how tumors are able to tolerate them.
The researchers used CRISPR/Cas 9-based genome editing to generate RCC models lacking common tumor suppressor genes. They then targeted cell cycle regulator genes to mimic common chromosomal abnormality associated with metastatic RCC in humans, leading to a phenotype consistent with the human disease. This is the first immunocompetent somatic mosaic model for metastatic RCC, meaning the model has an accumulation of different mutations that result in uncontrolled cell growth but still maintains a functional immune system.
Using genome sequencing and single-cell RNA sequencing to further examine these models, the researchers uncovered molecular drivers of RCC and gained a new understanding of the evolution of chromosomal instability.
Their single cell analyses revealed that a cluster of highly conserved IFNR genes were suppressed in the model, and that this cluster normally functions as a critical gatekeeper, or tumor suppressor, of renal cancer progression.
IFNR gene clusters normally are involved in the immune response. After analyzing various data sets from both mice and humans, the researchers discovered an inverse correlation between the loss of these IFNR genes and aneuploidy, a condition marked by having an abnormal number of chromosomes.
This study suggests that the tumors adapt to high levels of chromosomal instability through the disruption of the IFNR pathway and that this is likely a major biomarker of metastatic potential. It also highlights how renal cancers in different species have followed similar evolutionary patterns that converge around chromosomal instability, which in turn may explain the heterogeneity of these tumors.
In the future, the researchers plan to test drug combinations in these newly generated models to determine how the tumors adapt to various therapies, with the goal of rapidly translating these studies into clinical trials that can help predict treatment response in patients with RCC.
This work was supported by the Fondazione AIRC per la Ricerca sul Cancro (AIRC), the Conquer Cancer Foundation of the American Society of Clinical Oncology, the Kidney Cancer Association, Horizon Europe , the Sheikh Ahmed Bin Zayed Al Nahyan Center for Pancreatic Cancer, the Pancreatic Cancer Action Network, Inc., the Ransom Horne Jr. Professorship for Cancer Research, the Barbara Massie Memorial Fund, MD Anderson’s Moon Shots Program®, the Bruce Krier Prostate Cancer Research Endowment Fund, the Lyda Hill Foundation, the UK Medical Research Council, the National Institutes of Health (NIH) (R01 CA258226-03), and the U.S. Department of Defense (W81XWH-21-1-0950) . A full list of collaborating authors and their disclosures can be found with the full paper here.
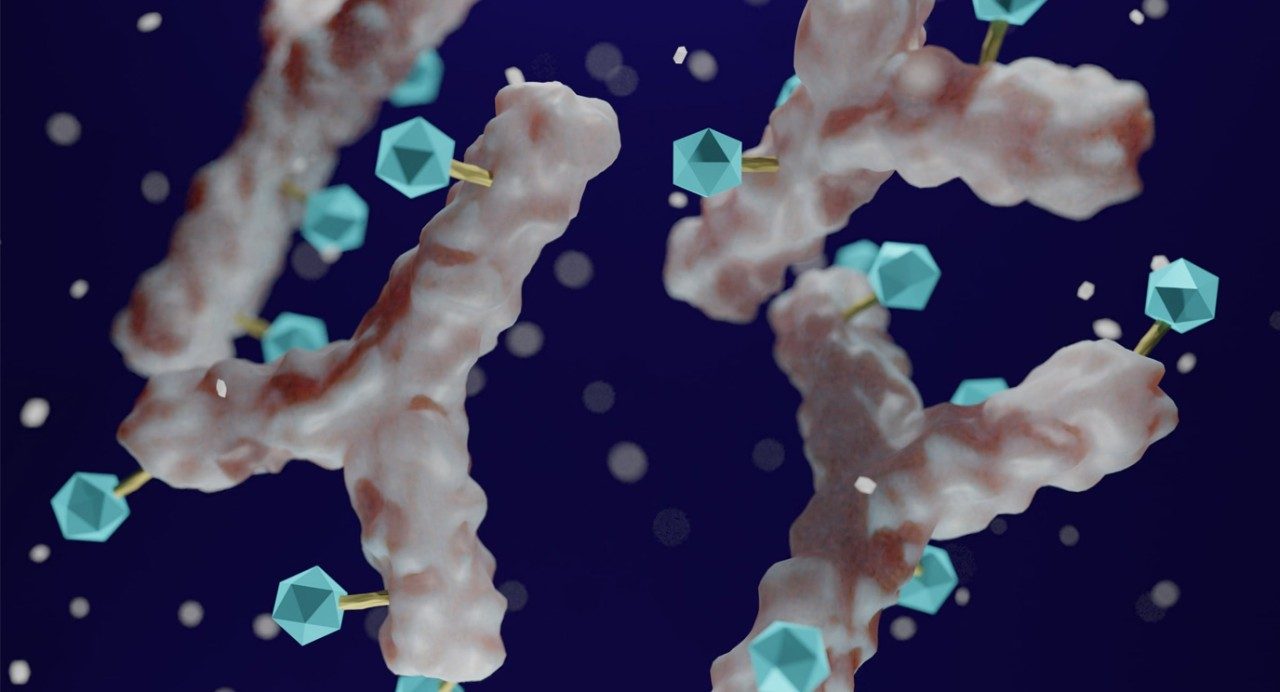
Antibody drug conjugates: A shift in treatment options for solid tumors
Antibody drug conjugates have existed for years, but several recent advances are helping to refine how these cancer drugs work, expanding our understanding to help overcome their challenges and, ultimately, extending their benefit to more patients.
“Antibody drug conjugates are an exciting field of drug development,” says Funda Meric-Bernstam, M.D., chair of Investigational Cancer Therapeutics.
Antibody drug conjugates target cancer cells with a powerful punch
Potent cancer drugs are typically unable to differentiate cancer cells from normal ones. Antibody drug conjugates overcome this challenge by linking the drug to a monoclonal antibody specifically chosen to target and deliver the drug to cancer cells.
“We conjugate a cancer drug, such as a chemotherapy that’s highly toxic, to an antibody that targets a protein on the surface of a cancer cell,” says Meric-Bernstam. “The thought is that by delivering much higher concentrations of chemotherapy to cancer cells, we have a greater therapeutic index.” Because the drug payload is directly carried to the cancer cell, it reduces the side effects a patient may experience.
Antibody drug conjugates are administered intravenously, and the frequency of treatment depends on the specific drug. Many antibody drug conjugates are being used or explored to treat metastatic disease, and patients continue to receive infusions as long as they’re benefitting from treatment. However, antibody drug conjugates are also being explored to treat patients with earlier stage disease.
HER2 serves as a target for antibody drug conjugates across several cancer types
The first antibody drug conjugate used to treat solid tumors was T-DM1, a combination of the HER2 protein-targeting monoclonal antibody trastuzumab and a chemotherapy drug called DM1.
T-DM1 is approved to treat metastatic breast cancer with overexpression of HER2, meaning there are high levels of HER2 protein on the surface of the cancer cell. It’s also approved to treat breast cancer with HER2 amplification, which means there is a higher-than-normal number of copies of the HER2 gene.
The level of HER2 expression of a tumor cell is determined by an immunohistochemistry (IHC) test. HER2 positive cancers are defined as either IHC 2+ with amplification or IHC 3+, with the higher number of IHC denoting a higher level of HER2 protein.
In addition to breast cancer, HER2 can also be found in several other types of cancers including stomach, lung, gynecologic and bladder cancers, but the levels of HER2 expression vary across tumor types.
DESTINY-PanTumor02 and other clinical trials aim to expand antibody drug conjugate benefit
The next evolution of HER2-targeting antibody drug conjugates came quickly with the introduction of the trastuzumab deruxtecan. Like T-DM1, it shows strong efficacy in tumors with high levels of HER2. But unlike T-DM1, it has also been shown to be effective against breast cancers with lower HER2 levels.
“Trastuzumab deruxtecan represents a rapid evolution in antibody drug conjugate technology that may be more efficacious. It has opened the door for many more patients to potentially benefit from these treatments,” says Meric-Bernstam.
Trastuzumab deruxtecan is currently approved by the Food and Drug Administration (FDA) to treat patients with HER2 positive breast cancer, HER2 low breast cancer (HER2 2+ or 1+ tumors without amplification), HER2 positive gastric cancer and HER2 mutant lung cancer.
Yet patients with more difficult-to-treat HER2-expressing cancers are without a targeted treatment option.
Meric-Bernstam is leading several clinical trials investigating antibody drug conjugates. One study is the DESTINY-PanTumor02 clinical trial, a multicenter basket clinical trial investigating trastuzumab deruxtecan in patients with solid tumors with IHC 2+ or 3+ levels of HER2 expressions.
New targets may lead to new antibody drug conjugate options for patients
The burst of development in antibody drug conjugates can be credited to the progression of the technology used to link the drugs’ components as well as it can be attributed to improvements to the efficacy of the payload drugs.
As antibody drug conjugates have evolved, more targets have been identified. “We now see multiple targets moving forward as well as different strategies to treat the same patient population,” says Meric-Bernstam.
For example, the TROP2 protein is overexpressed in several epithelial tumor types, including triple-negative breast cancer, hormone receptor positive breast cancer and bladder cancer. Sacituzumab govitecan is approved to treat patients with these TROP2 positive cancers, and other drugs, such as datopotamab deruxtecan, are being investigated to treat the same TROP2 positive cancers.
In addition, enfortumab vedotin has been explored to target tumors overexpressing the nectin protein. Although nectin is overexpressed in other tumor types, thus far the drug has been approved to treat patients with nectin positive bladder cancer.
Improved understanding will lead to better patient selection
Over the next few years, Meric-Bernstam expects several more antibody drug conjugates to emerge. “I think we’ll see multiple antibody drug conjugate options for patients,” she says.
New questions will arise as more antibody drug conjugates that target the same proteins in the same patient population are developed. To improve patient selection, Meric-Bernstam says more research is needed to:
- understand the influence of a protein’s expression level on the efficacy of the drug
- evaluate if and how previous treatment with a different antibody drug conjugates and other chemotherapies will impact efficacy and sequencing
- better predict patient response to the various payload options
- anticipate the potential side effects
Although side effects vary between the antibody drug conjugates, Meric-Bernstam warns there is still the risk of side effects related to bone marrow, lung inflammation and neuropathy. Lastly, she predicts that there will be more research exploring rationale combinations, too.
With so many advances made in the field in such a short time, Meric-Bernstam sees antibody drug conjugates as shifting the options for patients with difficult-to-treat solid tumors.
“We’ve seen so many antibody drug conjugates demonstrate benefit to patients with difficult-to-treat tumors that, in my mind, they’re the next pillar of cancer therapeutics,” says Meric-Bernstam.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.

Clinical trial of new AhR inhibitor shows cancer might be even more wily than we thought
The human immune system is constantly attacking damaged cells that might turn into cancer, thus protecting us from these cells growing out of control and becoming malignant. However, cancer cells have many ways of protecting themselves from the body’s immune system. One of these is a protein, called aryl hydrocarbon receptor (AhR), which is common on tumor and immune cells. When AhR is activated, it causes immunosuppression and promotes growth of the malignant tumor.
Researchers at MD Anderson — along with collaborators at Yale, as well as in Canada, the UK, Germany and Spain — have been conducting a Phase I clinical trial of a drug called BAY 2416964 that can block AhR. As a result, it should increase the activity of antigen-presenting cells and T cells and reduce the activity of immunosuppressive myeloid cells – thus allowing the immune system to see and attack the cancerous tumor.
Ecaterina Dumbrava, M.D., assistant professor of Investigational Cancer Therapeutics at MD Anderson, presented the group’s findings at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting.
“It’s a new drug with a new mechanism of action, which is always exciting,” Dumbrava says. “It’s part of what is called immune metabolomics, meaning it acts on the metabolism of the tumor and immune cells.”
Theoretical background seems promising
In theory, BAY 2416964 should help patients with advanced solid tumors of many common cancer types because it “antagonizes” the transcription factor activity of AhR by competing with its ligands. AhR is part of the pathway that changes tryptophan into kynurenine, and this pathway plays an important part in the metabolism of cancer progression and is believed to limit the efficacy of anti-PD-1 therapy, a type of immunotherapy commonly given to cancer patients. Efforts to interfere with the first part of the pathway, IDO, have led to disappointing results in clinical trials. However, AhR inhibition blocks downstream effects so, in theory, drugs like BAY 2416964 that act on AhR shouldn’t have the same issues.
“There is a difference between targeting only IDO versus targeting downstream enzymes in the tryptophan pathway as a possible alternative approach to restore the tumor immune response,” Dumbrava says. “Blocking AhR is expected to enhance immune response and improve outcomes in combination with PD-1 checkpoint inhibitors.”
The clinical trial, though, first needed to determine how BAY 2416964 acts on its own.
How the Phase I clinical trial works
The first part of the clinical trial enrolled patients with all types of solid tumors. Participants were given increasing amounts of BAY 2416964 to find the optimal dose. These 39 enrollees had cancers like colorectal cancer, breast cancer, pancreatic cancer, kidney cancer, ovarian cancer or thymus gland cancer that hadn’t responded to previous treatment. Although they experienced some side effects from BAY 2416964, none experienced severe reactions or had to discontinue the use of the drug as a result.
In addition, blood tests showed evidence of AhR inhibition. That meant the drug was working as intended.
With the safety of different doses of the drug established, the researchers next enrolled patients with non-small-cell lung cancer or head and neck squamous cell carcinoma.
Dashed hopes and next steps
Unfortunately, the results of the clinical trial weren’t as successful as the researchers had expected, based on preclinical models and a solid theory behind the drug. Of the 67 patients able to be evaluated for their response to the drug, only 32.8% had stable disease. There was also one patient with thymoma in the first part of the trial who achieved a partial response. No other patients achieved a partial or complete response to the drug.
Despite these findings, Dumbrava and her colleagues hope that BAY 2416964 may still play a valuable role in treating cancer when combined with other drugs, especially PD-1 checkpoint inhibitors.
“Safety data and observed pharmacodynamic effects support combination therapies,” Dumbrava says. “A study in combination with pembrolizumab, which is a type of PD-1 checkpoint inhibitor, is currently ongoing, and it’s possible that giving these two drugs together will be more effective than either one alone.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop UT MD Anderson
Show your support for our mission through branded merchandise.