request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Ovarian Cancer
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsOvarian cancer is a type of cancer that begins in the female reproductive organs that produce and store eggs (ovaries). It occurs when abnormal ovarian cells divide and multiply uncontrollably.
Ovarian cancer is a type of cancer that begins in the female reproductive organs that produce and store eggs (ovaries). It occurs when abnormal ovarian cells divide and multiply uncontrollably.
“Ovarian cancer” is a generic term for any primary malignant ovarian tumor. However, ovarian cancer is not one disease. There are many types of ovarian cancer, including some that are extremely rare and require specialized treatment. Therefore, establishing the correct diagnosis upfront is very important. The main types of ovarian cancer are named for the cells where the disease first forms.
Types of ovarian cancer
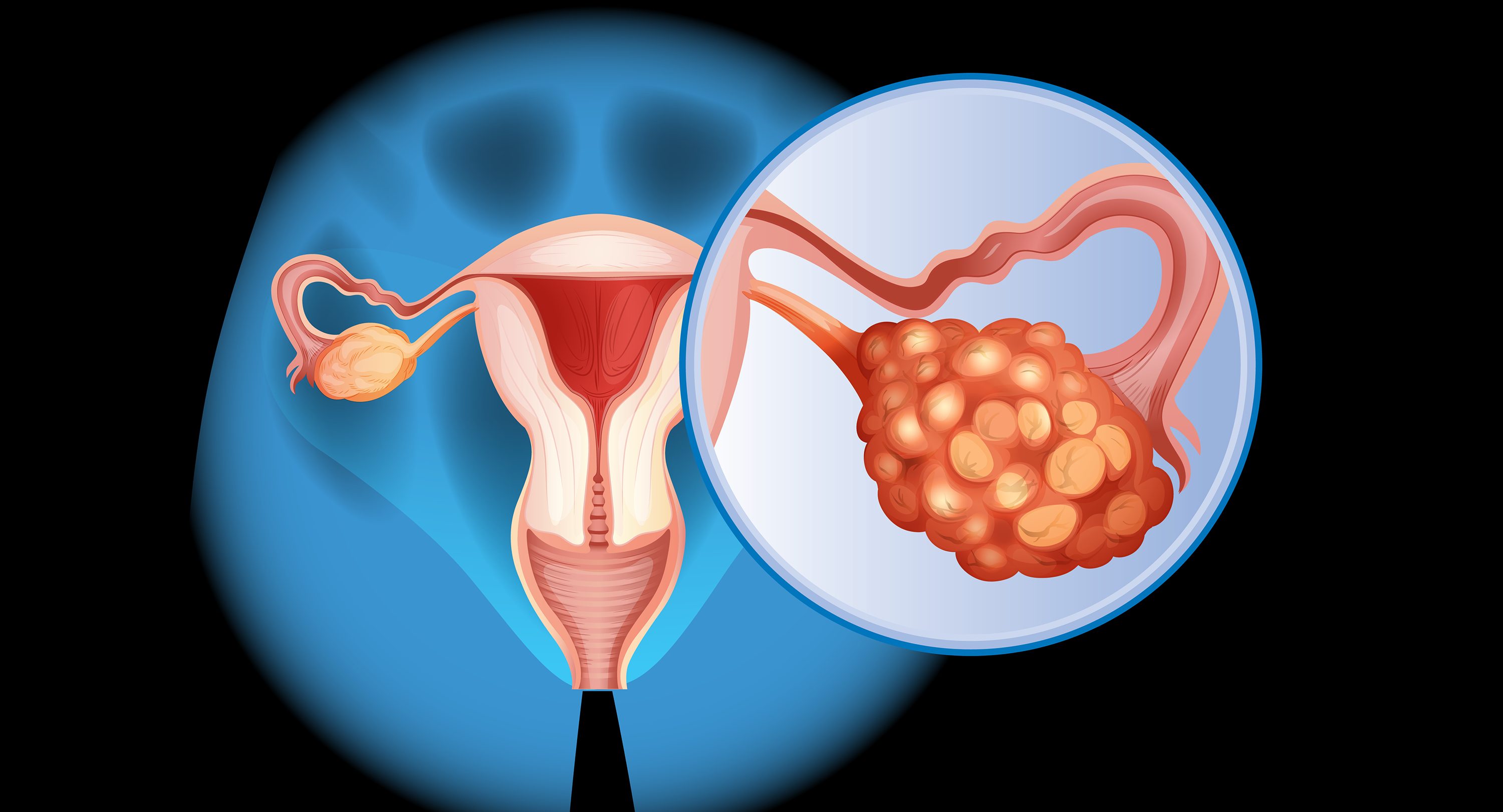
Epithelial ovarian cancer
About 90% of ovarian cancers start in the epithelium tissue; these cancers may come from the fallopian tube or from cells in the ovary. These may also arise from tissue that has implanted on the ovary. For example, endometriosis attached to the ovary may turn into endometrioid (carcinoma). This type of ovarian cancer is divided into many subtypes, including serous, mucinous, endometrioid, clear cell, transitional and undifferentiated types. The risk of epithelial ovarian cancer increases with age, especially after the age of 50.
Germ cell ovarian cancer
Germ cell tumors account for about 5% of ovarian cancers. They begin in the egg-producing cells. This type of ovarian cancer can occur in women of any age, but about 80% are found in women under the age of 30. The main subtypes are teratoma, dysgerminoma, endodermal sinus tumor and choriocarcinoma.
Stromal ovarian cancer
These tumors represent about 5% of ovarian cancers. They grow in the connective tissue that holds the ovary together and makes estrogen and progesterone. Most are found in older women, but sometimes they occur in girls.
Stromal tumors usually do not spread as fast as other ovarian tumors. Subtypes include granulosa, theca and Sertoli-Leydig cell tumors.
Primary peritoneal ovarian cancer
Primary peritoneal ovarian cancer is rare. It has cells that look like high-grade serous ovarian cancer, but it starts in the lining of the pelvis and/or abdomen. Women can get this type of cancer even after their ovaries have been removed. Symptoms and treatment are similar to those of epithelial ovarian cancer.
Ovarian cancer screening
Ovarian cancer screening is recommended only for women at increased or high risk.
Being at increased risk does not mean you will get ovarian cancer. But it does mean you should start regular screening exams to detect cancer if it develops. When found early, the chances for successfully treating the disease are greatest.
You can find out more, including who is at increased risk and how to schedule a screening, on our Ovarian Cancer Screening page.
Ovarian cancer risk factors
Anything that increases your chance of getting ovarian cancer is a risk factor. These include:
- Age: The risk of ovarian cancer increases with age. About half of ovarian cancers are in women over 60.
- Family history of ovarian cancer
- One close relative with ovarian cancer who has a suspected BRCA1 or BRCA2 mutation
- Genetic factors: Approximately 10% to 15% of ovarian cancers are due to genes that make you more likely to develop cancer. These include:
- BRCA1 or BRCA2 mutations or suspected risk of BRCA1 or BRCA2 mutations
- Lynch syndrome (hereditary nonpolyposis colorectal cancer)
- Never having children. The more children you have, the less likely you are to develop ovarian cancer.
Not everyone with risk factors gets ovarian cancer. However, if you have risk factors, it’s a good idea to discuss them with your health care provider.
Some people have an elevated risk of developing ovarian cancer. Review the ovarian cancer screening guidelines to see if you need to be tested.
Some cases of ovarian cancer can be passed down from one generation to the next. Genetic counseling may be right for you. Learn more about the risk to you and your family on our genetic testing page.
Learn more about ovarian cancer
MD Anderson is #1 in Cancer Care

Ovarian cancer survivor, employee: Treatment at MD Anderson is ‘the best decision I ever made’
I work in Philanthropy at MD Anderson, and I’m a cancer survivor. This means I can say I’ve been both an employee and a patient at the greatest cancer hospital in the world.
In 2018, I was diagnosed with a type of ovarian cancer called dysgerminoma. I was 32 years old, so this was a rare cancer for someone my age. I found out about my cancer diagnosis through my annual well-woman exam. My normal gynecologist was pushing down on my belly and felt something hard that shouldn't be there. I ended up having surgery to remove it. It turned out to be cancer. I immediately knew that MD Anderson was where I wanted to be treated.
Getting a cancer diagnosis at such a young age is shocking and terrifying. It's not supposed to happen; it’s odd, scary and overwhelming. But, as an MD Anderson employee, I knew firsthand how patients are treated and how care is individualized to the patient. I knew my best chance for treatment was going to be at MD Anderson.
Hands down, it was the best decision I ever made.
Today, I’ve been cancer-free for six years. Here are three perspectives I learned through my cancer treatment.
1. A deeper understanding of individualized care
As an employee, you're always told that we prioritize individualized care at MD Anderson. But it's not until you become a patient that you experience it. Making that shift connected so many dots and allowed me to understand another side of MD Anderson.
Going in for your first appointment is terrifying and overwhelming because of all the unknowns. Chemotherapy was a huge fear of mine because I'd seen chemo portrayed on television and in movies as people who get really sick and just waste away. But my care team did such an amazing job of making me not just feel welcome, but also safe. They were one of the biggest reasons why I felt like I was going to be OK. I'm a person who wants to know as much as possible, so my team provided me with a lot of information. That way, I wouldn’t have to wonder and worry. They were so caring, warm and professional; they knew exactly what we were dealing with. My cancer is a rare cancer, but at MD Anderson, it's not rare.
My care team also asked me questions about my daily life so they could tailor my treatment plan to my needs. The very first day that I met my doctor, he asked if I got motion sick. I said yes, and a couple hours after I saw him, he gave me a call and said that we were going to change my chemo regimen to a different drug that would help me avoid that. Then, before starting treatment, I met with a pharmacist to learn about the medications I'd be taking. When we discussed anti-nausea medications, she told me to let her know if my medication didn’t work so she could find me a better option. Little things like that really made me feel special and cared for.
2. The importance of ‘just another Thursday’
I tried to keep my life as normal as possible during treatment. This included both my routine and my relationships.
I couldn't go into the office when I was having chemo, so for the week after chemo, I would work from home. Then, when I went to the office, I’d try to make it just like another Thursday. At times, chemobrain made it hard to remember things, which would get very frustrating, so I started writing lots of things down. I had to learn to be gentle with myself when those times happened; it was a moment, it wasn't forever.
For my own mental sanity, I still needed to joke with my friends and have typical conversations with people. I talked to family and friends about acting normal around me. I told my parents, “It's going to be fine. Everything is normal. We can talk about it. Ask me questions, but let's not tiptoe around anything."
My care team also provided me with a sense of normalcy in a time when nothing felt normal. Before my chemo appointments, we would chat about our personal lives and upcoming trips. These casual conversations made me feel comfortable messaging them with all my treatment questions. I never felt like I was bothering them; instead, it really felt like they loved talking and chatting and hanging out.
I also meditated, practiced yoga and journaled during treatment. One of my neighbors would drop by to do art projects during lunchtime when I was working from home. That connection was a little pick-me-up that helped as I tried to keep everything as normal as possible.
3. What it means to be a cancer survivor
Even though I am a cancer survivor, I’m still very connected to MD Anderson. My post-cancer care and support has been great. My care team is wonderful and optimistic. If I'm ever feeling like I need extra support, I can talk to our Social Work team or reach out to support groups.
Today, my experience as a patient gives me a unique perspective in my role on the Philanthropy team. Donations are pivotal. Fundraising is a huge reason why MD Anderson is so successful and can invest so much in research, clinical trials, support programs like our Adolescent and Young Adult Program and Children’s Cancer Hospital, and other resources for patients and their networks. Cancer doesn't just affect the patient, it affects everyone in that patient's life. MD Anderson provides patients and their families and friends with so many resources to help them get through a really difficult time.
My role as a survivor is a huge milestone and accomplishment. It’s also a reminder of my responsibility to encourage other people to get preventative exams. If my cancer diagnosis can help somebody else down the road, then it was all worth it.
Request an appointment at MD Anderson online or call 1-877-632-6789.

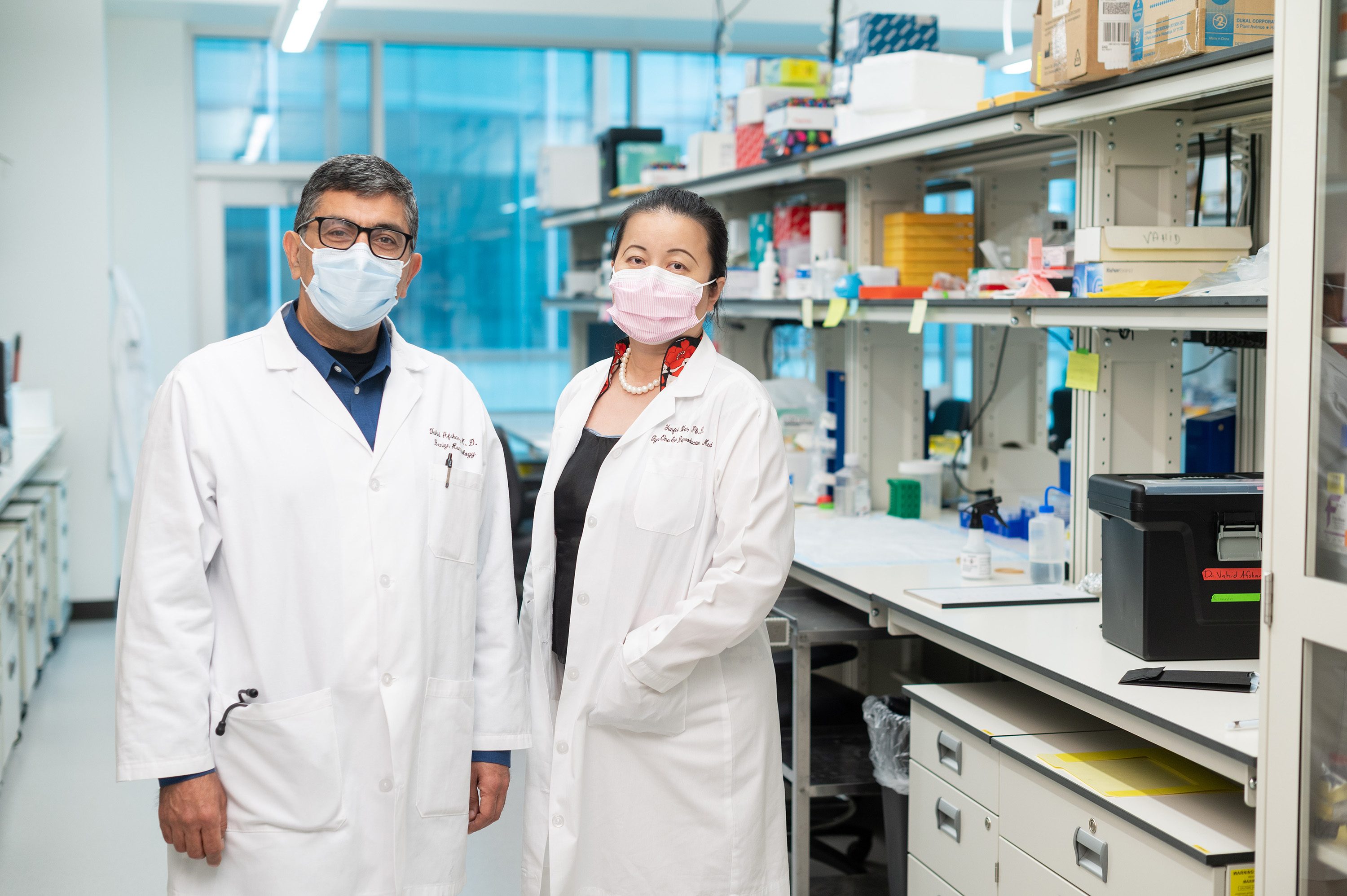
Gynecologic oncologist: Why I’m passionate about cancer care at MD Anderson
I’ve always sought out opportunities to advocate for women and women’s health. That’s what drew me to the field of gynecologic oncology.
As a gynecologic oncologist at MD Anderson, I treat cancers of the female reproductive system, including endometrial cancer, cervical cancer, ovarian cancer, vulvar cancer and vaginal cancer. My passion aligns with MD Anderson’s mission to end cancer. I’m thankful I get to work with so many incredible people who share my passion and dedication to Making Cancer History® and improving the lives of our patients.
Connecting with patients is crucial to personalized care
As an oncologist, I’ve learned that there’s no one-size-fits-all approach to treating cancer.
Cancer treatment is a personal experience. As cancer care evolves, we often have multiple ways to approach a challenge. We need to understand how the cancer is affecting the person in front of us so we can make a treatment plan that will get them through treatment and beyond.
That’s why I start by asking questions. I want to get to know my patients and their caregivers. I want to understand what their goals are. After that, I can determine what diagnostic tests we need to do. Then we can create a treatment plan that aligns with best practices and meets the needs of the patient and their support system.
MD Anderson’s multidisciplinary care sets us apart from other institutions. We offer the best specialized care, whether it's medical oncology, surgical oncology or radiation oncology. Having multiple specialists review your care plan before we start treatment means that you're going to receive the right care at the right time and have the best chance for a positive outcome.
Why I value my team at MD Anderson
When you become a gynecologic oncology patient at MD Anderson, you have an entire team supporting you, including nurses, advanced practice providers, medical assistants or my colleagues in the operating room.
I'm always inspired when I come to work because I know that my team is incredible, they're energized and they care about our patients as much as I do.
I think the key to having an effective team is respecting and trusting one another. For example, I know that if I need to have a difficult conversation with one of my patients, I can rely on my team to handle everything outside of that room so that I’m able focus on the patient and their loved ones.
I hear from my patients all the time about how much they love their care team and feel like they can always turn to them with questions or concerns.
My guiding principle when caring for each patient is, ‘Would I be doing the same if this patient was my family member?’ We get to know our patients so well – through surgery, chemotherapy, surveillance and survivorship. We do consider them family. We’re there through the highs and lows of treatment, and it’s a privilege to be able to offer support and guidance to them during that time.
Clinical trials help us better treat patients
Clinical trials are a critical part of our work to end cancer. There’s so much that we need to understand, learn and improve on to conquer a disease that is always changing. Clinical trials help us do that.
It's important for patients to have access to clinical trials, so we can offer them the very best cancer treatments. In addition, we may be able to extend their life and improve their quality of life.
MD Anderson is doing a lot of research in the field of gynecologic oncology. I encourage all patients to ask their doctors about clinical trials to see if they would be a good option for you.
Why you should come to MD Anderson for cancer treatment
MD Anderson only focuses on cancer, so we're able to provide the best comprehensive care to patients from the moment they're diagnosed through their treatment and onto survivorship. You won't be a number here or just another patient. We'll develop a multidisciplinary treatment plan that's right for you.
Because we focus only on cancer, we understand the highs and lows our patients go through better than anyone else. We focus on cancer care, we specialize in cancer care, and I believe we provide the very best cancer care there is.
Jolyn Taylor, M.D., is a gynecologic oncologist at MD Anderson.
Request an appointment at MD Anderson online or call 1-877-632-6789.
Should you have your fallopian tubes removed to reduce your ovarian cancer risk?
A woman could have her fallopian tubes removed for any number of reasons. Sometimes, it’s necessary to treat an ectopic pregnancy or to resolve an infection caused by pelvic inflammatory disease. In other cases, it’s done as a form of permanent birth control.
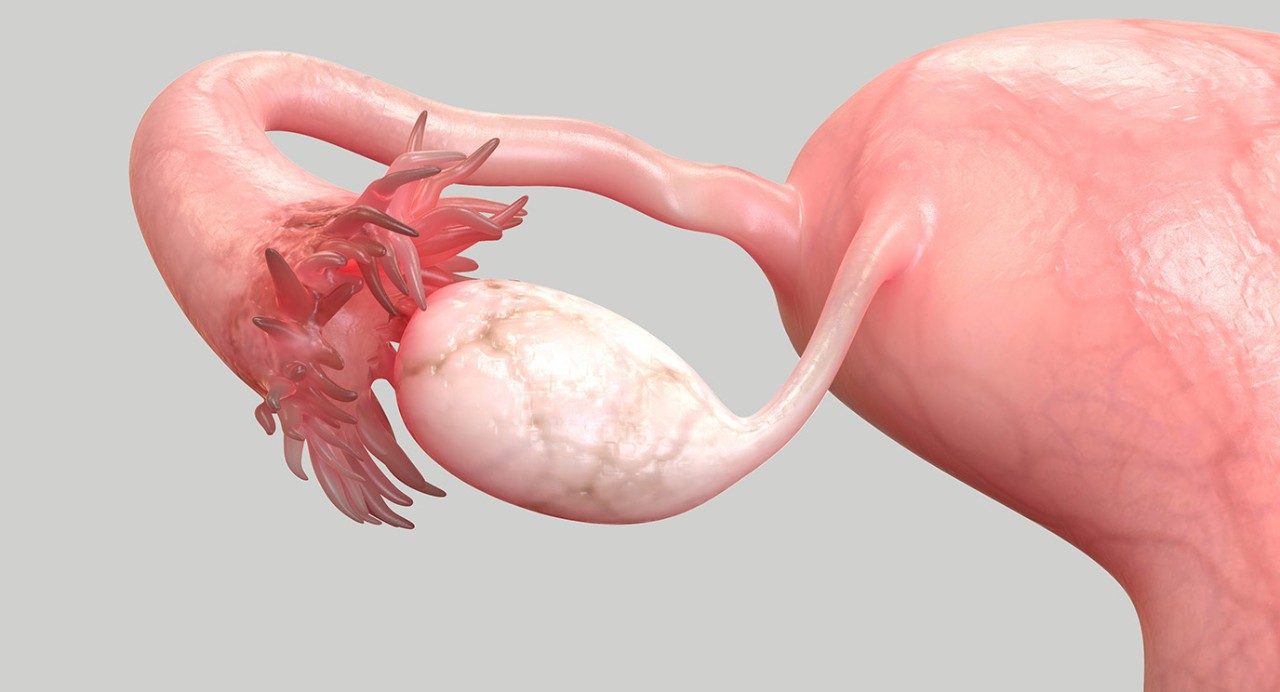
But a growing body of evidence suggests that the distal fallopian tube — or flower-shaped section located nearest the ovary — is the site of many cases of high-grade serous ovarian cancer, the most common type of ovarian cancer and one of the most aggressive.
Research also suggests that an opportunistic salpingectomy — the complete removal of the fallopian tubes during an unrelated pelvic surgery — could help reduce the chances of one day developing ovarian cancer.
So, who should consider having their fallopian tubes removed, and when? And, should anyone who’s finished childbearing seek out the procedure, even if they’re only at average risk of ovarian cancer? We asked Michaela Onstad-Grinsfelder, M.D., a surgeon specializing in gynecologic cancers.
Why do women typically have their fallopian tubes removed?
Women don’t usually go in just to have their fallopian tubes removed unless it’s for permanent birth control or to treat an ectopic pregnancy.
Having the fallopian tubes removed is one form of surgical sterilization, or “having your tubes tied.” Until fairly recently, it was more common for surgeons to use a metal clip or a ring to constrict and physically block the tubes, rather than removing the structures themselves.
Why has that changed?
A growing body of data suggests that the fallopian tubes may be the origin of many ovarian cancers. So, a lot of surgeons have changed their practice to remove the fallopian tubes entirely to give patients additional protection against ovarian cancer.
In the United States, the Society for Gynecologic Oncology and the American College of Obstetricians and Gynecologists both support the removal of fallopian tubes as permanent sterilization for women at average risk for ovarian cancer, but it’s also recommended by professional organizations in Australia, Canada, Germany and New Zealand.
How was this information discovered?
After the BRCA gene was linked to an increased risk for breast and ovarian cancers, doctors started removing the ovaries and fallopian tubes as a type of risk-reduction surgery, once BRCA-positive women were finished with childbearing.
Most ovarian cancers are diagnosed at stage III or IV, so we don’t usually see the disease in its earliest stages. But what we noticed when we started performing these surgeries is that there were often pre-cancerous lesions present in the fallopian tubes.
This was a really exciting discovery because, before that, we hadn’t known there was a lesion that could one day become ovarian cancer. So, we were able to start finding ovarian cancers really early that we hadn’t been able to catch before.
How did that discovery lead to the recommendation of opportunistic salpingectomies?
There was a lot of excitement in the medical community at that point about the possibility of reducing the risk of ovarian cancer by removing the fallopian tubes during hysterectomies or when patients were having their “tubes tied.” Before that, whenever someone had a hysterectomy, we would normally only take out their fallopian tubes if we were also taking out their ovaries.
But as the new data emerged, there was an increased interest in removing the fallopian tubes along with the uterus when performing hysterectomies. Because if a woman is pre-menopausal, her ovaries might still be benefitting her. But once she’s finished childbearing, the fallopian tubes serve no real purpose.
So, who should consider having their fallopian tubes removed?
People who are at increased risk of developing ovarian cancer, such as those who carry the BRCA genetic mutation, are recommended to have a stand-alone surgery to remove fallopian tubes with both ovaries (called a risk-reducing salpingo-oophorectomy).
Otherwise, it’s only recommended as an opportunistic salpingectomy: something to be done when you’re already having another type of gynecologic procedure, such as a hysterectomy.
Are any related clinical trials available?
We have a clinical trial going on right now for BRCA-positive women who are done with childbearing but are not quite ready to have their ovaries removed.
In this clinical trial, participants will have their fallopian tubes removed now, but delay the removal of their ovaries until later (between the ages of 35 and 45 for patients with BRCA1 and between the ages of 40 and 50 for those with BRCA2). The goal is to determine if it may be safe to delay the removal of both ovaries for women at high risk of developing ovarian cancer.
Do you ever foresee a time in which an opportunistic salpingectomy could be combined with another procedure, such as an appendectomy or a hernia repair?
Right now, we don’t typically bundle other types of surgeries with the removal of fallopian tubes. That’s partially because only OB-GYNs are specifically trained in that procedure.
But we’re actively looking for ways to team up with other surgeons to offer this service together. It could be an exciting strategy in the future to further reduce patients’ risk of ovarian cancer.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.


Featured Podcast:
Why are more women under 50 getting cancer?
Why choose MD Anderson for ovarian cancer treatment?
A team of some of the nation's top experts works together to address your specific condition when you come to MD Anderson's Gynecologic Oncology Center for ovarian cancer treatment and diagnosis. This team includes gynecologic oncologists, radiologists, radiation oncologists, surgical oncologists and pathologists. They are joined by a support staff trained to provide the highest level of ovarian cancer treatment.
This group follows you every step of the way, communicating and collaborating closely to deliver outstanding care. Their aim is to deliver the most advanced, minimally invasive ovarian cancer therapies while limiting side effects as much as possible.
Ovarian cancer care planned just for you
Your treatment for ovarian cancer is personalized to include leading-edge technologies and techniques. These may include advanced surgical procedures, chemotherapy options and targeted therapies. In addition, we offer treatment for benign (non-cancerous) tumors of the ovaries.
We are one of the most active centers in the nation for the treatment of rare ovarian cancers and relapsed ovarian cancer cases, offering the highest level of care that can include clinical trials and innovative approaches such as targeted therapies.
Surgery often is needed for an ovarian cancer diagnosis, but it is important to carefully consider the timing of surgery. Because MD Anderson is a leading cancer center with one of the most active ovarian cancer programs, our surgeons have a high level of expertise that sets them apart from many others. The MD Anderson physicians will carefully consider whether it is better to do surgery upfront or after chemotherapy.
Rare ovarian cancers
Many rare ovarian cancers have distinct molecular and clinical features. An accurate diagnosis is essential for getting the right care. The pathologists at MD Anderson are experts in diagnosing rare ovarian cancers. When patients are diagnosed with one of these rare cancers, they get care from gynecologic oncologists who specialize in that particular disease.
Precision medicine
We are leaders in studying ovarian cancer on the molecular level and translating research into advanced ways to find and treat the disease. Through our High-Risk Ovarian Cancer Screening Clinic and Gynecologic Cancer Genetics Clinic, we offer genetic testing for women with hereditary breast and ovarian cancer syndrome and other high-risk inherited conditions.
MD Anderson leads the nation in innovative research into the causes, prevention, detection and treatment of ovarian cancer, including rare ovarian cancers. In fact, we are one of the few cancer centers in the nation to house a prestigious federally-funded Ovarian Cancer SPORE (Specialized Program of Research Excellence) program. This means we offer a variety of clinical trials of new ovarian cancer treatments.
And, at MD Anderson you're surrounded by the strength of one of the nation's top comprehensive cancer centers. We have all the support and wellness services needed to treat not just the disease, but the whole person.
Going through cancer gives you an opportunity to see what you're made of.
Megan Silianoff
Survivor

What does ovarian cancer pain feel like?
Symptoms of ovarian cancer are so vague that roughly 80% of cases are diagnosed only after the disease has reached stage III or IV.
Abdominal pain is one of its top five symptoms. But what does ovarian cancer pain feel like? Does it ever come and go? And, when should you see a doctor?
We talked with Pamela Soliman, M.D., a surgeon who specializes in ovarian and other gynecologic cancers. Here’s what she shared.
What does ovarian cancer pain feel like?
Some patients describe it as a constant pain or a dull ache in their lower abdomen.
But many also report discomfort or bloating in their upper abdomen, even though the ovaries are situated much lower in the pelvis.
Does ovarian cancer pain ever come and go?
It can, but pain doesn’t have to be constant for it to ring an alarm bell. When pain lingers for more than two weeks and won’t go away with medication, that’s a big red flag.
So, if the pain doesn’t get better on its own after a couple of weeks, it’s important to let your doctor know.
What other conditions do patients tend to confuse with ovarian cancer pain?
- gas
- indigestion
- GERD/acid reflux
- gallstones
- menstrual cramps
What are the most common ovarian cancer symptoms?
In addition to abdominal pain or discomfort, there are four others. Some people use the acronym “BEACH” to help them remember.
B is for Bloating
Pay attention if it seems fairly consistent and can’t be explained by eating foods known to produce gas, such as beans or broccoli. Tumors use some of the food you eat to nourish themselves, too, so your face may get thinner while your abdomen gets larger.
E is for Early satiety
You can’t eat as much as you normally would because you feel full quickly, but your clothes still feel tight and you’re gaining weight.
A is for Abdominal pain or discomfort
This could also feel like acid reflux, gas, menstrual cramps, ovary pain or pressure in the pelvis.
C is for Changes in bowel or bladder habits
Diarrhea is one of the most commonly reported symptoms of ovarian cancer. But you could also be constipated or feel the urge to urinate more often.
H is for Heightened fatigue
Take note if you feel exhausted even after getting enough sleep, especially if you’re too tired to engage in normal daily activities.
What’s the one thing you want people to know about ovarian cancer pain?
A lot of women have ovarian cancer symptoms, and then they go to the doctor, and it turns out they’re fine. But if your symptoms persist, please let us know. Don’t just assume everything’s OK.
We rely on our patients to tell us what they’re experiencing so we can order additional testing if needed. So, I can’t emphasize enough how important it is to advocate for yourself.
Request an appointment at MD Anderson online or call 1-877-632-6789.
Treatment at MD Anderson
MD Anderson ovarian cancer patients can get treatment at the following locations.

Ascites: 8 things to know about this ovarian cancer symptom
Ascites is the accumulation of fluid in the peritoneal space of the abdomen. Though it can be caused by several non-cancerous conditions, when seen alongside a pelvic mass, ascites is often a sign of peritoneal carcinomatosis, a classic symptom of advanced-stage ovarian cancer.
So, what causes ascites? Can it be treated? And, does it ever develop anywhere else?
We went to Travis Sims, M.D., a gynecologic oncologist specializing in ovarian and other gynecologic cancers. Here are eight things he shared about this ovarian cancer symptom.
How is the word ascites pronounced?
It’s pronounced “as-SYE-teez.”
What causes ascites?
Ascites are thought to be caused by a combination of:
- high levels of fluid production in the peritoneal cavity
- an obstructive process involving the peritoneal lymphatic system and increased vascular permeability –– or the exchange of fluids between organs and tissue.
It is largely caused by increased levels of a protein called vascular endothelial growth factor (VEGF).
Does ascites ever develop anywhere else in the body?
Ascites, by definition, is the pathological accumulation of fluid in the peritoneal cavity. But fluid can also accumulate in other parts of the body. If fluid accumulates around your lungs, for instance, that is called a pleural effusion.
Are any other cancers associated with the development of ascites?
Several, but the ones I am most familiar with are:
- ovarian cancer
- fallopian tube cancer
- primary peritoneal cancer
- endometrial cancer
Can any conditions other than cancer ever cause ascites?
Yes. Chronic hepatitis, liver failure, congestive heart failure, and pancreatitis, to name but a few.
How is ascites typically diagnosed?
In our patients, we often discover ascites during a physical exam.
Ascites can cause the abdomen to become very distended. We can often perceive a “fluid wave,” or movement of liquid beneath the surface when assessing patients with it. Patients may also complain of shortness of breath, abdominal tenderness and pain, loss of appetite, indigestion, fatigue, constipation, or back pain.
We can confirm the presence of ascites with imaging, such as an abdominal ultrasound or a CT scan of the abdomen.
Can ascites be treated?
Yes. Patients can undergo a procedure called therapeutic paracentesis, in which a needle is inserted into the abdomen to drain off the fluid. This can relieve their immediate discomfort, but the fluid tends to return without treatment of the underlying cancer.
In patients with advanced or recurrent cancer that is no longer responding to treatment, a catheter can be placed in their abdomen. This allows the patient to drain off fluid whenever they are uncomfortable or having painful symptoms.
What’s the one thing you want people to know about ascites?
Unfortunately, ovarian cancer is a disease that we cannot screen for. That’s why it is important to pay attention to your body. If you have unexplained abdominal distention, pain, or any of the other symptoms mentioned above persistently for a couple of weeks, please talk to your doctor.
Request an appointment at MD Anderson online or call 1-877-632-6789.
Featured Articles

The pill and cancer: Is there a link?

Stage III ovarian cancer survivor: Don’t ignore your symptoms
Ovarian cysts and cancer: Is there a connection?
Ovarian cancer stages: How they are determined
Researchers explore new possibilities for ovarian cancer treatment

Breast and ovarian cancer diagnoses help clinical dietitian empathize with patients

Ovarian cancer survivor finds support in colleagues, students

How is ovarian cancer treated?
Clinical Trials
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
