request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Rectal Cancer
Get details about our clinical trials that are currently enrolling patients.
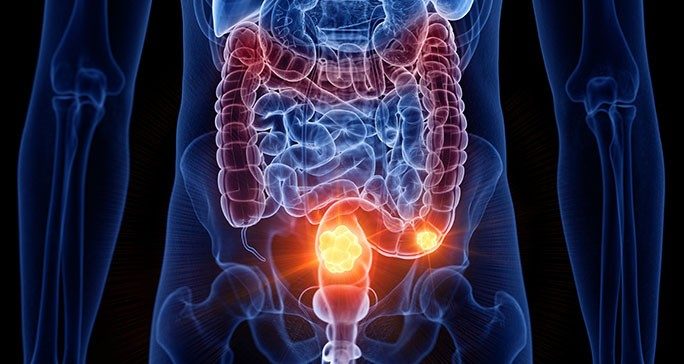
View Clinical TrialsRectal cancer is cancer that starts in the rectum. The rectum consists of the last few inches of the large intestine. It connects to the colon on one end and the anus on the other.
Rectal cancer is cancer that starts in the rectum. The rectum consists of the last few inches of the large intestine. It connects to the colon on one end and the anus on the other.
The body moves waste, called stool, through all three structures before expelling it through the anus.
Rectal cancer and colon cancer start the same way and share many risk factors and symptoms. The two diseases are often referred to together as colorectal cancer. There are some significant differences between the two diseases, though.
Rectal cancer that has not spread to distant parts of the body is also treated with surgery. For some patients, radiation therapy and chemotherapy are used to decrease the risk of the cancer returning after treatment. In some cases, radiation therapy and chemotherapy can reduce the need for surgery. Rectal cancer surgery can be more complex than colon cancer surgery.
How does rectal cancer start?
Rectal cancer usually starts as a polyp. Polyps are small overgrowths in the tissue lining the colon or rectum. Polyps are not cancer.
Some polyps can turn into cancer over time. Most of these polyps are adenomas, which begin in mucus-producing gland cells that line the intestine and other organs. Adenomas are considered pre-cancerous growths.
It can take several years for an adenoma to develop into cancer. When it does, the cancer is called an adenocarcinoma. This is the most common type of rectal cancer.
There are other, rarer types of rectal cancer, including rectal neuroendocrine tumors and rectal cancers that involve the cells of the anus.
There are more than 150,000 combined colon and rectal cancer diagnoses in the United States each year. As of 2018, the disease’s five-year survival rate is about 65%. This figure does not include people diagnosed more recently, who could benefit from new treatments.
Young-onset colorectal cancer
Historically, most cases of colorectal cancer have been in people over age 55. In recent years, there has been an increase in diagnoses among people under age 55. MD Anderson’s Young-onset Colorectal Cancer Program offers specialized services for these patients. Services include fertility care, genetic testing and counseling, as well as support groups for young adults.
Rectal cancer screening
Most precancerous polyps produce few, if any, symptoms, so it is important to get screened regularly for rectal cancer. Rectal cancer screenings allow your doctor to find and remove polyps before they turn into cancer. Screening can prevent most cases of rectal cancer cases. It can also catch rectal cancer early, when treatments are more likely to be successful.
- Learn more about rectal cancer screenings
Rectal cancer risk factors
Anything that increases your chance of getting colorectal cancer is a risk factor. Colorectal cancer risk factors include:
- Age: More than 75% of colorectal cancer cases are diagnosed in patients age 55 and older. The median age at diagnosis is 66 years old. However, the rate of colorectal cancer diagnosed in adults less than 55 years old has increased in recent years.
- Race: African Americans have the highest rate of colorectal cancer among all racial groups in the United States.
- Family history: People whose relatives have had colorectal cancer or colorectal polyps have an increased risk of colorectal cancer.
- Inflammatory bowel disease: Patients with conditions that include Crohn’s disease or chronic ulcerative colitis are more likely to develop colon cancer. Learn more about inflammatory bowel disease and colorectal cancer.
- Personal history of colorectal cancer or polyps: People who have previously had colorectal cancer or colon polyps are at an increased risk of developing colorectal cancer.
- Hereditary cancer syndromes: Some genetic changes can be inherited and increase your risk for certain types of cancer. Inherited syndromes including hereditary nonpolyposis colorectal cancer, or Lynch syndrome, and familial adenomatous polyposis may put you at higher risk for developing colorectal cancer. Learn more about hereditary cancer syndromes.
- Diet: A diet heavy in red meat, processed meats, or meats cooked at very high heat can increase a person’s rectal cancer risk.
- Obesity: Obesity increases a person’s chance of developing many different diseases, including colorectal cancer.
- Sedentary lifestyle: A lack of movement and exercise is a risk factor for colorectal cancer.
- Cigarette smoking: Tobacco use, including cigarettes and chewing tobacco, is a colorectal cancer risk factor.
- Drinking too much alcohol: Heavy drinkers are at an increased risk for colorectal cancer.
For patients concerned about inherited family syndromes that cause colorectal cancer, we offer advanced genetic testing and counseling to help understand your risk.
Rectal cancer prevention
Lifestyle choices that may decrease your risk of getting rectal cancer include:
- Regular screening tests
- Staying at a healthy weight
- Regular exercise
- Eating a healthy diet with lots of fruits and vegetables
- Avoiding cigarette smoking
- Drinking alcohol only in moderation
Learn more about rectal cancer:
MD Anderson is #1 in Cancer Care
Cancer in the sigmoid colon: What it means when colon cancer is on the left side
The sigmoid colon is the part of the large intestine (colon) closest to the rectum. It absorbs water from stool and pushes the stool to the rectum and anus until it’s ready to be expelled when you use the bathroom.
Colorectal cancer is an umbrella term for colon cancer and rectal cancer. Studies have shown that colorectal cancer is more common in the sigmoid colon, which is on the left side, along with the descending colon and rectum. The rectum is also considered the left side even though it’s not part of the colon.
Gastrointestinal medical oncologist Kanwal Raghav, M.D., estimates that about 70% of colorectal cancers are diagnosed on the left side.
“It’s unclear why colon cancer starts in a particular location, although some explanations exist,” says Raghav. “However, left-side colon cancers are more common than right-side colon cancers.”
The colon starts at the cecum, which is on the right side. It goes up to the ascending colon, across the body to the transverse colon and down to the descending colon and sigmoid colon, which are on the left side.
We spoke with Raghav to learn more about the differences between left-side and right-side colon cancer. Here’s what he shared.
It’s common for left-side tumors to cause symptoms.
It's common for people with left-side colorectal cancer to have changes in their bowel habits or blood in their stool. People with right-side tumors often show fewer symptoms.
Left-side tumors and right-side tumors have different genetic characteristics.
Tumors that develop on the left side of the colon have more mutations of tumor-suppressing genes, like APC and TP53. These genes help prevent tumors from growing. Mutations in these genes make you more likely to develop certain cancers, including colon cancer.
Tumors that develop on the right side of the colon are more likely in people who have hereditary cancer syndromes. These include high microsatellite instability (MSI-high) – also referred to as DNA mismatch repair deficiency (dMMR) – and Lynch syndrome.
Left-side tumors are easier to detect during a colonoscopy.
During a colonoscopy, your doctor examines the walls and lining of your colon, including the sigmoid colon, by inserting a flexible scope into your rectum and around your large intestine. Doctors examine the left side first since it’s closer to where the scope is inserted. Colorectal cancer usually starts as a polyp in the colon or rectum.
Left-side tumors often present as polypoid lesions, which protrude into the lumen of the gastrointestinal tract and are easier to see. Colonoscopies are good at detecting these polyps, which is why getting this routine screening is so important.
Many polyps on the right side of the colon are sessile serrated adenomas. These are flat and harder to detect during a colonoscopy. Because of this, right-side colon cancers are often diagnosed at advanced stages and may be harder to treat.
Colonoscopy prep is important because your colon will need to be completely clean of any stool, so your doctor can easily see both the left and right side of your colon.
The side on which cancer develops helps determine your treatment.
Overall, left-side tumors have a better prognosis than right-side tumors. This is because colon cancer on the left side responds better to chemotherapy and targeted therapies, like anti-EGFR and HER2 drugs.
Right-side tumors tend to have more genetic mutations, which are often associated with more aggressive cancers. Right-side tumors are also harder to detect, so they’re often diagnosed when the disease is more advanced. Recently, immunotherapy has been effective in treating these cancers because the body can recognize the abnormal cells and attack them. Immunotherapy has helped improve the prognosis for patients with stage IV right-side colon cancer.
Your doctor and care team will work together to develop the best treatment plan for you.
Knowledge of left-side and right-side colon cancer leads to treatment advances.
We’ve been treating colorectal cancer for a long time. But only in the last four or five years have we really started to understand the differences between colon cancer that develops on the left side versus the right side. Before then, it wasn’t as commonly acknowledged.
Over the years, we have learned that colon cancer can’t be viewed as one disease. We’re now looking at it as a complex disease with many subtypes and trying to develop targeted and personalized therapies that can be used depending on the specific type people have. Slowly and steadily, we are moving the bar for personalized therapy in colorectal cancer. And I think the location of the cancer – left side versus right side, including the sigmoid colon – is a part of that.
Request an appointment at MD Anderson online or call 1-877-632-6789.

Anal cancer vs. colorectal cancer: What’s the difference?
Anal cancer and colorectal cancer both develop in the lower gastrointestinal tract, but these types of cancer differ in many ways.
We spoke with gastrointestinal radiation oncologist Emma Holliday, M.D., to learn more about the differences between anal cancer and colorectal cancer.
What parts of the lower digestive system do anal cancer and colorectal cancer affect?
Anal cancer affects the anal canal and anus.
Colorectal cancer affects the large intestine, including the cecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum.
What are the risk factors for anal cancer and colorectal cancer?
The most common cause of anal cancer is the human papillomavirus (HPV), particularly types 16 and 18, which cause 90% of anal cancers and precancers.
Other less common risk factors for anal cancer include:
- HIV infection
- smoking
- a weakened immune system caused by medicines taken for organ transplants, autoimmune diseases or other conditions
You’re at greater risk for colorectal cancer if you have:
- history of precancerous polyps
- genetic syndromes, such as familial adenomatous polyposis or Lynch syndrome
- inflammatory bowel diseases, such as Crohn’s or ulcerative colitis
Other risk factors for colorectal cancer include:
- a diet high in processed meats and low in fruits and vegetables
- lack of physical activity
- being overweight
What are the symptoms of anal cancer and colorectal cancer?
There are some overlapping symptoms. Anal cancer and colorectal cancer can both cause:
- weakness or fatigue
- unexplained weight loss
- belly or pelvic pain
- changes in bowel habits, such as:
- anal or rectal bleeding
- constipation
- diarrhea
- urgent bowel movements
- difficulty controlling bowel movements
Symptoms specific to anal cancer include:
- itching or pain around the anus
- lumps in or around the anus
- pain in the anus when passing bowel movements
Symptoms specific to colorectal cancer include:
- abdominal pain
- bloating
- a feeling that the bowels don’t empty completely
Anal cancer and colorectal cancer often have symptoms that can be mistaken for other conditions. For example, anal cancer is often misdiagnosed as hemorrhoids. This is why regular cancer screenings are so important. Be sure to get a colonoscopy or seek a second opinion if your symptoms don’t resolve in a few weeks.
How are anal cancer and colorectal cancer diagnosed?
Anal cancer and colorectal cancer can be diagnosed at regular screening colonoscopy exams, even before a patient develops symptoms.
If you develop symptoms in between screening colonoscopies, a diagnostic colonoscopy can be performed to look inside the anal canal, rectum and colon to check for cancer. A biopsy can be performed to determine whether or not cancer is present.
How are anal cancer and colorectal cancer treated?
The most common type of cancer cell causing anal cancer is squamous cell carcinoma. It responds well to and is most commonly treated with radiation therapy and chemotherapy delivered together. We can sometimes use a procedure called a local excision to remove very small and early-stage anal cancers that have not metastasized to the lymph nodes and do not invade the sphincter. This represents a minority of anal cancer cases.
Treatment options for colorectal cancer differ depending on the location of the cancer. Tumors in the colon can be treated with surgery alone, or chemotherapy may be given before or after surgery, depending on the size of the tumor and whether or not the cancer has spread to lymph nodes.
Tumors in the rectum have a higher chance of coming back after surgery, so rectal cancer is often treated with chemotherapy and/or radiation therapy before surgery. Patients with rectal cancer have several treatment options, depending on the location of the tumor in the rectum, its size and whether the cancer has spread to lymph nodes. These treatment options are:
- chemotherapy followed by surgery and no radiation if the tumor shrinks enough after chemotherapy
- chemotherapy followed by radiation and no surgery if there is no cancer left after chemotherapy and radiation
- chemotherapy, radiation and surgery if there is a high risk of recurrence
Getting the right diagnosis is the best way to ensure you get the correct treatment. And with early detection, both anal cancer and colorectal cancer can be successfully treated.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.

What does colon cancer pain feel like?
Most people diagnosed with colon cancer won’t mention pain as one of their symptoms. But when they do, how do they describe it? What does the pain caused by colon cancer actually feel like? And, does it tend to occur only in certain locations?
We went to gastrointestinal medical oncologist Benny Johnson, D.O., for insight. Here’s what he shared.
What does colon cancer pain feel like?
Most patients who come to our clinic with pain as a symptom describe it as an intermittent crampy feeling in their abdomen.
But it’s important to note that many of our patients say that they don’t have any pain at all. Instead, they might report an odd sensation of fullness in their abdomen or notice some blood in their stool.
How common is pain as a sign of colon cancer?
Not very. I’d say only about 15% of our patients mention pain as one of their colon cancer symptoms.
Does colon cancer pain always occur in a particular spot?
No. But patients with more advanced colon cancer that has spread to the liver sometimes notice a sense of fullness or bloating in the upper right side of their abdomen.
And, depending on where a tumor is located, it can also cause an obstruction, or a blockage in the colon, which can cause severe pain. Those typically occur on the lower left side of the abdomen.
But again, a lot of our colon cancer patients don’t report pain as a symptom. They just see a little blood on the toilet paper and get referred for a colonoscopy.
To be clear here, are we talking about actual pain or just significant discomfort?
One person’s painful is another person’s uncomfortable. So, there’s a wide spectrum. And it’s very subjective.
Primary tumors located in the colon — and even those that have spread to other organs — can cause real pain. And patients who have a full-blown obstruction can be in a lot of pain. But those who don’t might just experience some mild discomfort or even an occasional crampy feeling.
What other conditions do patients tend to confuse with colon cancer pain?
- constipation
- hemorrhoids
- gas
- spicy foods
- irritable bowel syndrome (IBS)
If you’re experiencing abdominal pain or discomfort for more than a couple of weeks, talk to your doctor and make a plan. Try traditional interventions first to address the most common complaints and see if that resolves them. If not and your symptoms persist, please follow up.
What’s the one thing you want people to know about pain as a symptom of colon cancer?
Colon cancer is not just a diagnosis of the elderly anymore. More and more young people are being diagnosed with colon cancer — even in their late 30s and early 40s. They’re also presenting with more advanced cases of disease. That’s why the recommended age for people’s first colon cancer screening with a colonoscopy was recently lowered from age 50 to 45.
That’s also why it’s so important to be aware of your body. If something doesn’t feel right, see your doctor.
Don’t chalk up your symptoms to something like hemorrhoids or constipation, especially if you’ve also noticed a change in your bowel habits, such as:
- more frequent bowel movements
- feeling like you’re not emptying your bowels completely
- your stool shape or consistency has changed and/or
- rectal bleeding
Even a new, vague sense of discomfort is not unreasonable to investigate since a growing number of people are getting diagnosed with colon cancer at a younger age. So, listen to your body and take your symptoms seriously.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Why choose MD Anderson for rectal cancer treatment?
At MD Anderson's Gastrointestinal Center, your rectal cancer treatment is personalized to provide the best outcomes, while focusing on your quality of life. We offer leading-edge treatments for rectal cancer, including advanced minimally invasive surgeries that provide successful treatment with less impact on you and sphincter-preserving surgeries, eliminating the need for a colostomy bag.
Multidisciplinary team approach
Rectal cancer treatment at MD Anderson is provided by a team of experts, including medical oncologists, surgeons, radiation oncologists, gastroenterologists, radiologists, clinical nurses and mid-level providers. They discuss your case and develop a treatment designed to attack your cancer while minimizing side effects.
Supplementing your clinical care, MD Anderson also provides nutrition counseling, pain management, psychological support, wound management and other services.
Younger patients can also receive specialized support through our Young-onset Colorectal Cancer Program. This program offers services like genetic counseling and testing, fertility preservation and young-adult support groups.
In addition, our advanced knowledge in cancer genetics can help diagnose and treat inherited family syndromes that may increase your risk of rectal cancer. This expertise also helps us work with you to plan the most effective treatment for your specific condition.
For patients who have been successfully treated for rectal cancer and are being monitored for recurrence, our tumor Intercept program also offers circulating tumor DNA testing. Patients may even be matched with clinical trials to monitor for or prevent the cancer’s return. This test can help doctors diagnose a recurrence long before it shows up in an imaging exam.
Leading-edge advancements
As one of the world’s largest cancer research centers, MD Anderson is a leading center for the investigation into new methods of rectal cancer treatment and diagnosis. Through our clinical trials, this research can give patients access to treatments and procedures not found anywhere else.
And at MD Anderson you'll also be surrounded by the strength of one of the nation's largest and most experienced cancer centers. From support groups to counseling to integrative medicine care, we have all the services needed to treat not just the disease, but the whole person.
When it comes to dealing with cancer, it is what is it and you’ve got to seek the best care that you can.
Drew Long
Survivor

14 common anal cancer questions
Anal cancer can be hard to talk about. And, even when it is talked about, anal cancer is often mistaken for — or lumped together with — colorectal cancer, instead of being recognized as the distinct type of cancer that it is.
But talking about anal cancer is important, both for educational purposes and to allow those affected by the disease to feel less alone — especially with rates of HPV-related anal cancer climbing. The topic may be a bit uncomfortable, but it isn’t without hope. Most early-stage anal cancers can be cured with chemoradiation alone.
Here are some common anal cancer questions I hear.
What is anal cancer, and how does it differ from colorectal cancer?
Anal cancer is a completely different disease with a different biology. It’s also treated differently.
Colorectal cancers tend to be adenocarcinomas, which arise from the glands in the gastrointestinal tract. Anal cancers, on the other hand, tend to be squamous cell carcinomas, which develop on the surfaces lining the body.
Anal cancer is also primarily caused by HPV infection; colorectal cancer is not.
The two cancers are also treated differently. The standard treatment for anal cancer is chemoradiation alone if the cancer hasn’t spread. But colorectal cancer may be treated with some combination of chemotherapy, radiation and surgery, depending on its location.
Who is most at risk for developing anal cancer?
In the United States, women are twice as likely as men to develop anal cancer. People who are immunocompromised — whether it’s due to cancer treatment, diseases like HIV, immunosuppressive drugs for autoimmune diseases or a prior organ transplant — are also at higher risk.
Still, it’s important to note that anal cancer is not very common. Only about 9,000 people are diagnosed with it a year in the United States.
Can anal cancer be prevented?
The majority of anal cancer cases are caused by exposure to the human papillomavirus (HPV). HPV is the most common sexually transmitted disease. A lot of people never even realize they’ve been exposed to HPV, because the body usually clears it naturally. Only a very small fraction will develop HPV-related cancers like anal cancer.
That’s why we highly recommend getting vaccinated against HPV, ideally at around age 11 or 12, or before the onset of sexual activity. That’s when you’ll derive the most benefit from it as a cancer-preventing vaccine. As early as age 9 is reasonable, though, and everyone up to age 26 should get the HPV vaccine. If you’re age 27-45 and have been sexually active, there may still be some benefit to getting the HPV vaccine. Talk to your doctor to see if it’s right for you.
The vaccine has proven to be safe and effective at preventing infection from the nine known strains of HPV that are linked to cancer and genital warts. In addition to preventing most anal cancers, the vaccine also prevents most cervical, penile, vaginal and vulvar cancers, plus HPV-related throat cancers.
How is anal cancer typically diagnosed? Are anal cancer symptoms ever mistaken for other things?
Anal cancer is often detected initially after patients experience certain symptoms, such as:
- pain during a bowel movement
- a little bleeding during or after a bowel movement
- a change in bowel habits
That’s normally when people consult their doctors: when their symptoms persist, increase or get worse.
Can hemorrhoids cause anal cancer?
No. Sometimes, people have what they think is a hemorrhoid that won’t go away, and it turns out to be anal cancer. But hemorrhoids and anal cancer are two separate things. And neither one causes the other.
Is bowel leakage ever a sign of anal cancer?
No. Not usually. But anal bleeding and discharge can be.
What does anal cancer look like? Is it ever a lump you can see?
Occasionally, someone will be able to feel a lump or a mass through the skin. But anal cancer is not typically visible from outside the body. It tends to form internally, so the more common ways to see it usually are through an endoscope or on a scan.
How fast does anal cancer grow?
Anal cancer is a fairly slow-growing disease. It probably takes several years to develop.
What can patients expect during their first appointment for anal cancer?
At MD Anderson, you’ll meet with a team of specialists, including a medical oncologist, a radiation oncologist, and a surgical oncologist. All of them will specialize in treating anal cancer.
You’ll go over your medical history. At some point, you’ll likely have a proctoscopy, a type of internal examination conducted with a scope. It’s similar to a colonoscopy but doesn’t require anesthesia or the same type of preparation. It can usually be performed in a doctor’s office.
You’ll also have some imaging studies done to fully assess the extent of the cancer, and blood tests to help determine the most appropriate chemotherapy dosages.
What treatments are available for anal cancer?
Most patients with anal cancer that hasn’t spread can be cured with chemoradiation alone. That’s when chemotherapy is given in tandem with radiation therapy to make the radiation more effective.
If the cancer comes back, we’ll do surgery. We do everything we can to prevent that, though, because it often requires a permanent ostomy. We’ll use immunotherapy and other systemic therapies if other organs are involved.
One thing we do differently here at MD Anderson involves the selection of chemotherapy agents and their dosages. We may dose patients differently than your local doctor normally would. What that means is that if you come to MD Anderson, your likelihood of survival will be about the same, but your treatment can be much less toxic. And that means you’ll likely have fewer side effects and a better quality of life.
Can anal cancer be cured?
We cure over 80% of our patients with stage I or stage II anal cancer, and about 60% of our patients with stage III anal cancer.
Stage IV anal cancer usually cannot be cured, but it can be treated.
What lifestyle changes can anal cancer patients expect after treatment?
Patients typically experience side effects for up to six months after treatment ends. But it takes some patients up to a year before they start feeling more like their old selves.
Tender, sensitive skin is one of the most common short-term side effects of radiation therapy. For that, we normally recommend moisturizing creams and topical ointments.
Long-term side effects may include differences in sexual, bowel or bladder function. We educate patients about how to manage those.
What are the latest research advances for anal cancer?
We’ve developed an in-house circulating DNA blood test to detect the presence of HPV and identify patients at high risk for recurrence.
We’re also developing an immunotherapy clinical trial for these patients, which would be the first in the world to use circulating HPV-positive tumor DNA as a prerequisite for study entry.
What advice would you give to newly diagnosed anal cancer patients?
Where you go first for anal cancer treatment matters. You want to make sure you’re going someplace with a lot of experience in treating anal cancer.
MD Anderson is one of the leading institutions in the United States for treating patients with anal cancer. Our focus is not only on curing the cancer but on personalizing the treatment so it’s less toxic than the standard therapy you might otherwise get from your local oncologist.
We want our patients’ quality of life to remain as high and functional as possible, even after treatment. So, we go out of our way to create treatment plans that will cause fewer long-term disruptions to patients and their families.
Request an appointment at MD Anderson online or call 1-877-632-6789.
Treatment at MD Anderson
Rectal cancer is treated in our Gastrointestinal Center.
Featured Articles
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.





