The Science and Benefits of Proton Therapy
- Treatment Options
- Ablation Therapy
- Angiogenesis Inhibitors
- Awake Craniotomy
- Brachytherapy
- Breast Reconstruction Surgery
- CAR T Cell Therapy
- Chemotherapy
- Cryoablation
- High-Intensity Focused Ultrasound (HIFU)
- Histotripsy
- Hyperthermic Intraperitoneal Chemotherapy
- Immunotherapy
- Immune Checkpoint Inhibitors
- Integrative Medicine
- Interventional Oncology
- Laser Interstitial Thermal Therapy (LITT)
- Microwave Ablation
- Minimally Invasive Surgery
- MR-Linac Radiation Therapy
- Palliative Care
- Proton Therapy
- Radiation Therapy
- Radiofrequency Ablation
- Stem Cell (Bone Marrow) Transplantation
- Stereotactic Body Radiation Therapy
- Stereotactic Radiosurgery
- Surgery
- Targeted Therapy
- Theranostics
- Y90 Radioembolization
Proton Therapy
Proton therapy is similar to traditional radiation therapy, but it uses a different type of energy and is much more accurate at targeting tumors.
Standard radiation therapy uses X-ray beams made up of photons, which are tiny particles that transmit light. Photons deposit energy as they travel to the tumor, into the tumor itself and beyond the tumor. This results in side effects from damage to nearby healthy tissues or organs. The dose delivered to the tumor must be limited to minimize these side effects.
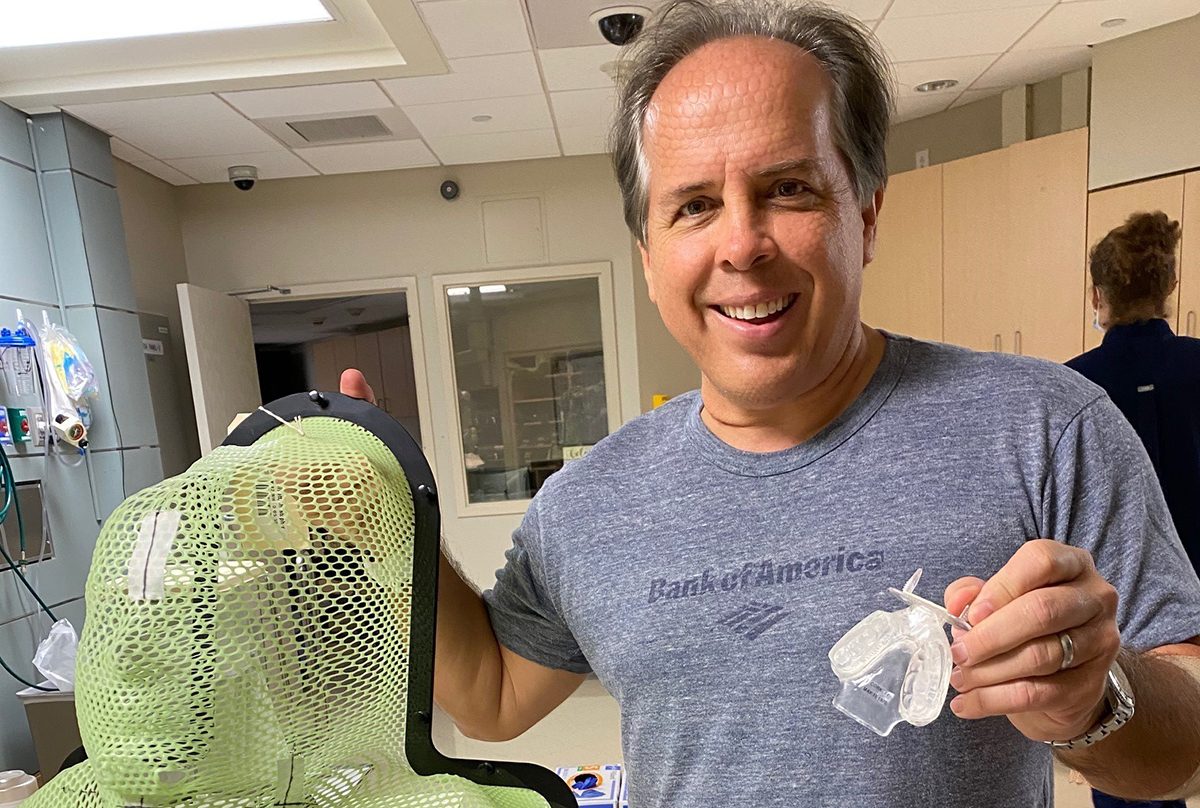
Proton therapy uses protons, which are positively charged particles found in the nucleus of an atom. Proton beams enter the body with a low dose of radiation (“entrance dose”). The dose increases as it approaches the target area and deposits its maximum radiation directly to the tumor before stopping. There is no “exit dose” beyond the tumor. This means the tumor can be targeted more precisely, usually within one millimeter, and allows for the delivery of a more powerful dose of radiation.
Pencil Beam and Intensity Modulated Proton Therapy
Pencil beam scanning, also known as spot scanning, is a proton therapy technique used to treat complex tumors. Powerful magnets direct thousands of ultra-fine proton beams from multiple directions toward the tumor, creating a protective “U” shape around healthy tissue and avoiding sensitive areas. MD Anderson’s Proton Therapy Center currently uses pencil beam scanning to treat cancers of the prostate, brain, base of the skull and eye.
The Proton Therapy Center is also a leader in Intensity Modulated Proton Therapy. This treatment is best used to deliver a potent and precise dose of protons to complex or concave-shaped tumors that may be next to the spinal cord or embedded in the head and neck or skull base, including nasal and sinus cavities; the oral cavity; salivary gland; tongue; tonsils; and larynx.
Proton Therapy Center
Want to read more about proton therapy? Visit our Proton Therapy Center site.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Featured Articles

Proton therapy helps survivor overcome two cancer diagnoses

Prostate cancer survivor grateful for precise treatment during proton therapy

Proton therapy saved my ability to taste during treatment for tongue cancer

Squamous cell carcinoma survivor thankful he chose proton therapy
Squamous cell carcinoma survivor grateful for proton therapy
request an appointment online.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
