Phantosmia: 8 things to know about olfactory hallucinations
Phantosmia is the scientific term for olfactory hallucinations — that is, the perception of odors that do not exist. It’s like detecting the aroma of coffee brewing at home when no one is making it, or smelling the scent of roses at work when no one is wearing perfume or has flowers at their desk.
Here, I’ll explore what causes phantosmia, how it’s treated, and if it can ever be a sign of cancer.
Phantosmia is one of many possible olfactory conditions
The first thing to know about phantosmia is that it’s just one of several conditions that can affect the sense of smell.
- Phantosmia is when you detect odors that aren’t actually there.
- Cacosmia is when you smell something unpleasant that isn’t actually there.
- Hyposmia is when you smell things accurately, but at a lower intensity.
- Anosmia is the complete loss of your sense of smell.
Hyposmia is likely the most common of these because it occurs when people have colds or allergies.
A brief overview of olfaction
The second thing to know is that the sense of olfaction is a complicated and intricate mechanism. So, it’s helpful to understand how it works.
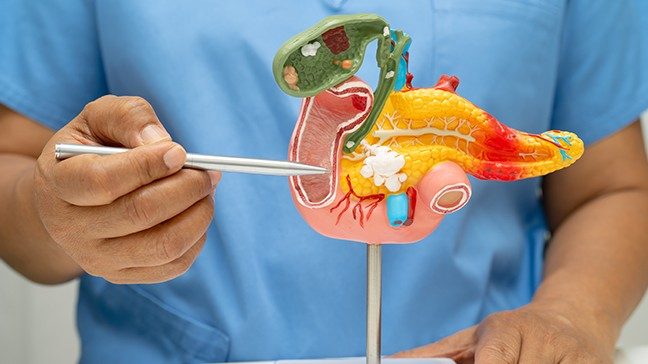
Aromas are generated by airborne scent molecules that emanate from a given substance. When inhaled, they land on special receptors in the nasal lining, or mucosa. From there, they are carried across the nasal cavity, through the cribriform plate (a structure at the skull base that looks like a sieve), and into the frontal lobe of the brain to the olfactory bulb, where we actually perceive odors.
So, what causes phantosmia?
Anything that obstructs the nose can theoretically prevent scent molecules from reaching the olfactory area I just described. So, it’s pretty common for blockages to cause hyposmia or anosmia. But it’s far less common for those blockages to cause phantosmia.
You probably won’t be able to smell things normally, for instance, if you develop nasal polyps or a stopped up nose. Some of the secretions there may also give you an altered sense of smell, as if you’re smelling the mucus itself. But it’s pretty rare for an obstruction to cause phantosmia.
Generally speaking, the most common causes of phantosmia are:
- Viral infections, such as a really nasty cold or COVID-19
- Neurodegenerative disorders, such as multiple sclerosis
- Seizure disorders, such as epilepsy
- Head injury, which could be from an auto accident, sports-related concussion or other trauma
- Migraine headaches, which can also cause visual hallucinations, known as “auras”
Is phantosmia ever a sign of cancer?
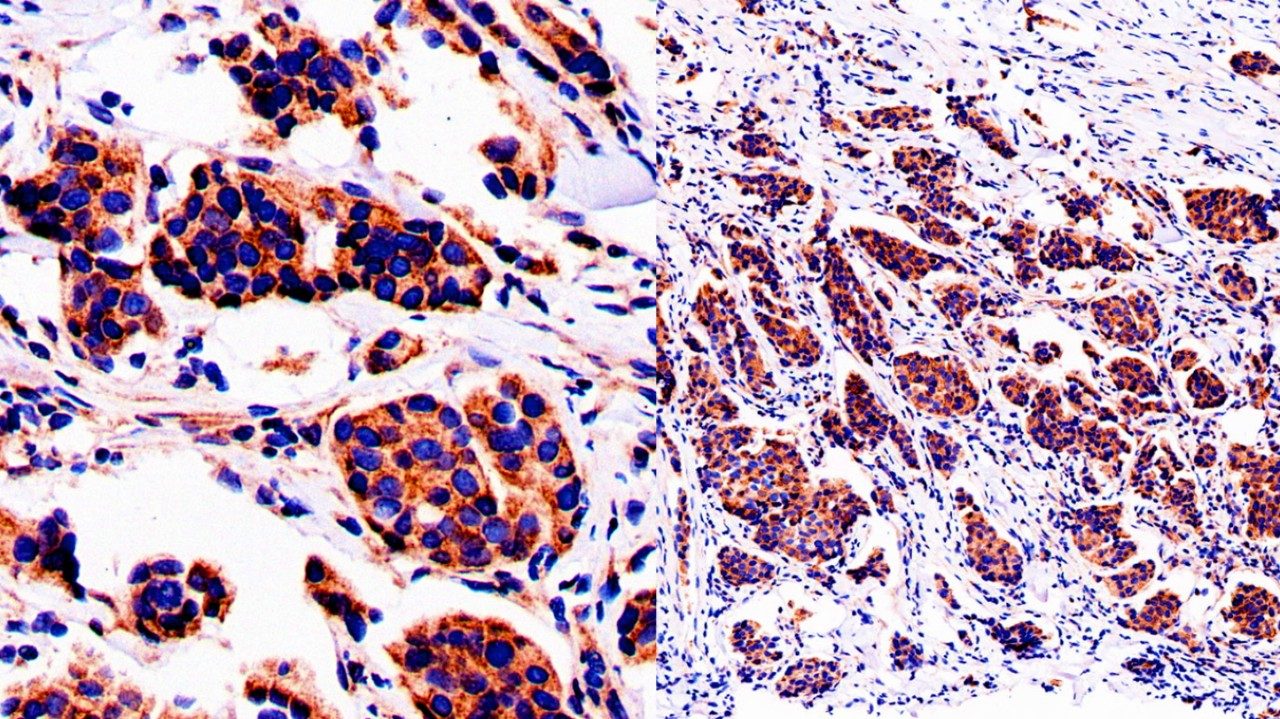
Occasionally, tumors do alter the anatomy of the olfactory region, which can result in phantosmia as a symptom. But I don’t want anyone worrying about this. Statistically speaking, phantosmia is far, far more likely to be caused by something else.
Rarely, phantosmia does happen due to a tumor, such as an olfactory groove meningioma, a type of brain tumor that’s usually benign. Tumors may also spread to the olfactory grooves from somewhere else. The nasal and sinus areas are located right below the skull base, while the brain is located just above it. So, theoretically, the problem could originate from either of those directions.
How art is shaping the patient experience at MD Anderson
Intrathecal chemotherapy: 10 questions, answered
Facing a pediatric brain tumor with a cheerful spirit
How to talk to your children about vaping
Phantosmia: 8 things to know about olfactory hallucinations
|
$entity1.articleCategory
|
|---|
|
$entity2.articleCategory
|
|
$entity3.articleCategory
|
|
$entity4.articleCategory
|
|
$entity5.articleCategory
|
|
$entity6.articleCategory
|
Find stories by topic
Find out everything you need to know to navigate a cancer diagnosis and treatment from MD Anderson’s experts.
Read inspiring stories from patients and caregivers – and get their advice to help you or a loved one through cancer.
Get MD Anderson experts’ advice to help you stay healthy and reduce your risk of diseases like cancer.
Learn how MD Anderson researchers are advancing our understanding and treatment of cancer – and get to know the scientists behind this research.
Read insights on the latest news and trending topics from MD Anderson experts, and see what drives us to end cancer.
Find out what inspires our donors to give to MD Anderson, and learn how their generous support advances our mission to end cancer.