request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Pancreatic Cancer
- Pancreatic Cancer Treatment
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsPancreatic Cancer Treatment
Treatment at MD Anderson's Gastrointestinal Center combines groundbreaking research and the most up-to-date technology with a multidisciplinary team approach, to craft a care plan specific to your individual needs.
At MD Anderson, pancreatic cancer treatment plans are based on whether or not a tumor can be surgically removed or resected. Most pancreatic cancers are diagnosed after they’ve already spread beyond the pancreas, but about 20% of pancreatic tumors are localized to the pancreas and are resectable. Whether or not a tumor is resectable, patients’ treatment plans usually vary. Typically, patients require more than one type of therapy provided by a multidisciplinary team of doctors.
Some therapies are the current standard-of-care, while others are being tested in clinical trials. Clinical trials are critical for advancing pancreatic cancer care and improving survival outcomes. They are supported by our pancreatic cancer research.
One or more of the following therapies may be recommended to treat the cancer or help relieve symptoms.
Pancreatic cancer treatment is impacted by resectability
Surgery is the only treatment that can cure pancreatic cancer, but is an only option for about 20% of cases. This means that it’s important to define whether a patient may benefit from surgery at the time of pancreatic cancer diagnosis, and reserve surgery only for when it may provide clinical benefit.
Because of this, MD Anderson doctors use a contemporary staging system, called resectability staging, to plan a patient’s treatment. This type of staging classifies pancreatic cancers into three groups, based on whether or not they can be removed with surgery. A patient’s potential treatment plan varies depending on the resectability staging of their pancreatic cancer.
Resectable
The cancer is confined to the pancreas, or has only spread to immediately nearby tissue, and the tumor can be removed entirely with surgery. This typically includes pancreatic cancers that are stage I and II. Patients with resectable pancreatic cancer may:
- Go straight to surgery.
- Receive chemotherapy prior to surgery.
- Receive radiation and chemotherapy prior to surgery.
Borderline resectable
The cancer has reached nearby blood vessels, but it has the potential to be removed with surgery. This typically includes some stage II and III cancers. Before surgery, patients with borderline resectable pancreatic cancer often receive chemotherapy and may subsequently receive radiation. After these initial therapies, patients are then evaluated to determine whether their tumor can be completely removed with surgery.
Unresectable
The cancer cannot be removed by surgery. This stage is divided into locally advanced and metastatic.
- Locally-advanced: The cancer is still largely confined to the pancreas and surrounding organs, but has grown into or is surrounding major blood vessels. This typically includes many stage III cancers. Patients with locally-advanced, unresectable pancreatic cancer always receive chemotherapy first and then are considered for radiation therapy. Depending on the size and placement of the tumor, higher than normal doses of radiation (dose-escalation) may be used during treatment.
- Metastatic: The cancer has spread to distant organs and can’t be completely removed. Patients with metastatic pancreatic cancer are treated with chemotherapy if it can be given safely based on patient’s tolerance. Radiation therapy is sometimes used to relieve symptoms associated with their cancer.
Pancreatic cancer surgery
The main surgical approaches used to treat pancreatic cancer are:
- Potentially curative: Attempt to treat pancreatic cancer by removing it.
- Palliative: Attempt to relieve symptoms, like a blocked bile duct or bowel.
Potentially curative surgical techniques
When pancreatic cancer is confined to the pancreas, and sometimes when it has spread only to nearby areas, the tumor can be removed with surgery. Complete removal of the tumor with surgery is often the best chance at curing pancreatic cancer. Partial removal of tumors doesn’t help patients live longer, so surgery is only done if the cancer can be removed entirely.
The most common technique used to remove a pancreatic tumor is called a pancreatoduodenectomy, or, more commonly, the Whipple procedure. This operation removes parts of the pancreas, intestine, nearby lymph nodes, gallbladder, bile duct and sometimes parts of the stomach.
The pancreas is located next to important blood vessels that supply blood to the liver and drain blood from the intestine. Often, cancer in the pancreas spreads into these vessels. If the pancreatic tumor cannot be completely separated from these blood vessels, many surgeons considered it unresectable. However, at MD Anderson the surgeon will often remove the tumor and reroute the affected vessels. This is called vascular resection and reconstruction and is performed during the Whipple procedure. These complex operations are potentially curative and are performed in about half of patients with localized pancreatic cancer who undergo surgery at MD Anderson.
Whether or not vascular resection and reconstruction is necessary, the Whipple procedure is a major operation that carries a high risk of complications, even when it is performed by experienced surgeons. Studies have shown this procedure is more successful and has less risk when it’s performed at a major cancer center by doctors with extensive experience in the procedures. Learn more about what makes MD Anderson surgeons some of the most experienced and skilled in the nation.
Palliative surgical operations
In many cases, cancer cannot be completely removed because it has spread too far beyond the pancreas or into major blood vessels. For these patients, surgery is sometimes used to help relieve symptoms of pancreatic cancer. Blockage of the bile duct is the most common symptom of pancreatic cancer that is treated with surgery. Blockages can cause bile to leak into surrounding organs, leading to pain and digestive problems. There are two techniques used to relieve this symptom:
- Stent placement: An endoscope is used to insert metal tubes (called stents) that help keep the bile duct open. This is often done during endoscopic retrograde cholangiopancreatography (ECRP).
- Bypass operations: The flow of bile is re-routed from the bile duct directly to the intestine, bypassing the pancreas. Bypass operations can provide longer-lasting relief, but have longer recovery periods than stent replacements.
Chemotherapy for pancreatic cancer
Chemotherapy drugs kill cancer cells, control their growth or relieve disease-related symptoms. Chemotherapy may involve a single drug or a combination of two or more drugs, depending on the type of cancer and how fast it is growing. Depending on the resectability (likelihood that the tumor can be completely removed by surgery) of the pancreatic cancer, chemotherapy can be given:
- Prior to surgery, to try to reduce the size of the pancreatic tumor that needs to be removed. This is called neoadjuvant therapy.
- After surgery, to destroy any cancer that may not have been completely removed. This can reduce the chance that the cancer returns and is called adjuvant therapy.
- Along with radiation, which is called chemoradiation. This is sometimes used for localized pancreatic cancer.
There are many chemotherapy drugs used to treat pancreatic cancer, including:
- Gemcitabine
- Nab-paclitaxel
- 5-fluorouracil (F-5U)
- Irinotecan
- Oxaliplatin
- Capecitabine
- Cisplatin
- Liposomal Irinotecan
Based on the patient’s ability to tolerate therapy, two or more chemotherapy drugs are typically given in combination to treat patients.
Two chemotherapy combinations have been approved for the initial treatment of pancreatic cancer, including:
- Gemcitabine + nab-paclitaxel
- FOLFIRINOX (5-flurouracil, irinotecan and oxaliplatin)
Radiation for pancreatic cancer
Radiation therapy uses high-energy photon beams (x-rays) to slow or shrink pancreatic tumors. Due to the level of precision of some types of radiation therapy, higher than normal doses of radiation (dose-escalation) can be considered and used without damaging normal tissues. MD Anderson uses several different types of radiation therapy to treat pancreatic cancers.
- Intensity-modulated radiation therapy (IMRT): Delivers radiation beams from several different angles using advanced imaging and computational techniques. Because of the extreme precision associated with this therapy, higher-than-normal doses of radiation (dose-escalation) can be used. This type of therapy is usually administered between 3-6 weeks and is sometimes given in addition to chemotherapy.
- Stereotactic body radiation therapy (SBRT): Also known as stereotactic ablative radiotherapy, or stereotactic ablative body radiation (SABR), SBRT precisely targets tumors with very high doses of radiation. SBRT achieves this by using several radiation beams of various intensities aimed at the tumor from different angles.
- 3D conformal radiation therapy: The traditional method that uses three-dimensional scans to image the tumor prior to delivering radiation beams. This type of therapy is usually administered for about 2-6 weeks.
- Proton therapy: Delivers proton beams, rather than photon beams. In some situations, protons cause less radiation exposure to surrounding tissue than photons. This type of therapy may be used for pancreatic cancer patients whose disease has recurred in the same area, despite prior radiation therapy.
At MD Anderson, our radiation oncologists use a special machine called a CT on rails to deliver higher than normal doses of radiation (dose-escalation) with extreme precision. This technique is typically used during IMRT and SBRT.
Targeted therapy for pancreatic cancer
Instead of killing cancer cells, as well as healthy cells, with traditional chemotherapy, targeted therapy isolates specific molecules and slows or stops their growth.
For some patients with advanced cases of pancreatic cancer, MD Anderson doctors can conduct genetic sequencing to determine whether the patient is a candidate for one of MD Anderson’s targeted therapy clinical trials.
In these clinical trials, researchers are using novel therapies to target specific genetic mutations, such as the KRAS mutation, that until now were considered untreatable.
These experimental therapies have the potential to improve the chances of successful treatment and survival.
Learn more about pancreatic cancer:
Treatment at MD Anderson
Pancreatic cancer treated in our Gastrointestinal Center.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.

Pancreatic cancer survivor: I’m glad I took a chance on a Whipple procedure
You might say that cancer runs in my family, but not with what I’d call any consistency. There’s been a random case of bladder cancer here, colon cancer there, or melanoma somewhere else. But overall, my extended family has been pretty healthy. So, I was surprised to be diagnosed with pancreatic cancer in 2017.
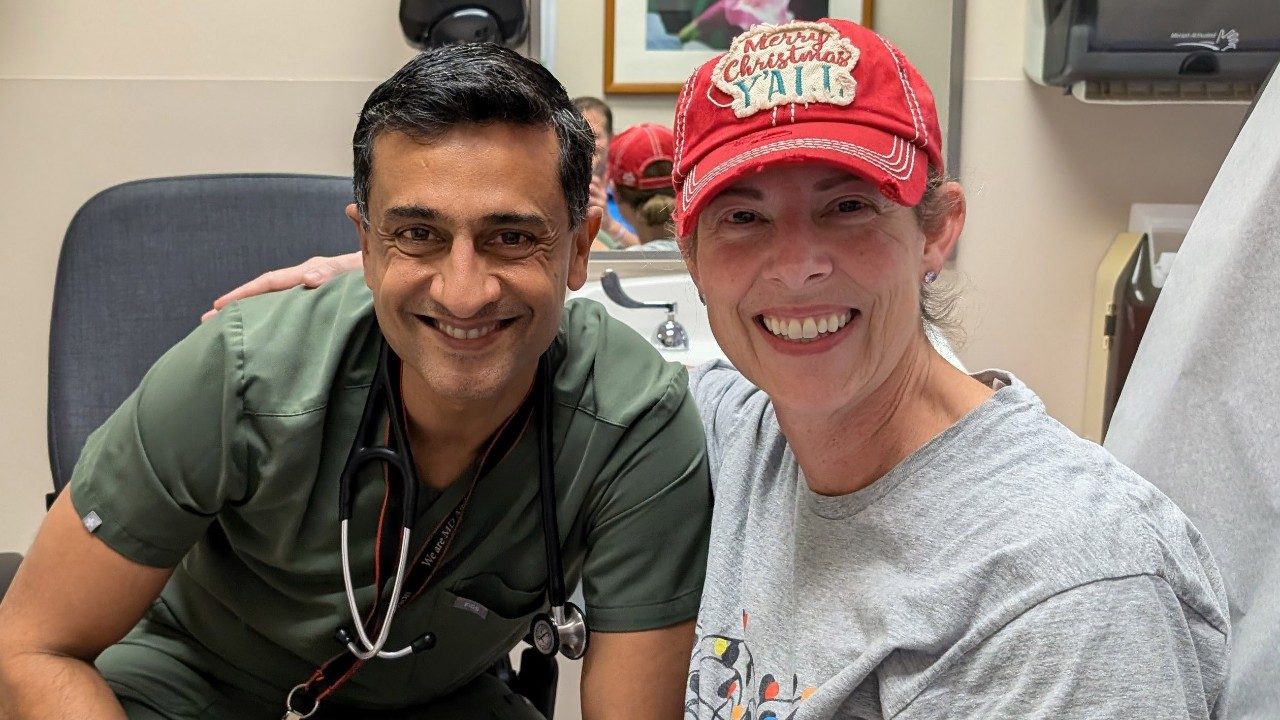
I went to MD Anderson for my treatment at the recommendation of one of my office staff. Her son-in-law did a fellowship there under Dr. Ching-Wei Tzeng, a surgical oncologist who specializes in gastrointestinal tumors.
My pancreatic cancer treatment was really tough. But I’m cancer-free today. I’m feeling good and back to ranching full-time. If I hadn’t gone to MD Anderson, I wouldn’t be here today. So, if I had to do it all over again, I would.
My pancreatic cancer symptoms
I’ve had problems with ulcers and irritable bowel syndrome for most of my adult life. So, I initially chalked up the abdominal pain I felt for a couple of weeks before my diagnosis to one of those. Then, my doctor prescribed an antibiotic, and I had what I thought was an allergic reaction to it. I started itching all over real bad.
My wife was putting calamine lotion on my back to soothe the itching one day when she noticed that my skin was turning yellow. I called the doctor. He told me I must have a blockage somewhere and to be there in an hour. Scans revealed a tumor on my pancreas. It was about the size of a man’s thumbnail and looked like a tiny soda can.
My doctor said that pancreatic tumors were rarely benign, but that I might be a candidate for surgery since the tumor was fairly small and didn’t appear to be attached to any blood vessels. I just needed to go someplace with experts who could treat it properly.
My wife and I called MD Anderson and made an appointment.
My pancreatic cancer treatment
At MD Anderson, I had a stent endoscopically installed to unblock my bile duct. The tumor happened to be sitting on it, which caused my symptoms to show up early. Pancreatic cancer doesn’t usually cause symptoms in its early stages. So, to that extent, I guess, I kind of lucked out.
Once I had the stent installed, I started chemotherapy to shrink the tumor under the supervision of gastrointestinal oncology specialist Dr. Milind Javle, then had a Whipple procedure under Dr. Tzeng to remove it. Afterward, I had more chemotherapy to kill any potential microscopic cancer cells that might still be floating around, undetected by scans.
I trusted Dr. Tzeng, but I was really worried about the Whipple procedure. My late grandfather had had his stomach removed at another hospital years before and barely survived the operation. I’d heard family stories for years about how hard that experience was for him and how much it changed his life for the worse. I knew my only chance at survival was to have the surgery, but it still took everything I had to go through with it.
The hardest parts of my pancreatic cancer treatment
Dr. Tzeng performed my Whipple procedure on Oct. 9, 2017. It took me quite a while to start feeling normal again afterward. Even now, my digestive system can be fickle. But I’m adapting, and I can eat about anything I want to in moderation. Now, instead of having one or two bad days a week, I’ll only have them about once every six months, which is probably no different from a person who hasn’t had intestinal surgery.
Chemotherapy turned out to be the hardest part of my cancer treatment. I was so sick that some days I couldn’t get out of bed until 3 p.m. Even then, I’d just lie there on the couch and breathe. I was too sick to do anything else, even watch TV. I came close to wanting to give up. But then I’d think, “What if the next round is the one that cures me?” So, I’d gather my strength and go back for another.
Hold onto hope
Nobody knows how you’re going to respond to cancer treatment, or what’s going to happen to you in the end. The main thing is not to give up hope. It’s easy to feel low when the whole thing starts. You find out you’re sick, and the news always seems to be bad.
But today, I’m 69 and back to managing our ranch full-time. We have about 400 head of cattle now. We also have two grandkids, both born after my diagnosis. That’s way cool. It took about three years, but now I’m not just alive, but living.
I always wanted a custom-made saddle, but never felt like I could afford it. Then, a few months before my cancer diagnosis, I had a little extra money in my pocket from a business I’d sold. I decided to splurge and ordered one built. Then I found out I had cancer, and I thought, “I’ll never get a chance to use it.”
Today, that saddle has a lot of wear on it. And two years ago, I took out a 20-year mortgage to buy another piece of land. That’s not something I ever thought I’d do again. So, hold on to hope. It’s out there.
Request an appointment at MD Anderson online or call 1-877-632-6789.

‘How I knew I had pancreatic cancer’: 3 survivors share their symptoms
The most common symptoms of pancreatic cancer are pain in your abdomen or back, weight loss and jaundice.
But these issues can also be caused by other conditions, such as gallstones, hepatitis or even heavy drinking. So, when should you see a doctor about them?
“Most people with abdominal pain won’t have pancreatic cancer,” says pancreatic cancer surgeon Matthew Katz, M.D. “But any pain that persists beyond a couple of weeks should still get checked out. And, if you’re experiencing rapid weight loss without trying, you should mention it to your doctor as soon as you notice it. Anyone whose skin or eyes turn yellow should be evaluated immediately.”
Here’s how three of our patients knew they had pancreatic cancer, in their own words.
Abdominal pain that radiates to your back
“I had a little dull pain start just below my left breast in September of 2016,” recalls Reneata Benjamin, a retired elementary school librarian who was 53 when she was diagnosed with stage III pancreatic cancer. “I was rubbing it so much that people started asking me what was wrong. Finally, my daughter told me I needed to see a doctor because it just kept getting worse.”
Sometimes, the combination of back and abdominal pain can make pancreatic cancer patients feel like there’s a belt of pain wrapped around their middle.
“The classic presentation is to have abdominal pain that radiates to the back,” explains Katz.
Jaundice
Jaundice, or yellowing of the skin or eyes, is another telltale sign of pancreatic cancer.
“My wife noticed my skin turning yellow while putting calamine lotion on my back to soothe some itching,” remembers Steven Adami, a Wyoming rancher who was 62 when he was diagnosed with stage II pancreatic cancer. “I called the doctor, and he was so concerned that he told me to be at his office in an hour.”
Itching
Itchy skin was what prompted Dana Sigalos to contact her doctor.
“I went in for my regular checkup feeling fine over the Thanksgiving break in 2022,” recalls the retired oil and gas professional, who was 64 when she was diagnosed with stage I pancreatic cancer.
“But the following Monday, I developed unbearable itching all over my body. I called my doctor and said, ‘You’ve got to do something about this.’ Instead, he told me I needed more testing. My bloodwork had just come back and it was abnormal. My bilirubin levels were really high.”
Unexplained weight loss
Unintentional weight loss is a common symptom of many gastrointestinal cancers, including pancreatic cancer.
This weight loss could be due to:
- inflammatory proteins secreted by the cancer
- jaundice, pain or other symptoms
- physical obstructions in the gastrointestinal tract
All of these can limit a person’s appetite and ability to get enough nourishment.
If you experience rapid, unintentional weight loss, it’s important to tell your doctor. So, what counts as rapid weight loss?
“Losing 5% or more of your body weight in a month would be very concerning,” says Katz. “But losing anything over 10 pounds, even if it’s over an extended period, such as 3 to 6 months, should be investigated if it can’t be explained by a change in diet, activity level or medications.”
Don’t dismiss non-specific symptoms
Other symptoms of pancreatic cancer include:
- Dark urine or light-colored stools
- Bloating, or a feeling of fullness
- Nausea, vomiting or indigestion
- Fatigue
- Lack of appetite
- Sudden-onset diabetes
Unfortunately, pancreatic cancer doesn’t often produce symptoms in its earliest stages. So, by the time they start appearing, the disease is often advanced, when it’s harder to treat. That’s why Katz says you shouldn’t dismiss even vague symptoms.
“I can’t tell you the number of patients I’ve seen who had aches and pains or diarrhea for months and just didn’t think it was worth mentioning to their doctor,” Katz says. “Don’t dismiss these symptoms, particularly if they’re persistent or in the elderly. While they may turn out to be caused by something other than pancreatic cancer, they’re worth evaluating.”
Request an appointment at MD Anderson online or call 1-877-632-6789.

Second opinion, rare interventional radiology procedure save stage IV pancreatic cancer patient
When retired geologist and author David Allard was diagnosed with stage IV pancreatic cancer in August 2020, his local doctor told him he had less than six months to live.
“I was only 62 at the time,” David recalls. “I hadn’t had any symptoms. And I’d always been very fit and active. So, I couldn’t accept that prognosis.”
The Texas Hill Country resident sought a second opinion at MD Anderson. Gastroenterologist William Ross, M.D.; gastrointestinal medical oncologist Shubham Pant, M.D.; and gastrointestinal radiation oncologist Eugene Koay, M.D. devised a treatment protocol. But some unchecked internal bleeding threatened to derail the whole plan.
That’s when they referred David to interventional radiologist Peiman Habibollahi, M.D. And that’s why David is still here, five years later.
Unconventional problem calls for unconventional solution
David’s internal bleeding was due to a condition called portal and splenic vein thrombosis, blood clots in the main vessels that carry blood from the intestines to the liver. In David’s case, they were caused by a lime-sized pancreatic tumor pressing up against both of those veins. That, in turn, was causing varices to develop in his stomach. They were under so much pressure, they’d begun to bleed.
As with all deep-tissue blood clots, David’s thrombosis was potentially fatal on its own. But it also posed a serious roadblock to his healing.
“David’s internal bleeding was unresponsive to any conventional treatments, such as endoscopic cauterization,” explains Habibollahi. “He was also losing so much blood that it was becoming life-threatening. As a result, David was unable to continue receiving cancer therapy.”
Shunt installed during complex surgery still working, five years later
To resolve the problem, Habibollahi proposed a pair of procedures:
- An image-guided recanalization of the portal and splenic veins
- A trans-jugular intrahepatic portosystemic shunt, also known as “TIPS”
The first procedure would create a new pathway for blood to flow through and decompress the varices that were bleeding. The second would protect the new connection with a shunt to ensure it remained open and functional.
“Dr. Habibollahi said he couldn’t guarantee it would work, but there was a pretty good chance that it would,” David recalls. “He had done this surgery about 20 times before, and was successful in 75% of those cases.”
David decided to take a chance. He had the complex, eight-hour surgery on Dec. 7, 2020, and stayed in the hospital for five days to recover.
“I’m really grateful that Dr. Habibollahi didn’t give up,” adds David. “He ran into a few snags during the procedure, but he kept trying, using an incredibly tiny tool set to do all this intravenously. The shunt is still there and working well. My blood counts are nearly normal.”
Successful surgery means cancer treatment can continue
Once it was clear the surgery had been successful, David was able to resume his cancer treatments. In all, he had 17 rounds of intravenous chemotherapy under gastrointestinal medical oncologist Shubham Pant, M.D., followed by three weeks of radiation therapy at the recommendation of radiation oncologist Eugene Koay, M.D.
After his last radiation treatment in July 2021, David started taking an oral chemotherapy agent called capecitabine. He’s been on that drug ever since for maintenance. He shows no evidence of disease.
“Most people die within a year of my diagnosis,” says David. “But scans show there’s nothing but scar tissue left now where the tumor once was. That’s why you can’t just accept the first thing you’re told. Dr. Habibollahi performed a surgery on me that’s not done just anywhere. MD Anderson saved my life.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Innovative robotic Whipple procedure helps cancer survivor beat the odds again
In February 2024, Mandy Gartrell was diagnosed with stage III pancreatic cancer. The teacher, wife and mother of two was already a cancer survivor after a breast cancer diagnosis in 2010. So, Mandy and her husband, Brandon, were surprised by her latest diagnosis.
“Hearing you have cancer, it doesn’t matter how many times, is always shocking. We went through a lot of emotions,” she says.
Mandy’s pancreatic cancer symptoms included a recurring ache in her upper abdomen, yellowing skin, a flat rash and darkening urine. After abnormal bloodwork, she went to the ER for a sonogram, and eventually an MRI and CT scan, which showed a blockage in her primary bile duct. An endoscopic retrograde cholangiopancreatography revealed a 2.5-centimeter mass on her pancreas.
Pancreatic cancer diagnosis leads to treatment at MD Anderson
Mandy had a procedure done back home in Fort Worth, Texas, to place a stent into her bile duct. Afterward, her surgeon referred her to MD Anderson to seek specialized surgical treatment for the pancreatic tumor. Her tumor was intertwined with major vessels and in a difficult location next to her hepatic artery.
MD Anderson surgical oncologist Naruhiko Ikoma, M.D., spoke with Mandy and told her, “We can take care of this.” Ikoma specializes in robotic surgery and the multidisciplinary treatment of pancreatic and gastric cancers. He felt confident that MD Anderson could provide her with the best results.
“When Dr. Ikoma walked us through Mandy’s surgical plan, I realized we were working with a top expert in the field. I knew we were in the right hands,” says Brandon. “He was kind and understanding, and he listened to us.”
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention and Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
