request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Thyroid Cancer
Get details about our clinical trials that are currently enrolling patients.
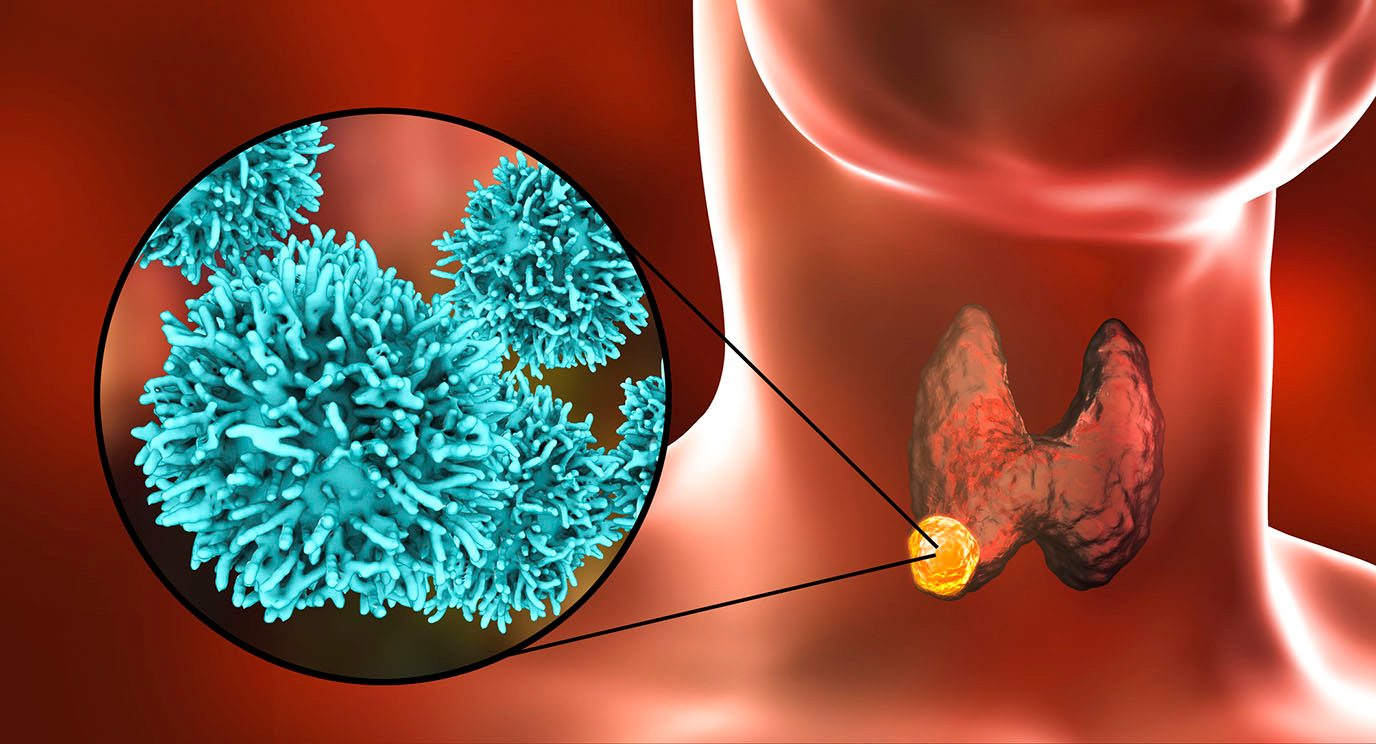
View Clinical TrialsThyroid cancer begins in the thyroid gland, a small butterfly-shaped gland in the front of the neck at the base of the throat. It is usually a slow-growing disease that can be treated successfully.
Thyroid cancer begins in the thyroid gland, a small butterfly-shaped gland in the front of the neck at the base of the throat. It is usually a slow-growing disease that can be treated successfully.
The thyroid has two halves, or lobes, one on each side of the neck. It wraps around the trachea (windpipe) just under the larynx (Adam's apple). A thin strip of tissue known as the isthmus connects the two halves.
The thyroid is part of the body's endocrine system, a system of glands that controls hormones in the body. It normally weighs less than an ounce and cannot be seen or felt in most people. However, it has an important function. The thyroid makes hormones that help regulate the body's heart rate, blood pressure, temperature and metabolism (the breakdown of food to create energy).
Thyroid cancer rarely impacts the thyroid gland’s ability to produce hormones. There is no connection between thyroid cancer and common thyroid conditions like hyperthyroidism.
Differentiated thyroid cancer
Most thyroid cancers can be categorized based on how their cells look compared to normal cells. These are called differentiated thyroid cancers. They can be either well differentiated or poorly differentiated.
Cancer cells that look most like normal, healthy cells are well differentiated. Patients with well-differentiated thyroid cancers are most likely to be disease-free at the end of treatment.
Doctors believe most thyroid cancers start as well-differentiated. As the cancer grows, its cells can develop additional mutations, changing it to a poorly differentiated cancer. Compared to well-differentiated thyroid cancer, these diseases are harder to treat. They also have a have a higher risk of spreading to the lungs and bones and are more likely to recur after treatment.
Differentiated thyroid cancers develop from follicular cells. Follicular cells produce thyroid hormone, which is important for growth, mental function and metabolism.
Differentiated thyroid cancer types include:
Papillary thyroid cancer: This is the most common type of thyroid cancer. It accounts for about 80% of diagnoses. It occurs in only one lobe of the thyroid gland in 80-90% of cases and both lobes in 10%-20%. Treatment is successful in most cases.
Follicular thyroid cancer: This accounts for less than 10% of thyroid cancers. Though it can be more aggressive than papillary thyroid cancer, follicular thyroid cancer usually grows slowly. Treatment for follicular thyroid cancer is similar to papillary thyroid cancer and is successful for most patients.
Both papillary and follicular thyroid cancer are considered well-differentiated cancers. Well-differentiated thyroid cancer tends to stay contained within the thyroid gland. When it does spread outside the thyroid, the most common locations of spread, or metastasis, are lymph nodes, lungs, bones and the liver.
Oncocytic thyroid cancer/Hürthle cell thyroid cancer: Also called oxyphilic cell carcinoma, this disease was considered a type of follicular thyroid cancer until recently. Most patients diagnosed with Hürthle cell carcinoma do well, but the outlook may change based on the extent of disease at the time of diagnosis.
Poorly differentiated thyroid cancer: This is a rare type of thyroid cancer, accounting for less than 5% of all cases.
Anaplastic thyroid cancer
This disease makes up just 1% of thyroid cancer cases. Sometimes called undifferentiated thyroid cancer, it is the rarest and most dangerous type of thyroid cancer. These tumors start as papillary, follicular or Hurtle cell thyroid cancers. They then develop more mutations that cause them to behave very aggressively.
Anaplastic thyroid cancer grows and spreads very rapidly. As it grows, it can move into the trachea and cause breathing problems. Patients with anaplastic thyroid cancer need to seek out treatment immediately.
Some patients are now effectively treated with targeted therapy, surgery, and a combination of chemotherapy and radiation therapy. MD Anderson’s Anaplastic Thyroid Cancer Clinic provides the immediate, specialized treatments these patients require.
Medullary thyroid cancer
Medullary thyroid cancer (MTC) is the only type of thyroid cancer that develops from the parafollicular cells of the thyroid gland.
Parafollicular cells, also known as C cells, produce calcitonin, which helps control calcium metabolism. Most parafollicular cells are in the upper third of each lobe of the thyroid. MTC accounts for less than 5% of thyroid cancers. MTC cells usually produce calcitonin and/or carcinoembryonic antigen (CEA). These proteins can be measured in the blood and used to monitor how the disease is responding to treatment.
Sometimes MTC spreads to the lymph nodes, lungs or liver before a thyroid nodule is found or symptoms develop. MTC can be treated most successfully if it is diagnosed before it has spread.
There are two types of MTC:
- Sporadic MTC accounts for 85% of medullary thyroid cancers. It occurs mostly in older adults and is not inherited.
- Familial MTC is inherited. It often seen in childhood or early adulthood. If familial MTC occurs in association with tumors of certain other endocrine organs (such as the parathyroid and adrenal glands), it is called multiple endocrine neoplasia type 2 (MEN 2). Patients with MTC should undergo genetic testing to learn if they have inherited the gene that causes familial MTC. If they have the gene, their parents, siblings and children should also get genetic testing.
Thyroid cancer statistics
About 44,000 people are diagnosed with thyroid cancer each year in the United States. More than half of the cases occur between ages 20 and 55. The disease is slow growing and responds well to treatment. Its five-year survival rate is more than 98%.
Thyroid cancer risk factors
A risk factor is anything that increases a person’s chance of developing a specific disease.
Less than 1% of thyroid cancers are tied to a risk factor other than age and gender. Certain risk factors have been identified, though. They include:
- Exposure to high levels of radiation, especially during childhood: Radiation exposure is the most significant risk factor for thyroid cancer. This exposure typically comes in the form of radiation treatment to the head and neck area for a childhood cancer. Occasional X-rays or scans that are part of routine medical procedures (such as a dental exam) have very low levels of radiation and are not risk factors.
- Inherited disorders: Familial medullary thyroid cancer is usually caused by an inherited mutation in the RET gene. People who inherit the gene are likely to develop medullary thyroid cancer. Other types of thyroid cancer also may be caused by diseases that run in families. People with a history of thyroid cancer in their family should consider genetic counseling to learn and manage their risk.
- Iodine deficiency: The thyroid uses iodine to make hormones. People with low iodine levels have a higher risk of developing thyroid cancer. This risk factor is uncommon in the United States, where iodine often is added to table salt.
- Age: Over half of thyroid cancer cases occur between ages 20 and 55.
- Gender: Women are three times as likely as men to develop thyroid cancer. Papillary thyroid cancer, the most common type of the disease, is found most often in women of childbearing age.
Not everyone with risk factors gets thyroid cancer. However, if you have risk factors it is a good idea to discuss them with your doctor.
Some cases of thyroid cancer can be passed down from one generation to the next. Genetic counseling may be right for you. Learn more about the risk to you and your family on our genetic testing page.
Learn more about thyroid cancer:
MD Anderson is #1 in Cancer Care

10 thyroid myths you shouldn’t believe
Have you ever heard that people with thyroid disorders shouldn’t eat certain vegetables? Or that you can treat an underactive thyroid gland with iodine supplements, and other thyroid disorders with hormone supplements?
If so, you’re not alone. The only problem? None of these claims is accurate. So, before you take any action based upon them, we want to set the record straight on these and seven other common thyroid myths you might’ve heard.
Myth #1: If you’re feeling tired, gaining weight, losing your hair and unable to concentrate, it must be your thyroid.
Fact: These symptoms can be linked to thyroid problems, but they are more often caused by aging, stress, lack of sleep, and poor nutrition. Many people begin experiencing these issues as they get older.
These symptoms may also be caused by chemotherapy or cancer. In any event, they are not always due to thyroid problems.
Myth #2: People with thyroid disorders should avoid certain vegetables.
Fact: Patients with certain types of thyroid cancer may be asked to follow a low-iodine diet temporarily while undergoing diagnostic testing or as a part of their treatment. But people with thyroid disorders can and should eat a healthy, well-balanced diet.
Some people claim that cruciferous vegetables — including broccoli, cauliflower, Brussels sprouts and kale — can interfere with thyroid function. However, these vegetables are still part of a heathy, balanced diet, and you can eat them in moderation, even if you have a thyroid disorder.
Myth #3: You can address thyroid disorders with over-the-counter hormone supplements.
Fact: Many over-the-counter thyroid supplements are not regulated by the Food and Drug Administration (FDA), and there is no oversight on these products, which are made with hormones taken from animals. There is also very little data on their long-term effects. So, we would not recommend them.
Myth #4: You can fix an underactive thyroid with iodine supplements.
Fact: Diet alone cannot cure thyroid problems. But iodine supplements can negatively affect the thyroid gland if taken without a physician’s supervision.
Still, it is very rare for people to be iodine-deficient in the United States. Iodine is usually present in the soil where farmers grow their fruits and vegetables. Also, many foods produced here are fortified with iodine, including:
- dairy products
- eggs
- bread
- salt
- seafood
Myth #5: If you have hypothyroidism, you need a thyroid ultrasound.
Fact: Having hypothyroidism does not automatically mean you need a thyroid ultrasound. You only need an ultrasound if you have signs of a thyroid nodule or other concerns that require further evaluation.
Most people with hypothyroidism do not need routine ultrasounds.

Do thyroid cancer patients need a low-iodine diet?
You’ve probably heard of the low-fat diet. Maybe even the low-carb diet. But what about the low-iodine diet?
If you or someone you know has been diagnosed with thyroid cancer, this is the diet you’re most likely to hear about. But why might a low-iodine diet be recommended by a doctor, and which cancer patients stand to benefit the most from one?
For answers to these questions and more, we checked in with Jessica Tilton, senior clinical dietitian.
What is the low-iodine diet?
The low-iodine diet is sometimes prescribed to people with differentiated thyroid cancer (papillary, follicular and poorly differentiated). Its goal is to make their thyroid glands “hungry” for iodine by temporarily eliminating as much of that mineral as possible from their diets.
Doctors can then “light up” the cancerous areas during a scan, or treat those same areas using radioactive iodine, because papillary thyroid cancer cells will quickly absorb it.
Can the low-iodine diet be used by patients with other types of thyroid cancer?
Only differentiated thyroid cancer cells absorb radioactive iodine. So, it’s not effective with anaplastic or medullary thyroid cancers.
How long are differentiated thyroid cancer patients typically asked to follow a low-iodine diet?
It’s not meant to be a long-term thing. Generally, we recommend it for up to 14 days before a diagnostic procedure or treatment, and then maybe 1 to 3 days afterwards.
What does a low-iodine diet entail? Are there particular foods to avoid?
The American Thyroid Association recommends that people following a low-iodine diet limit their iodine intake to 50 micrograms or less per day. That means avoiding iodized salt and anything that comes from the ocean. This includes fish, shellfish, seaweed, and even calcium supplements derived from oyster shells. Other things to avoid include:
- egg yolks
- dairy products
- red dye #3 (found in maraschino cherries and some fruit cocktails)
- blackstrap molasses
- soy products (including tofu)
- rhubarb
- bakery products (made with iodized salt in the dough, or other ingredients containing iodine, such as potassium iodate)
Which foods are allowed on the low-iodine diet?
There are many foods people can still enjoy on a low-iodine diet. These include unsalted:
- vegetables and fruits (fresh or frozen)
- nut butters
- egg whites
- fresh meats (less than 6 ounces per day)
- peeled sweet or regular potatoes
- pastas
- vegetable oils
- whole grains, such as rice or oatmeal
- salads with vinaigrette or other salt-free dressings
As with any diet in which you’re actively trying to avoid a particular ingredient, it’s important to check food labels for iodine.
What could happen if I don’t adhere closely enough to a low-iodine diet?
If your thyroid isn’t sufficiently deprived of iodine before a procedure involving radioactive iodine, it could adversely affect the accuracy of your test results or the effectiveness of your treatment. So, you might have to do the whole thing all over again, which could delay your treatment.
Can people who are allergic to seafood benefit from the low-iodine diet?
No. Most people who are allergic to the iodine in seafood tend to be allergic to a specific type, such as crab or shellfish. It’s actually pretty rare to find someone who has issues with iodized salt by itself.
And again, the human body needs iodine to function correctly. So, a low-iodine diet is designed to be temporary. It’s not meant to be a permanent solution.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Papillary thyroid cancer: 8 questions, answered
Papillary thyroid cancer is the most common form of thyroid cancer. It is normally a slow-growing cancer and makes up roughly 80% to 85% of all thyroid cancer cases.
How is papillary thyroid cancer diagnosed? Does it have any symptoms? And how is it typically treated?
For answers to these questions and more, we reached out to endocrinologist Priyanka Iyer, M.B.B.S., who specializes in endocrine neoplasia and hormonal disorders.
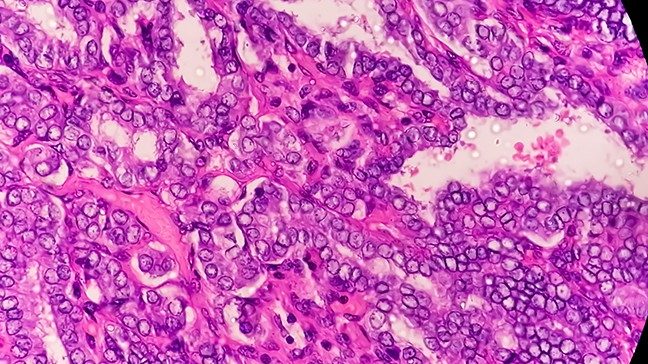
How is a “papillary” thyroid cancer diagnosis made?
We classify thyroid cancer as “papillary” based on the way the tumor cells look under a microscope, rather than the way they appear on scans or to the naked eye during surgery. Papillary thyroid cancer cells have tiny papillae, which are finger-like projections.
What is papillary microcarcinoma?
This term just means that papillary thyroid cancer measures less than one centimeter across, or about the width of a staple. Tumors smaller than that are measured in millimeters. They are usually considered very low risk.
It’s important to note that all thyroid cancers start as microcarcinomas. Then, they grow to whatever size they are at the time of diagnosis.
What is metastatic papillary thyroid cancer?
Metastatic just means cancer has spread from its original location. About 30% of people have metastatic thyroid cancer at the time of their diagnosis.
What are the symptoms of papillary thyroid cancer?
Most people have no symptoms of papillary thyroid cancer, especially when the disease is in its earliest stages. There’s no routine blood test to check for it, either, so most people only find out they have it by chance.
In some cases, a doctor may detect a lump or a nodule on the thyroid by feeling around a patient’s neck during an annual exam. Other times, papillary thyroid cancer may be found when someone gets a CT scan or an MRI done for a different reason.
In its later stages, patients might notice a change in their voice or even weight loss, because they’re having trouble swallowing. In very advanced cases, someone might have trouble breathing because the tumor has already spread to the lungs or wrapped around their windpipe. But those scenarios are very, very rare.
How is papillary thyroid cancer typically treated?
About 80% to 85% of papillary thyroid cancers can be removed surgically. But if a tumor is small enough and of a slow-growing variety that makes it low-risk, we might just recommend observation.
The types of surgery used typically include either:
- a lobectomy/partial thyroidectomy removes only the lobe affected by the tumor
- a total thyroidectomy removes both lobes — the entire thyroid gland
Patients may also be prescribed radioactive iodine treatment if cancer has spread to adjacent tissues or lymph nodes.
What are the latest advances in the diagnosis or treatment of papillary thyroid cancer?
In just the last 10 years, nine different targeted therapy agents have been approved by the Food and Drug Administration (FDA) to treat thyroid cancer. Seven of these can be used for papillary thyroid cancer.
Three of them are considered anti-angiogenics, which target the tumor’s blood supply. Those are:
- Sorafenib
- Lenvatininib
- Cabozantinib
Others target specific genetic mutations, such as:
- Selpercatinib, (RET mutation and fusion gene)
- Pralsetinib (RET mutations)
- Larotrectinib (NTRK-fusion)
- Entrectinib (NTRK-fusion)
How do these new drugs benefit papillary thyroid cancer patients?
Systemic treatments like these are a good option when papillary thyroid cancer is at an advanced stage or is still spreading, despite surgery and radioactive iodine treatment. They work by slowing down a tumor’s growth. So, patients may be able to enjoy a longer life without further disease progression.
These drugs can be used for patients with tumors that can’t be removed surgically, whether due to their size or the fact that they’re wrapped around critical structures. They’re also being used to reduce the overall size of a tumor or the amount of metastatic thyroid cancer in someone’s body.
Newer drugs in this group tend to be very well-tolerated, but some of the older ones can have fairly significant side effects that affect patients’ quality of life. So, it’s important to discuss the risks and benefits of these — or any drugs — with your care team before deciding whether to take them.
What type of research is being done right now for papillary thyroid cancer?
As of now, no immunotherapy agent has been approved by the FDA for the treatment of any kind of thyroid cancer. So, it’s still considered experimental. But at MD Anderson, Mark Zafereo, M.D., is leading a clinical trial combining immunotherapy with two different targeted therapies to see if this combination can shrink down large, inoperable thyroid tumors small enough to make surgery an option.
Two of the drugs involved — dabrafenib and trametinib — have already been approved by the FDA to treat anaplastic thyroid cancer. But we also use them in clinical trials in cases of advanced papillary thyroid cancer, because sometimes, it can turn into anaplastic thyroid cancer.
What’s the one thing you want people to know about papillary thyroid cancer?
Papillary thyroid cancer is usually very slow-growing. But it’s still a good idea to ask for molecular testing before starting your treatment because some mutations can make thyroid cancers less responsive to radioactive iodine. If that turns out to be the case for you, then we can consider other therapies.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Can you have thyroid cancer without knowing?
The thyroid is a small, butterfly-shaped gland at the base of the neck. It’s responsible for the hormones that control your heart rate, blood pressure, temperature and metabolism.
When thyroid cells grow abnormally, they can cause thyroid cancer. But because symptoms are vague and may mimic other less-serious conditions, it’s possible you could have thyroid cancer for months or even years without knowing it.
Thyroid cancer surgeon Nancy Perrier, M.D., explains how thyroid cancer can go unnoticed – and what you can do to catch it early when it’s easiest to treat.
Thyroid cancer symptoms can go unnoticed
Unfortunately, thyroid cancer doesn’t have many obvious symptoms, and they can vary from person to person. Some signs of thyroid cancer include:
- a lump in the front of the neck
- swollen thyroid or swelling in the neck
- pain in the front of the neck that may stretch to the ears
- hoarse voice
- trouble breathing
- persistent cough
- problems swallowing
If you experience any of these symptoms for three weeks or longer, see your health care provider to have them checked out.
Accurate diagnosis is key
Because thyroid cancer symptoms may also be associated with other conditions, like enlarged lymph nodes in the neck, thyroiditis or Hashimoto’s disease, an accurate diagnosis is important. There are several tests your health care provider may use to find out if you have thyroid cancer.
The first thing they’ll likely do is perform a physical exam, to feel for any lumps or swelling in the neck. Firm nodules that don’t go away may be cause for concern. Soft, short-lasting nodules don’t usually cause problems.
After a physical exam, your care team will likely perform:
Imaging exams: Ultrasound and later a CT scan may be used to get a better look at the size, shape and location of thyroid nodules. These exams can also show if thyroid cancer has spread to lymph nodes or other areas of the body.
Biopsy: If the initial imaging shows a potential tumor, a biopsy may be used to remove a small number of cells so a pathologist can look at them under a microscope.
If the biopsy and imaging exams suggest you have thyroid cancer, it’s important to seek care from a cancer center with thyroid cancer specialists to get an accurate diagnosis. For example, you may have several nodules, but if the wrong one is biopsied and deemed benign, a cancerous nodule may get overlooked and cause problems in the future.
At MD Anderson, we have a team of pathologists who exclusively look at thyroid cancer all day, every day.
Certain types of thyroid cancer can grow slowly
Papillary thyroid cancer is the most common and least aggressive type of thyroid cancer. It can occur in one or both thyroid lobes and can grow over several years. Certain people may be at risk for papillary thyroid cancer, like those with some types of young-onset colon cancer.
Patients diagnosed with papillary thyroid cancer often have symptoms that they dismiss for years until receiving a diagnosis.
Other, less common types of thyroid cancer, like anaplastic thyroid cancer or poorly differentiated thyroid cancer, are more aggressive. They tend to present as a large lump that shows up suddenly over a few weeks or months.
Thyroid cancer doesn’t always need treatment right away
If a thyroid nodule isn’t causing problems, patients may choose to take a watch-and-wait approach, where their care team will monitor the lump for any changes before moving forward with treatment.
Most of the time, when patients go to get a lump checked out, it’s already causing trouble breathing or swallowing. In this case, the most common treatment is surgery to remove part or all of the thyroid.
Patients with genetic mutations – especially children at high risk for thyroid cancer – may live for years before needing treatment. We monitor these patients with ultrasounds and lab work.
It’s sometimes better to let the body release thyroid hormones naturally for as long as possible before moving forward with treatment. But, if we know someone is at high risk for developing thyroid cancer, we can watch them closely and, if needed, remove the thyroid quickly, before the disease has a chance to spread.
Seek treatment from thyroid cancer experts
Don’t be afraid to get a second opinion. You want the right treatment at the right time from the right place. The thyroid is such a delicate gland, and it’s in a very challenging area. So, it’s vital to seek treatment from experts who have experience treating – and removing – the tumor so you can achieve the best quality of life possible.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Thyroid cancer survivor: Targeted therapy saved my life
I probably wouldn’t be here today if I’d accepted the standard treatment for my stage IV anaplastic thyroid cancer and stayed in San Diego for my cancer care.
But I took my doctor’s advice and went to MD Anderson instead. My oncologist, Dr. Ramona Dadu, my surgeon, Dr. Mark Zafereo, and the Endocrine Center saved my life. They stepped out of the box to do something different for my thyroid cancer treatment — and it worked. I’ve been cancer-free since December 2017.
My anaplastic thyroid cancer symptoms
I showed no symptoms of thyroid cancer until June 2017, when I suddenly started having trouble swallowing. I went to my chiropractor, thinking I just needed an adjustment. But he felt all around my neck and told me to see a head and neck specialist. Something was growing there.
The specialist performed a biopsy. It showed I had cancer, but he wasn’t sure what kind. A PET scan revealed spots of cancer throughout my neck, so it could have come from my esophagus, thyroid or salivary glands.
The specialist removed more than a dozen lymph nodes from my neck on Aug. 17. They were all cancerous. But he wasn’t able to remove the largest growth because it was sitting right on top of my esophagus. He said his facility didn’t have the team for that and suggested I travel to MD Anderson.
Genetic mutation leads to targeted therapy
I took his advice and made an appointment at MD Anderson.
After MD Anderson head and neck surgeon Dr. Randal Weber had done his own exam and reviewed all my scans and records, he told us he thought I had anaplastic thyroid cancer. But he referred me to the Endocrine Center for confirmation and to see if my tumor could be shrunk. Due to its size and location, my tumor was inoperable at that point.
At the Endocrine Center, I met with Dr. Ramona Dadu. She confirmed Dr. Weber’s diagnosis and said she suspected my cancer also had a BRAF mutation, which meant it would respond well to two targeted therapy drugs: dabrafenib and trametinib. Dr. Dadu performed a blood test to confirm it, but went ahead and started me on the drugs, because the cancer was so fast-growing and the drugs are so fast-acting. We’d know in a matter of days if my cancer was responding, possibly even before the test results came back.
My Christmas miracle
When I first started taking the targeted therapy, my only goal was to live long enough to watch my younger son graduate from college in mid-December. I couldn’t participate in the clinical trial related to the drugs because I could barely swallow water at that point, so pills were out of the question.
But within four days of my first dose (which I received through a feeding tube), I could already feel the tumor starting to shrink. By the time I returned to MD Anderson for my follow-up in October, all that was left of the cancer was dead tissue.
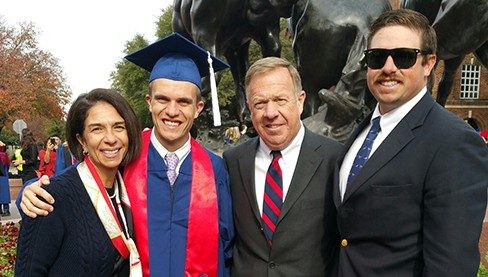
That was great news, of course, but I still needed a surgeon who was willing to remove it from my neck — a complex procedure. The care team presented my case to the tumor board, and luckily for me, Dr. Mark Zafereo stepped up. On Dec. 6, 2017, he removed my thyroid and cleaned out all the dead tissue. About a week later, I was well enough to drive up to Dallas with my wife to watch our son cross the stage and collect his diploma. We’ve called it my Christmas miracle ever since.
Benefitting from the clinical trial I didn’t join
I don’t know if I’ve been cured of anaplastic thyroid cancer yet, and I might never know, because this is such a new protocol for that disease. But if I hadn’t gone to MD Anderson, I probably wouldn’t be here at all. So, I benefitted from that clinical trial, even if I couldn’t participate. And I will gladly stay on these drugs for the rest of my life — or until they stop working, whichever comes first.
I’m thrilled that this combination was approved by the U.S. Food and Drug Administration for use in treating anaplastic thyroid cancer last May. It was already approved as a treatment for metastatic melanoma, but was being studied for use in treating anaplastic thyroid cancer, too.
Now, every time I see that new use listed on the information sheet that comes with my prescription, I feel proud. Because even though I couldn’t join the clinical study myself, my data helped prove that protocol’s effectiveness — so, I played a part in Making Cancer History®.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Pictures of thyroid cancer lumps

Thyroid cancer often has no symptoms when it is diagnosed. It may present as mild neck swelling (as seen on the patient’s left) or a palpable nodule.

The same mass shown from the side.

A larger thyroid mass. The bruise is caused by a needle biopsy of the tumor.

Lymph nodes around the thyroid or on the side of the neck (such as the distinct mass in the middle of the neck) can be affected by thyroid cancer.
Why choose MD Anderson for thyroid cancer treatment?
Where you go first for cancer care matters. For thyroid cancer, getting the best treatment the first time is important, since the disease is much more difficult to treat if it returns.
MD Anderson’s Endocrine Center sees more thyroid cancer patients than almost every hospital in the country. This gives its doctors and surgeons incredible expertise when developing your treatment plan. You will receive customized care for thyroid cancer from a team of renowned experts who work together to coordinate your care.
Your personal medical team will be made up of experts from several specialties. They work together, communicating and collaborating with each other and with you, to ensure you receive seamless, coordinated care.
If your treatment for thyroid cancer includes surgery, our surgeons use the most advanced techniques that are proven to have good results. These surgeons are skilled in performing complex surgeries, including procedures for residual cancers, recurrent cancers and cancers that impact critical structures in the head and neck area.
The Endocrine Center also specializes in treating patients with rare and aggressive thyroid cancers. The first drug to get FDA approval for anaplastic thyroid cancer treatment was developed through MD Anderson research. Today, we offer these patients rapid, specialized care in our Anaplastic Thyroid Cancer Clinic.
We remain at the forefront of research on preventing and treating thyroid cancer. We are constantly researching new therapies, new drugs and new drug combinations designed to cure thyroid cancer, extend life and improve patients’ quality of life.
Through this work, we are able to offer clinical trials for innovative treatments. These include studying the use of therapies to shrink tumors before surgery and the expanded use of targeted therapy for some patients.
And at MD Anderson you will also be surrounded by the strength of one of the world’s largest and most experienced cancer centers. From support groups to counseling to integrative medicine care, we have all the services needed to treat not just the disease, but the whole person.
Every day is a new day to live. I choose to live an incredible life no matter my diagnosis.
Amanda White
Survivor

Thyroid cancer surgery: What to consider
Hearing you have a thyroid nodule can be scary, but it doesn’t always mean you have cancer. In fact, only about 10% of thyroid nodules are malignant.
But if you’ve been diagnosed with thyroid cancer, you may be feeling anxious about the next steps, which almost always include surgery.
Below, Mark Zafereo, M.D., shares what to consider before undergoing thyroid cancer surgery.
Get an accurate diagnosis
It’s important that you’re comfortable with the evaluation of your thyroid nodule before undergoing surgery. Since most nodules aren’t cancerous, many patients don’t need surgery at all.
There are four types of thyroid cancer. About 95% of thyroid cancers are either papillary thyroid cancer or follicular thyroid cancer. Patients with these cancers typically have a good prognosis.
The remaining 5% are medullary thyroid cancer and anaplastic thyroid cancer, which can be more aggressive and may require more extensive treatment.
There are different types of thyroid cancer surgery
The type of surgery your doctor recommends will be based on a risk assessment that includes the tumor pathology, size and location.
The simplest thyroid tumor surgery is a lobectomy. This procedure removes half the thyroid gland. When a thyroid tumor is more likely to spread, a total thyroidectomy (removal of the entire thyroid gland) may be performed.
If the cancer has spread beyond the thyroid gland to surrounding lymph nodes, a more extensive surgery removing these lymph nodes may be needed.
In rare cases, thyroid cancers may spread to other important structures of the neck, which may require more complex surgeries that are best performed by an expert thyroid and neck surgeon.
Ask the right questions
When you meet with your surgeon, make sure you have a clear understanding of your diagnosis, surgical plan and expected recovery. Here are some questions to ask:
- How many thyroid cancer surgeries do you perform each year? The most experienced thyroid cancer surgeons perform more than 100 thyroid/neck surgeries annually.
- What type of thyroid cancer surgery do I need? How much experience do you have performing this specific type of surgery? If the surgeon hasn’t performed many surgeries like yours, seek a second opinion from someone who has.
- How many of your newly diagnosed patients have to undergo a second thyroid/neck surgery within a year? This number should be less than 1%.
- How closely do you work with an endocrinologist, radiologist and pathologist? It’s important that your doctors collaborate and are all confident in the diagnosis and care plan. This minimizes surprises during and after surgery.
- Will the surgery affect my metabolism regulation? If part of your thyroid gland is removed, it may still produce enough of the hormone that regulates your metabolism. But if you have the whole gland removed, you’ll need to take a daily thyroid hormone pill for the rest of your life.
- What are the risks of this thyroid surgery?
- How much discomfort will I have after surgery?
Every patient’s recovery from thyroid cancer surgery is different
Every patient’s recovery is different. Most people take a week or two off work to recover, but can talk and eat a few hours after surgery. All patients will have a scar after surgery. With surgeries limited to the thyroid, the scar is usually about 2 inches long and will look like a natural crease in the neck over time. But ask your doctor what to expect after your particular surgery.
Don’t rush into surgery
With thyroid cancer, you’re not in a race to remove the tumor as soon as possible. Except for the most aggressive thyroid cancers (such as anaplastic thyroid cancer), these cancers are typically slow-growing. Even when the cancer has spread to the lymph nodes, there’s generally not an urgent need for surgery. So, take time to research your options, and find the right cancer center with the right surgeon to perform the right surgery the first time.
Since there’s more urgency with anaplastic thyroid cancer, we encourage these patients to seek proper care soon after diagnosis. At MD Anderson, our specialized clinic called Facilitating Anaplastic Specialized Treatments, or FAST, enables us to quickly finalize treatment plans for patients with suspected anaplastic thyroid cancer.
Specialized care has benefits
Receiving thyroid cancer care at a major cancer center like MD Anderson can make a significant difference in your outcome. At MD Anderson, we have care teams studying every aspect of thyroid cancer, which gives you access to the most cutting-edge care and clinical trials. In fact, MD Anderson has the most clinical trials in the world for medullary and anaplastic thyroid cancers. No matter what type of thyroid cancer you have, a specialized team can help ensure you have a well-thought-out care plan that reduces your chances of recurrence and the need for another surgery.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Thyroid Cancer Treatment at MD Anderson
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients, family members and loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.