Diagnostic Tests
There are many different ways to diagnose cancer. As researchers learn more about the disease, new diagnostic tools are developed and existing methods improved. If your primary care physician suspects cancer, he or she will order tests to make a diagnosis. These tests can either be conducted by your physician or by oncologists at a cancer center like MD Anderson.
No matter who makes the diagnosis, a second opinion by a cancer expert is strongly recommended. Some types of cancer, such as lymphomas, can be hard to classify, even for an expert. Knowing a patient's exact type of cancer allows oncologists to choose the most effective treatment. The most common diagnostic methods include:
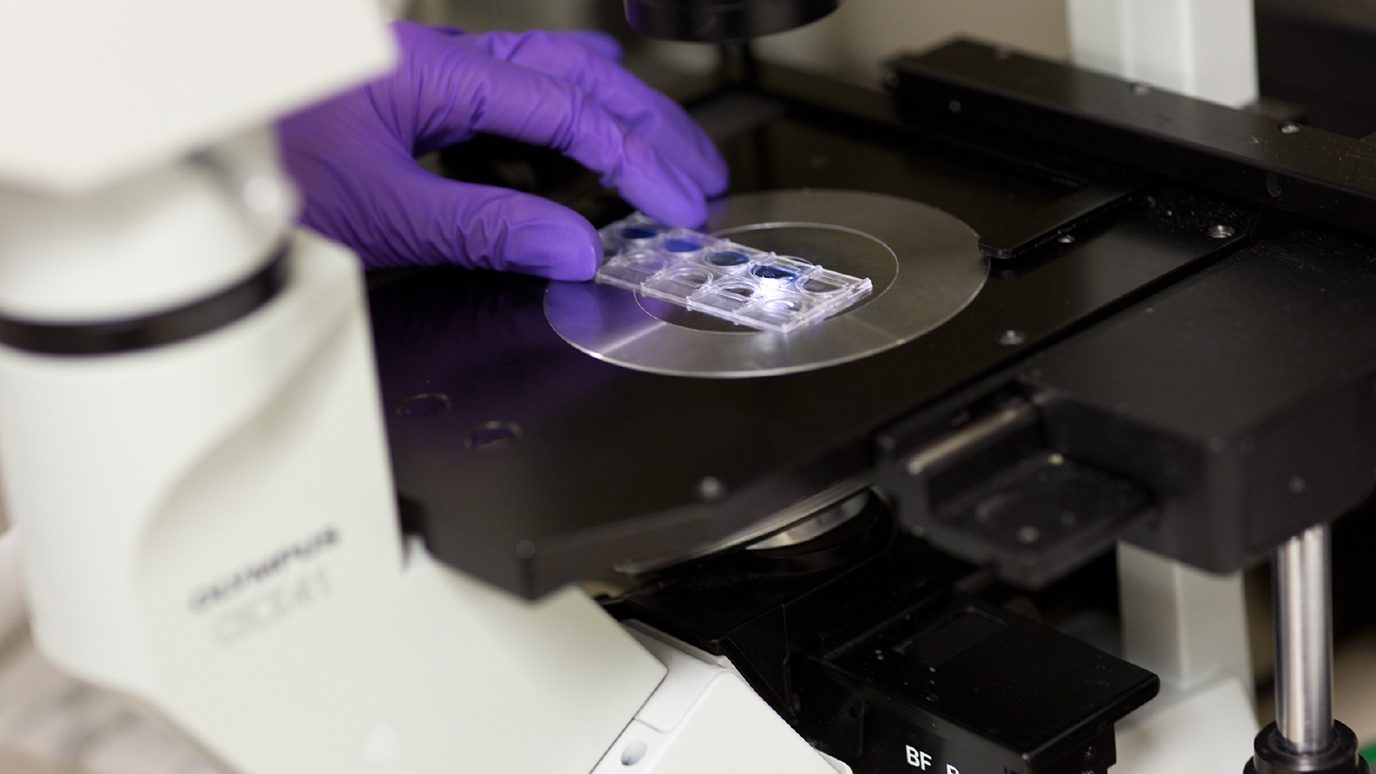
Biopsy
A small tissue sample is surgically removed and examined under a microscope for the presence of cancer cells. Depending on tumor location, some biopsies can be done on an outpatient basis with only local anesthesia. If the tumor is filled with fluid, a type of biopsy known as a fine needle aspiration is used. A long, thin needle is inserted directly into the suspicious area to draw out fluid samples for examination.
Endoscopy
A flexible plastic tube with a tiny camera on the end is inserted into body cavities and organs, allowing the physician to view the suspicious area. There are many types of scopes, each designed to view particular areas of the body. For instance, a colonoscope is used to detect growths inside the colon, and a laparoscope is used to examine the abdominal cavity.
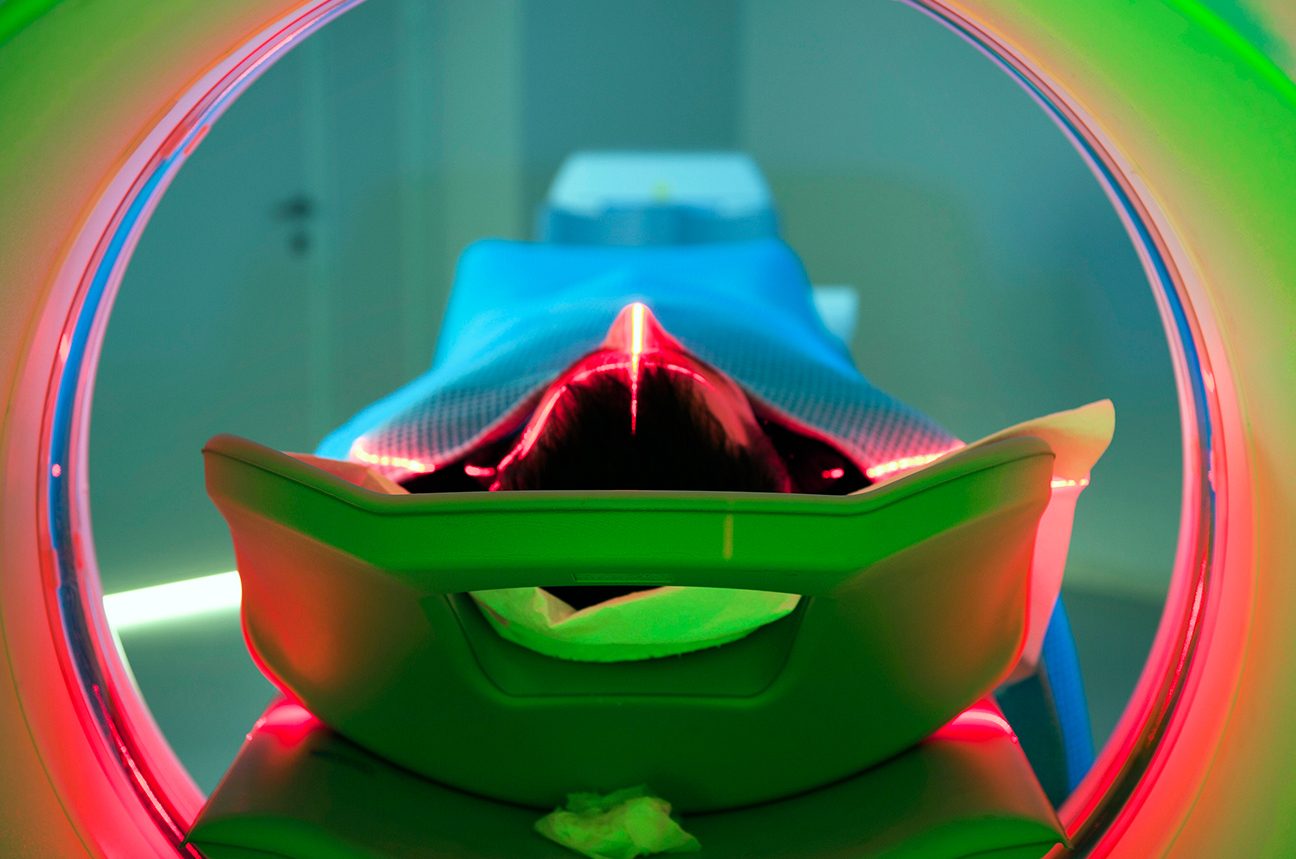
Diagnostic Imaging
MD Anderson uses several diagnostic imaging techniques to produce internal pictures of the body and its structures. These images are usually taken by a trained technician and then analyzed by a radiologist, a physician who specializes in interpreting diagnostic images. The images and the radiologist’s findings are then sent to the patient’s primary care center, where doctors use the information to form a care plan.
Blood Tests
Some tumors release substances called tumor markers, which can be detected in the blood. A blood test for prostate cancer, for example, determines the amount of prostate specific antigen (PSA). High PSA levels can indicate cancer. However, blood tests by themselves can be inconclusive, and other methods should be used to confirm the diagnosis.
MD Anderson Resources
Learn more about different diagnostic tests and procedures.
Which blood tests show cancer?
PSA tests can detect elevated levels of prostate-specific antigen in the blood, which are sometimes a sign of prostate cancer. And complete blood counts — or CBCs — can show high or low levels of certain blood components, which are sometimes a symptom of certain blood cancers.
But are there any simple blood tests available that can prove you have cancer?
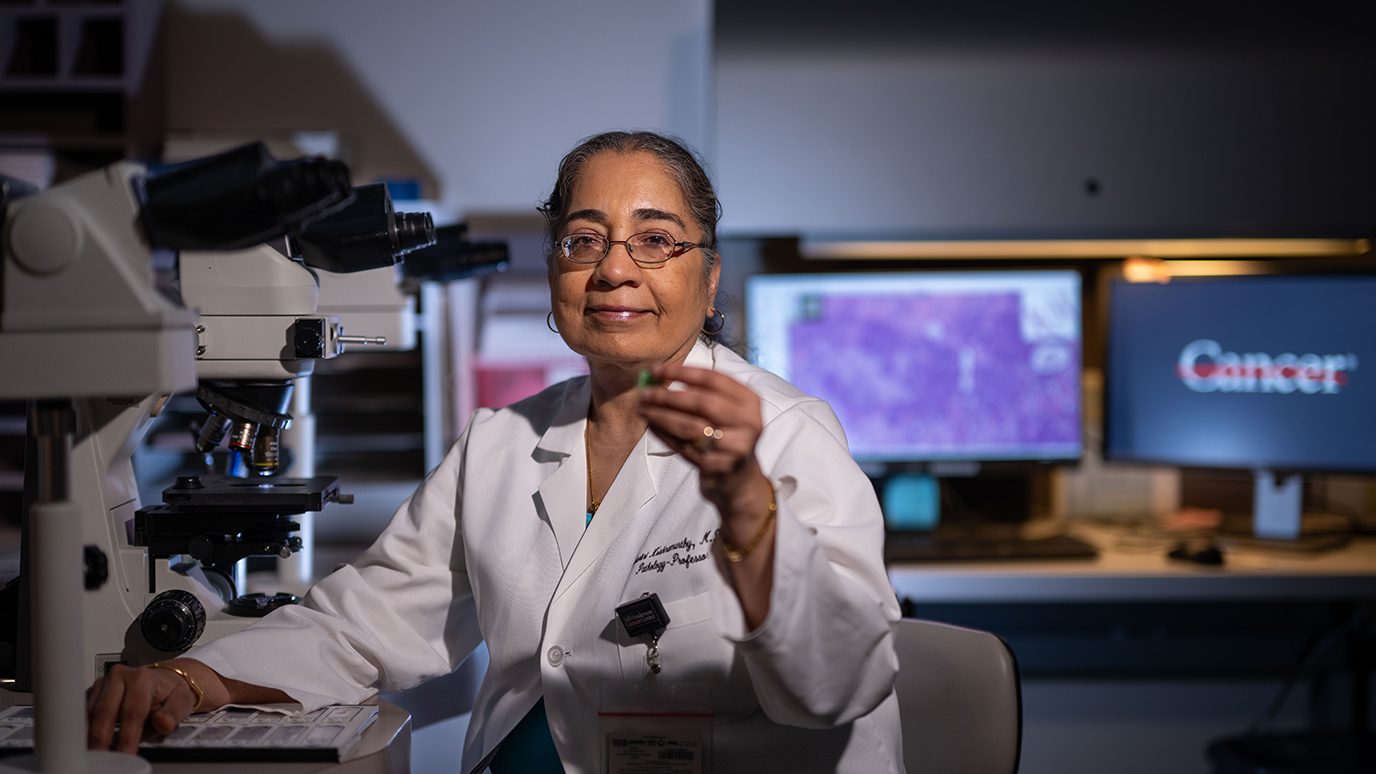
Adriana Maria Knopfelmacher Couchonal, M.D., a specialist in Laboratory Medicine, says the answer is no. “There is no one blood test that can say with certainty, ‘You have cancer,’” she says. “You can only confirm it by examining cells or tissue under a microscope.”
Read on to find out why.
Not all blood abnormalities are due to cancer
Just because you have an abnormal blood test doesn’t mean it’s caused by cancer.
“One good example of this is high protein levels,” explains Knopfelmacher Couchonal. “You might have these due to undiagnosed multiple myeloma. But you could also have them because you’re dehydrated or have an inflammatory condition.”
Screening blood tests are ultrasensitive, but not all-knowing
Screening blood tests are designed to be extremely sensitive. That means they can detect even the slightest abnormalities. But they can’t necessarily tell you what’s causing those abnormalities.
“Some solid tumors secrete chemicals that prompt the body to produce more red blood cells,” Knopfelmahcer Couchonal says. “So, when doctors see that on a blood test, they first try to rule out the most common causes. An elevated red blood cell count could be due to kidney cancer or a myeloproliferative disorder such as polycythemia vera. It could also be due to simple dehydration, hormones or smoking.”
The same principle applies when testing reveals extremely low levels of a particular blood component.
“If a blood test shows you’re anemic, your doctor will try to rule out things like iron deficiency first, before considering more serious possibilities,” she adds. “The vast majority of blood abnormalities can be explained by non-cancerous causes.”
Blood tests are not used in isolation
Even blood tests used to detect certain tumor markers are no guarantee that cancer is present.
Ovarian cancer, for instance, often causes a rise in CA-125 levels, a protein found on the surface of certain cells. But elevated CA-125 levels can also be the result of endometriosis — a painful, yet ultimately benign condition. That’s why doctors have to take other factors into account.
“Blood tests are not used in isolation,” explains Knopfelmacher Couchonal. “Otherwise, medicine would be easy. In addition to elevated CA-125 levels, for instance, we have to look for other things that point to ovarian cancer — like extreme bloating or ascites, as well as an abdominal scan that shows something abnormal.”
Blood tests are only one piece of the diagnostic puzzle
Even when many signs seem to point in a certain direction, you cannot make a definitive cancer diagnosis without a biopsy.
“A biopsy will always be the gold standard,” Knopfelmacher Couchonal says. “You can put all the other diagnostic puzzle pieces together to get a general idea of what you might be looking at. But before you can say for sure what it is, you have to examine tissue under a microscope.”
This applies to liquid biopsies as well, though Knopfelmacher Couchonal says they are not generally used for diagnostic purposes.
“Liquid biopsies can detect certain tumor cells — mostly colon cancer, prostate cancer and metastatic breast cancer,” she says. “But by the time they’re ordered, your diagnosis is usually already known. So doctors use them primarily to monitor your progress and guide any changes in your treatment.”
Request an appointment at MD Anderson online or call 1-877-632-6789.
request an appointment online.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.