request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Glioblastoma
- Glioblastoma Treatment
Glioblastoma Treatment
At MD Anderson’s Brain and Spine Center, some of the nation’s leading glioblastoma experts will develop your treatment plan based on your specific needs. They take a team approach, with neurosurgeons, neuro-oncologists and radiation oncologists working together to coordinate your care and deliver the best therapies with the fewest side effects. Your quality of life is also a key concern during treatment, and our care team constantly looks for ways to make patients as comfortable and self-sufficient as possible.
Glioblastoma treatment plans
The standard treatment for glioblastoma starts with surgery to remove as much of the tumor as safely as possible.
Surgery typically does not remove all of the tumor, though. This is because glioblastoma usually forms microscopic branches that spread into different parts of the brain.
After surgery, patients usually get a combination of chemotherapy and radiation therapy, followed by chemotherapy and possibly tumor treating fields. Elderly patients and/or those who have little to no ability to care for themselves (such as bathing, dressing or feeding themselves) may not be able to withstand the combined chemotherapy and radiation therapy phase of treatment. In these cases, they may get a shorter course of radiation with or without chemotherapy.
Recurrent glioblastoma treatment
Because it is impossible to remove or destroy all glioblastoma cells in a tumor, all glioblastomas recur. The timing can range from weeks to years.
Some patients with recurrent glioblastoma may be eligible for another surgery to remove as much of the tumor as possible. Radiation therapy can also be used as a palliative measure to slow tumor progression and to relieve symptoms caused by the tumor.
However, many standard treatments haven’t proven effective for recurrent glioblastoma. Patients should work with their care team to consider available treatment options and choose a plan that meets their goals. Many clinical trials are available for recurrent glioblastoma, and MD Anderson has one of the largest glioblastoma clinical trial programs in the country, including trials that offer personalized care built around the characteristics of the patient’s specific disease.
Surgery
Surgery is the first treatment for many brain tumors, including glioblastoma.
Glioblastoma tumors develop microscopic branches that spread throughout the brain. In most cases, these branches make it impossible to remove the entire tumor through surgery.
Instead, surgery is used to reduce the size of the tumor, relieve symptoms or help determine what other treatments are needed.
Craniotomy
Craniotomy is the most common surgery for glioblastoma. The procedure involves opening the skull in order to reach the tumor. Some brain tumors can be removed with little or no damage to the brain.
Craniotomies can take anywhere from 4 hours to 12 hours, depending on the size and location of the tumor. Most require a three-to-four-night hospital stay.
There are different types of craniotomies surgeons can use to help them remove as much of the tumor as possible without harming healthy brain tissue.
Awake craniotomy
Most craniotomies are performed under general anesthesia, but some patients undergo awake craniotomies. During these procedures, patients are woken up during the surgery to interact with the surgical team. This helps doctors avoid damaging key structures in the brain. Learn more about awake craniotomies.
Craniotomy with intraoperative MRI
If a patient has a large or complex tumor, doctors may use an intraoperative MRI during the procedure. This gives the surgeon a real-time image of the entire tumor throughout the operation. Surgeons use these images to help them remove as much of the tumor as possible while protecting normal, healthy brain tissue.
Fluorescence-guided craniotomy
Some brain tumors look like healthy brain tissue. These tumors can be difficult to distinguish from health brain tissue.
In these situations, doctors use a special solution, called a contrasting agent, to help them identify cancer tissue. Patients drink the contrasting agent a few hours before surgery. The solution is absorbed by tumor cells. The cells then turn pink, helping doctors remove the tumor without damaging key parts of the brain.
Recovering from surgery
Recovery from brain tumor surgery depends on the size and location of the tumor. Most side effects are temporary, but in rare cases they are permanent. These side effects include impacts on speech and movement.
Patients should begin therapy to help improve their speech and/or movement the day after surgery. These can include speech therapy, physical therapy and occupational therapy. Most patients start therapy the day after surgery. They usually begin walking with physical therapy and performing basic tasks like brushing teeth with occupational therapy. In some cases, the therapists may recommend a short stay in rehabilitation facility after they are discharged from the hospital.
Laser interstitial thermal therapy
Laser interstitial thermal therapy (LITT) is a treatment for primary and metastatic brain tumors that are hard to reach with conventional surgery or do not respond to stereotactic radiosurgery.
During the procedure, doctors implant a laser catheter into the tumor and heat it to temperatures high enough to kill cancer cells.
Getting LITT treatment
LITT is a minimally invasive treatment. In most cases it can be performed with just a two- to three-millimeter incision in the scalp. Only a very small area of hair needs to be shaved and the procedure itself takes just a few minutes to perform. Patients are put under general anesthesia and usually spend just one night in the hospital.
Recovering from LITT
Most patients who get LITT can go home the day after treatment and can quickly return to normal activities like cooking, working and grocery shopping.
Side effects of LITT include a mild headache caused by swelling in the area of LITT treatment. This is typically managed with a small dose of steroids over a short period of time.
Radiation therapy
Radiation therapy uses powerful, focused beams of energy to kill cancer cells.
Radiation therapy may be able to stop or slow the growth of brain tumors that cannot be removed with surgery. It may be used, alone or in combination with other treatments.
There are many types of radiation therapy. Almost all glioblastoma patients who get radiation receive intensity modulated radiation therapy, or IMRT.
This treatment focuses multiple radiation beams of different intensities directly on the tumor for the highest possible dose. There are different types of IMRT treatment, including volumetric modulated arc therapy, or VMAT.
Learn more about radiation therapy.
Getting IMRT
Patients receiving IMRT treatment first start with a CT scan simulation. This helps doctors plan the angles and shapes of the radiation beams that will be used for treatment. During simulation, brain tumor patients will be fitted with a mesh mask. The mask will hold the patient’s head in an exact position during treatment. This helps doctors deliver as much radiation to the tumor as possible while limiting exposure to healthy tissue. Patients can see and breathe through the mask without any trouble.
IMRT treatments usually begin about one week after simulation. Most patients get one treatment a day, Monday through Friday, for six weeks. Other patients only need three to five weeks of treatment.
Each session lasts around 30 minutes total. Most of this time is used to set up the treatment. The radiation is delivered for just five to 10 minutes in most cases. Patients usually don’t feel anything during treatment. There’s no anesthesia, though patients with claustrophobia may need light sedation.
Radiation therapy side effects
Brain tumor patients who get radiation therapy usually don’t experience side effects for the first half of treatment. Side effects usually start in the second half, including:
- Fatigue
- Hair loss at the treatment site
- Mild skin irritation, similar to a slight sunburn
- Headaches
- Brain swelling that may cause the brain tumor symptoms to worsen or recur. This is usually mild and temporary and can be easily treated with medications.
Long-term side effects
Radiation therapy to the brain can cause side effects that appear several months to years after treatment is complete. Possible side effects include changes in hormone function, an increased risk of stroke and changes in processing speed and memory.
These side effects depend on the location of the tumor and how much radiation the patient gets. Overall, though, serious side effects are rare, and the benefits of radiation therapy far outweigh the risks.
Chemotherapy
Chemotherapy drugs kill cancer cells, control their growth or relieve disease-related symptoms. Chemotherapy may involve a single drug or a combination of two or more drugs, depending on the type of cancer and how fast it is growing.
Chemotherapy is a standard treatment for many primary brain tumors, including glioblastoma. Patients are closely monitored while on chemotherapy, and their treatment may be adjusted based on how they respond to the therapy.
Learn more about chemotherapy.
Getting chemotherapy
There are different chemotherapy treatment plans for different types of brain cancer. Patients with newly diagnosed glioblastoma typically get chemotherapy pills. These patients typically get the chemotherapy pills in combination with radiation therapy, followed by the pills alone.
Patients with recurrent glioblastoma may be offered further chemotherapy treatment, either as pills or by IV. This treatment may be a standard treatment option or part of a clinical trial.
Chemotherapy side effects
The side effects of chemotherapy can include gastrointestinal symptoms, hair loss, fatigue and an increased risk of infection. Patients should talk to their doctors about ways to prevent or limit the side effects of chemotherapy.
Chemotherapy can also lead to drops in blood cell production. During treatment, the patient’s blood counts will be closely monitored to ensure they stay in a safe range.
Learn more about the side effects of chemotherapy.
Targeted Therapy
Targeted therapy drugs are designed to stop or slow the growth of cancer on a cellular level. They interfere with, or target, molecules or genes that support the spread of cancer.
Based on the characteristics of their tumor cells, only a small number of patients with glioblastoma are eligible for targeted therapy.
Read more about targeted therapy.
Getting targeted therapy
Patients with glioblastoma on targeted therapy typically get the medicine orally, as a pill. Patients often take these pills once a day for as long as they are effective.
Targeted therapy side effects
Targeted therapy side effects for patients with glioblastoma are often mild, though they can be more serious in some cases.
Some patients experience rash or gastrointestinal issues such as diarrhea, constipation, and nausea/vomiting. Patients should talk to their care team about ways to treat these and other side effects.
Learn more about the side effects of targeted therapy.
Tumor treating fields
Tumor treating fields emit radio waves in the brain that are meant to slow or stop the multiplication of cancer cells. This treatment requires patients to shave their heads and wear an adhesive skull cap with wires attached to a battery pack for 18 hours a day.
Tumor treating fields side effects
Side effects of tumor treating fields are usually mild. Patients report skin irritation and a tingling sensation on the scalp. Other, less common, side effects include headaches, muscle twitching and trouble sleeping.
Your care team can help you manage side effects of this treatment.
Clinical Trials
Clinical trials are a key part of MD Anderson's mission to end cancer. MD Anderson uses clinical trials to find better ways to prevent, diagnose and treat cancer. Trials could include new treatments or new combinations of existing treatments.
Treatment at MD Anderson
Glioblastoma is treated at our Brain and Spine Center and Proton Therapy Center.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.

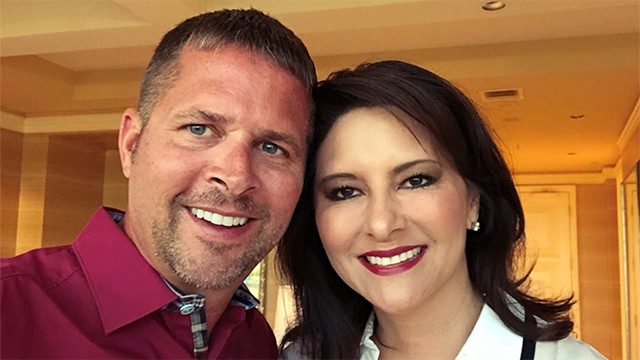
Glioblastoma survivor: ‘MD Anderson is a blessing’
When it comes to his glioblastoma diagnosis, Chris Cook is inspired by his faith, his family and his doctors at MD Anderson.
Post-holiday run leads to glioblastoma diagnosis
On Dec. 26, 2022, Chris was relaxing at home in Holland, Michigan. When his then-fiancée, Essie, left for work, Chris went on a six-mile training run with his German Shepherd, Sully.
“Around mile four, I got this metal taste in my mouth. I thought it was because of old cavities,” Chris recalls. “By mile five, I was feeling nauseous. I was starting to see white and felt my body going down.”
Chris awoke to police officers, bystanders and Sully. He was alert but could not speak. Paramedics took him to a hospital where doctors administered tests and a CT scan. “Everything was clear, I was able to speak with the doctors, and the hospital sent me home,” says Chris.
Weeks later, Chris received a letter from the State of Michigan, documenting his case as a “possible seizure.” He would need a doctor’s note clearing him to drive or to wait six months before driving again. Chris’ primary care doctor recommended that he see a neurologist.
“Things got a little more concerning when I saw the neurologist because my non-contrast CT scan showed a mass,” he says. Chris and his family immediately began searching to find the best cancer hospital when they learned he had a brain tumor. “Our research kept showing that MD Anderson was No. 1.”
Putting his trust in his MD Anderson care team
Chris first came to MD Anderson in February 2023. He met with neurosurgeon Sherise Ferguson, M.D., and neuro-oncologist Ashley Aaroe, M.D.
“Dr. Ferguson explained all aspects of the surgery, including risks to mobility connected with operating near the right vessel,” Chris says. “She discussed her plan to get around that vessel and jumped into this whirlwind, literally fighting with me.”
Reflecting on his meeting with Aaroe, Chris says, “I couldn’t have asked for a better head coach in this tough battle. She went above and beyond in answering my questions and in making sure I was able to digest the details about chemotherapy, radiation and medication.”
Leading up to surgery, Chris thought about the meetings with his doctors. “I remember asking Dr. Ferguson, ‘Looking back on your life, is this something you always wanted to do?’ She responded, ‘When I was a little girl, the only other thing I wanted to be was a ninja.’”
Chris’ brain tumor treatment
In February, Dr. Ferguson removed a 1.54-centimeter tumor in Chris’ brain. The operation involved the right middle cerebral artery and lasted more than 9 hours. “My ninja did a great job,” says Chris. “Our lives collided for her to save mine. As a surgeon, she didn’t just become a ninja; she became a samurai. And instead of a sword, she has a scalpel and knows how to operate with the best of them.”
Four weeks after surgery, Chris started 42 days of chemotherapy followed by six weeks of radiation therapy. A month after that, he started interval chemotherapy.
Aaroe manages Chris’ treatment plan. “We have a true partnership,” says Chris. “She keeps expectations real, keeps me centered about the medication I’m taking, and does a great job of coaching me.”
Chris travels to MD Anderson every other month for an MRI and a checkup with Dr. Aaroe’s team. In the non-MRI months, Chris sees doctors in Michigan for blood work and chemotherapy release-to-start sequence. His MD Anderson team collaborates with his local care team as needed.
Thankful for his MD Anderson care team
Chris says he received the same level of exceptional care from other MD Anderson specialists, such as radiation oncologist Subha Perni, M.D., and her team of nurses, as he did from Aaroe and Ferguson.
“It’s humbling how these professionals are so compassionate and genuinely care for me,” says Chris, calling MD Anderson a blessing. “Everyone who is going through cancer hopes that miracles are true. I met an entire team of miracles with my doctors, nurses and dietitians.”
Chris adds that MD Anderson did more than save his life. “The success of my surgery made it possible for me and Essie to get married on Sept. 30, 2023,” he says. “Everyone talks about bucket lists. Mine is all about the people who matter in my life and letting them know how amazing they are to me.”
Request an appointment at MD Anderson online or call 1-877-632-6789.
Why my wife had an awake craniotomy to treat glioblastoma
By the time my wife, Priscilla, was diagnosed with an aggressive brain tumor called glioblastoma, her condition was so serious that she needed emergency surgery just to prevent a fatal stroke. The local neurosurgeon who performed the procedure did his best, but he was unable to completely remove the tumor, due to its location deep inside her brain.
We consulted several other brain surgeons afterward, but nobody would agree to try again. They said a second surgery would offer Priscilla no benefit, and suggested we keep her comfortable and let nature take its course.
Instead, we went to MD Anderson. And today, nearly seven years later, Priscilla is still here.
My wife’s glioblastoma symptoms
Looking back now, I think my wife first started showing symptoms of glioblastoma in 2012, three years before her diagnosis. Around Priscilla’s 40th birthday, she began acting strangely. She started getting really forgetful, saying odd things at inappropriate times, and just acting completely checked out. She’d also have a single glass of wine sometimes and then not be able to stand up.
Things finally came to a head in 2015, when Priscilla stayed in bed all week during a Florida vacation with her girlfriends. She also said such outlandish things during that trip that a few of them privately approached me to express their concern. I took her to a local hospital when she returned. That’s when we discovered Priscilla’s odd behaviors were symptoms of a brain tumor.
My wife’s glioblastoma treatment
At MD Anderson, we met first with neurosurgeon Dr. Frederick Lang. He mapped out Priscilla’s remaining tumor with scans, then conducted an all-day cognitive assessment to get a baseline of how her brain was functioning. The next day, he performed an awake craniotomy, in which anesthesiologist Dr. David Ferson actually woke Priscilla in the middle of the brain surgery, so they could talk to her and monitor her brain functions during the tumor removal.
I had no idea an awake craniotomy was even an option. Now, I know it was to make sure the doctors knew exactly where the part of Priscilla’s brain was that managed speech, so they wouldn’t damage it while they were removing the remaining tumor. The idea of an awake craniotomy was scary and a little freaky, but also really fascinating. I’m glad it was an option.
Afterward, they put Priscilla back to sleep and closed the opening in her skull. It went really well. Dr. Lang was able to remove about 99% of the remaining tumor. Then, we had to wait for the pathology report to come back. It was a tense couple of weeks.
Genetic mutation means more treatment options
Once the pathology results came back, we all felt very relieved. Dr. Lang confirmed that Priscilla’s brain tumor was glioblastoma. It also was “MGMT methylated” and had a genetic mutation called IDH1. This meant that any remaining cancer cells in Priscilla’s body should respond well to chemotherapy.
We consulted with radiation oncologist Dr. Susan McGovern and neuro-oncologist Dr. Barbara O’Brien, who recommended six weeks of chemoradiation. Priscilla would undergo radiation therapy while also receiving chemotherapy. This would make both treatments more effective.
Priscilla began receiving chemoradiation in September 2015 and finished her treatments the following month. She also completed 12 additional cycles of chemotherapy in November 2016.
The scariest part of cancer for me
We all know that Priscilla’s cancer could still come back someday. But there’s no reason to sit around thinking about it. We just try to keep things as normal as possible, and only acknowledge cancer as a reality when we have to — usually at Priscilla’s follow-ups. She still gets a brain scan at MD Anderson every six months, and will for the rest of her life.
My wife doesn’t have quite as much energy as she used to. But the core of who she is remains the same, so we still enjoy going out to dinner together, traveling and spending time with our friends and families.
To me, the scariest part of a cancer diagnosis is the unknown. But it’s been seven years now since my wife was diagnosed, and she’s still here. She’s also getting to watch our kids grow up. So, we’re all very grateful.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
7 glioblastoma myths
Last updated Sept. 11, 2023
Glioblastoma is the most common and aggressive primary brain tumor in adults. Although it’s considered a rare cancer, with about 12,000 new diagnoses each year, it’s gained increased visibility recently with the diagnoses of a few high-profile people.
- Related: Glioblastoma symptoms
As a neuro-oncologist and the clinical medical director of MD Anderson’s Brain and Spine Center, part of my job is to make sure glioblastoma patients and their families understand this disease and how it will affect them. Unfortunately, as I’ve learned, there are many myths and misconceptions about glioblastoma.
Here’s the truth about seven glioblastoma myths I commonly hear.
1. Myth: Cell phones cause glioblastoma.
Fact: To date, there is no established link that cell phones cause glioblastoma. Several different studies have failed to find clear evidence of a link between cell phone use and brain cancer. The number of people diagnosed with glioblastoma has remained largely stable over the past decade, while cell phone use has continued to increase.
2. Myth: There’s nothing you can do for an “inoperable” glioblastoma.
Fact: A tumor that’s considered “inoperable” at a hospital without specialized brain tumor programs may actually be operable if you seek treatment at a cancer center with the right expertise. Here at MD Anderson, our neurosurgeons successfully operate on many patients who thought their tumors were inoperable. We treat glioblastoma patients every day and have a great deal of experience and expertise in safely removing tumors. This includes glioblastomas involving brain regions responsible for important functions, such as language or movement.
Certain brain tumors that cannot be safely surgically removed may qualify for laser interstitial thermal therapy (LITT). This minimally invasive surgical procedure uses thermal heat to destroy brain tumors from the inside out. Chemotherapy and radiation therapy are also part of the standard-of-care treatment for glioblastoma.
3. Myth: Glioblastoma can be completely removed by surgery.
Fact: Even a successful gross total resection for glioblastoma always leaves behind microscopic disease. Glioblastoma has “tentacles” that reach out from the main tumor mass. These tentacles are invisible to the naked eye and even to many of our most advanced imaging technologies. A gross total resection of a brain tumor is defined as removing at least 98% or more of the contrast-enhancing tumor, which is the part of the tumor that we can see on the MRI scan when the patient is given contrast dye through an IV. An MD Anderson analysis showed that glioblastoma patients who have a gross total resection tend to live longer. However, invisible cells of cancer are always left behind in the brain after surgery. That’s why the standard-of-care treatment for glioblastoma includes chemotherapy and radiation, even after an excellent surgical resection.
4. Myth: Radiation therapy is the same for any brain tumor.
Fact: Most patients undergoing radiation therapy for glioblastoma receive photon-based radiation therapy, such as intensity-modulated radiotherapy (IMRT). IMRT uses multiple X-ray beams made of photons at different angles to treat the area where the tumor was removed and any tumor left behind, even if it’s just microscopic disease. Radiation is carefully planned and targeted to protect the healthy, normal brain.
Patients with other types of brain tumors or who require radiation to both their brain and spine may receive a different type of radiation therapy, including proton therapy. To date, proton therapy has not been shown to be more effective than the standard photon-based radiation for glioblastoma. Multiple ongoing clinical trials are investigating and further defining the role of proton radiation in brain tumors.
5. Myth: The ketogenic diet can cure glioblastoma.
Fact: No diet can cure glioblastoma. A handful of case studies and internet bloggers have claimed the keto diet may have benefits for brain cancer patients, but the idea that you can “starve” glioblastoma through diet is a myth. While the role of diet in cancer is an area of active research, we know that glioblastoma patients need nutrients – including carbohydrates – to keep their bodies strong through treatment. We recommend a balanced diet based on the New American Plate guidelines developed by the American Institute for Cancer Research.
6. Myth: Having glioblastoma means your family is automatically at increased risk for developing a brain tumor.
Fact: Glioblastoma is a brain tumor that almost always develops sporadically. Being diagnosed with glioblastoma does not mean your children or siblings are more likely to develop glioblastoma or another brain tumor. Some very rare cancer syndromes, such as Li-Fraumeni Syndrome, are associated with an increased risk for developing brain tumors and other cancers, but these patients usually are diagnosed with multiple types of cancer at a very young age.
BRCA mutations are associated with an increased risk for developing breast and ovarian cancer, but there is no known association between BRCA mutations and glioblastoma development. A few ongoing genetic studies are looking at families that have multiple relatives with brain tumors to better understand if certain inherited genes contribute to brain tumor development.
7. Myth: Chemotherapy always makes your hair fall out.
Fact: The most commonly used chemotherapy for glioblastoma is called temozolomide (TMZ), and hair loss isn’t typically one of the side effects of this chemotherapy. However, treating glioblastoma with radiation therapy to the brain can cause hair loss around the part of the head where the radiation beam enters. After radiation is complete, the hair almost always grows back.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
What is astrocytoma, and how is it different from glioblastoma?
Astrocytoma and glioblastoma are two types of brain tumors. Recently, the World Health Organization (WHO) changed how these tumors are classified.
We asked neurosurgeon Chibawanye Ene, M.D., Ph.D., to explain the different types of astrocytoma brain tumors, as well as how astrocytoma differs from glioblastoma.
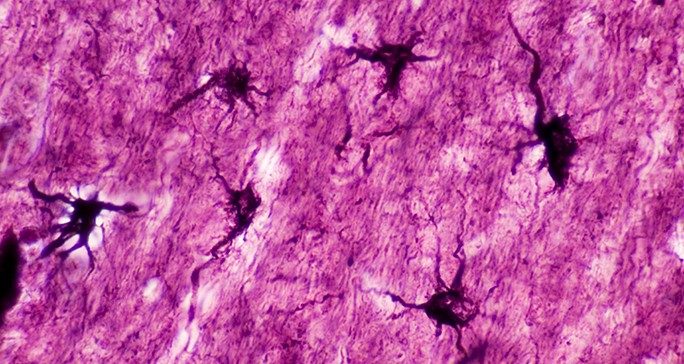
What is an astrocytoma?
Astrocytoma is a type of brain tumor. Astrocytoma brain tumors grow from astrocytes. An astrocyte is a type of cell in the nervous system. These cells get their name from their shape: they look like stars. Astrocytes help nerves work properly.
Astrocytoma develops when astrocytes grow abnormally. It’s not known exactly what causes an astrocytoma to form. Certain genetic mutations are associated with astrocytes growing out of control and becoming tumors. Still, scientists are not sure exactly what causes abnormal astrocyte growth.
Astrocytes are glial cells. Glial cells support the functions of the nervous system. Glial cells are found in the brain, spinal cord and elsewhere throughout the nervous system. Astrocytoma is a type of glioma (brain tumor).
What are the types of astrocytoma?
Astrocytomas are classified by the WHO from Grade 1 to Grade 4. Astrocytoma Grade 1 and astrocytoma Grade 2 are considered low-grade astrocytomas.
Low-grade astrocytoma includes pilocytic astrocytoma (WHO Grade 1). Pilocytic astrocytoma usually occurs in children. It is not considered cancerous because it does not spread in the brain. Pilocytic astrocytoma is rare in adults.
WHO Grade 2 astrocytoma tumors are also considered low-grade astrocytomas. But they grow faster than Grade 1 tumors and can affect more parts of the brain than Grade 1 astrocytomas. Grade 2 astrocytomas are more common among young adults.
What’s a Grade 3 astrocytoma?
Some low-grade astrocytomas progress to high-grade tumors (WHO Grade 3 or 4). Astrocytoma Grade 3 and astrocytoma Grade 4 are considered high-grade astrocytomas. High-grade tumors are fast-growing and aggressive.
WHO Grade 3 astrocytoma usually affects adults. Previously, Grade 3 astrocytoma was called anaplastic astrocytoma. Recently, the WHO revised its terminology. The term “anaplastic” is no longer used. Instead, these tumors are simply called Grade 3 astrocytomas.
Is Grade 4 astrocytoma the same as glioblastoma?
Until recently, glioblastoma was considered a Grade 4 astrocytoma brain tumor—the most aggressive astrocytoma.
Today, however, glioblastoma and astrocytoma are classified based on the presence or absence of a mutation in an enzyme called isocitrate dehydrogenase (IDH).
- Astrocytomas are all IDH-mutant tumors. This means they have a mutation in their IDH enzyme.
- Glioblastomas are all IDH-wild-type because they do not have IDH mutations.
Glioblastoma has a different molecular profile than Grade 4 IDH-mutant astrocytoma. Therefore, glioblastoma is no longer believed to evolve from a lower-grade astrocytoma. Still, both glioblastoma and Grade 4 astrocytoma are aggressive, cancerous tumors.
How do doctors know if a tumor is IDH-wild-type or IDH-mutant?
A doctor removes the tumor to biopsy it. Then, scientists run lab tests to determine whether the tumor is IDH-wild-type or IDH-mutant.
What are the signs and symptoms of astrocytoma?
Signs and symptoms of astrocytoma include headaches, blurry or double vision, seizures, trouble with balance and coordination, and mood changes.
What causes astrocytomas?
The precise causes are not known. Astrocytoma may be associated with certain genetic risk factors. Some hereditary syndromes, like Li-Fraumeni syndrome, Turcot syndrome, and von Hippel-Landau disease, may be connected to astrocytoma.
How is astrocytoma treated?
Astrocytoma is difficult to treat because the tumors are mixed with healthy tissue in the brain. The higher the grade of the tumor, the more likely that surgery will be accompanied by medication and radiation.
Grade 1 astrocytoma brain tumors, if completely removed by surgery, do not need additional treatments. Grade 2 astrocytoma may be treated with both surgery and chemotherapy. Whether radiation is used depends on factors such as age and how much tumor is left after surgery.
Grade 3 astrocytoma and Grade 4 astrocytoma brain tumors usually require surgery, radiation, and chemotherapy. That’s because these high-grade tumors spread within the brain and cannot be completely removed by surgery. Therefore, after surgery, chemotherapy and radiation are used to kill the tumor cells that spread outside of the area of surgery.
Today, we have more treatment options than ever before to manage astrocytoma. Modern surgical procedures enable surgeons to be more precise and effective when they remove tumors. Techniques like fluorescence-guided surgery and brain mapping also allow surgeons to more precisely target areas of the brain during surgery, minimizing impact on healthy areas.
In some cases, we can use radiation therapy instead to treat tumors without surgically opening the skull. For patients who don’t respond to radiation therapy, we can use laser interstitial thermal therapy (LITT) to kill the tumor.
MD Anderson is also testing next-generation brain tumor treatments through clinical trials. These treatments include using viruses or natural killer T-cells to destroy cancer cells. Results from these clinical trials will help determine whether these therapies can become part of the standard treatment for brain tumors.
Request an appointment at MD Anderson online or call 1-877-632-6789.

‘How I knew I had a brain tumor’: 4 survivors share their symptoms
Headaches and seizures are common brain tumor symptoms. But they can also be caused by other medical conditions.
So, how can you tell when a symptom is due to a brain tumor? And when should you see a doctor?
For more insight, we spoke with neuro-oncologist Shiao-Pei Weathers, M.D., and four survivors, who shared their first brain tumor symptoms and what led them to see a doctor.
Headache
Shelby Espinosa had had headaches in the past; doctors said they were related to back pain. But at age 22, she got a headache so severe that it caused her to stop mid-conversation.
“I had to stop talking and just hold my head,” she recalls. “It was so intense that I couldn’t think or respond. The pain would come and go, but the headache lingered for three days.”
Her back pain was gone, so she knew this was different. At the urging of her mom and then-fiancé, Shelby went to the emergency room, where she had a CT scan of her brain. Results revealed a tumor the size of a kiwi pressing against her brainstem. She had surgery to remove it, and a biopsy confirmed it was a type of brain tumor called medulloblastoma.
“Headaches that may indicate a brain tumor typically feel distinctly different from headaches you’ve had before,” says Weathers. “For example, people with chronic migraines are used to having headaches, but their headache usually feels the same each time.”
See a doctor if you have a history of headaches and suddenly have a new type of headache. Warning signs could be a headache that:
- wakes you up from sleep
- is worse in the morning
- feels worse when you’re lying flat
- causes nausea and vomiting that won’t go away
“Other potentially concerning signs could be a headache that lingers for days or weeks (especially if you rarely get headaches), or a headache that is accompanied by other symptoms, such as weakness, numbness, tingling or vision changes,” adds Weathers.
This was the case for Sean O’Brien. He was diagnosed with a brain tumor called juvenile pilocytic astrocytoma at age 20. He’d been suffering from a headache for years but didn’t find it too concerning because his family has a history of migraines and allergies. That was until the headache worsened during his sophomore year of college.
“At one point, the headache got so bad I sought out medical services on campus,” recalls Sean. “They told me I was overtired and needed to rest. Eventually, I did start to feel a little better.”
But then more symptoms arose.
He couldn’t sleep at night. And he began having blind spells where his vision would suddenly go out and return after a few moments. This started happening multiple times a day.
“I finally told my parents what was going on, and they got me to a doctor while I was home on Thanksgiving break,” says Sean. “The doctor discovered fluid buildup in my brain, and scans revealed a brain tumor.”
Seizure
Colin Clarke was playing soccer when he felt numbness on the left side of his face under his eye. Moments later, it happened again. Then he passed out.
“The next thing I know, I was on a gurney and put in an ambulance,” says Colin, who was 45 at the time. “I didn’t realize I’d had a seizure. I’d just headed the soccer ball! But I was told I had several seizures in the ambulance.”
He was later diagnosed with a grade II oligodendroglioma.
“A seizure is your body’s way of telling you something is going on medically. Sometimes it could be the hallmark of a new brain tumor that has yet to be discovered,” says Weathers. “But it doesn’t always mean a brain tumor. Any of us can seize under certain circumstances; for example, if your sodium drops low enough. Every person’s threshold to have a seizure is different.”
On two separate occasions, 39-year-old Chris Cook experienced a metallic taste in his mouth. It was subtle and sudden, and he assumed it was due to old cavities. Two weeks later, he noticed the metallic taste again while running with his dog. He began to feel faint. Then he blacked out.
“I woke up to my dog protecting me, first responders and the good Samaritans who called them to help me,” Chris recalls. “It was hard for me to comprehend what was happening, and I could not speak coherently. After a few minutes, I could think clearly, but I was unable to verbally express my thoughts until I was loaded into the ambulance.”
A neurologist diagnosed him with glioblastoma, the most aggressive type of brain tumor.
“A lot of patients think seizures are when your body stiffens all over, and you’re jerking on the ground losing consciousness because that’s what they show on TV,” says Weathers. “But seizures come in different types. It could be a flash of colored lights, stiffening and/or jerking of the face, arm and/or leg, or a period where you’re suddenly confused or unable to speak. It can also be an abnormal and typically foul smell or taste. Seizures usually present the same way each time.”
If it’s your first time having a seizure, see a doctor.
“It may not mean you have a brain tumor, but it could be indicating something else is going on in your body,” says Weathers. “The seizure is a warning sign to seek medical attention.”
Symptoms vary depending on the brain tumor's location
The type of symptom and its severity depend on where the tumor is in the brain.
Weathers classifies brain tumor symptoms into two buckets: global and focal. A global symptom is a more general symptom indicating something is growing in the brain and causing a buildup of pressure. A focal symptom tells you where the tumor likely is in the brain.
“If you have a constant headache for weeks that makes you nauseous or vomit, that’s a global symptom,” explains Weathers. “If you have anything growing in your brain, it will give you a headache if it grows large enough and starts pushing. But that doesn’t tell me exactly where it might be.”
Sometimes a brain tumor can cause a certain symptom based on where it’s growing in the brain. Depending on the location, you may have:
- difficulty speaking or understanding
- changes in vision, like a visual field cut or double vision
- weakness in the face, arm and/or leg
- numbness or tingling in the face, arm and/or leg
- hearing loss
- trouble swallowing
- slurred speech
Data suggests some symptoms are more common with certain types of brain tumors.
“It’s not a perfect correlation, but we tend to see seizures more often in patients with oligodendrogliomas than in patients with astrocytomas,” says Weathers.
Bottom line: See a doctor for new or different brain tumor symptoms
Brain tumor symptoms can be subtle, like a vision change. Or they can be more urgent, like a first-time seizure.
“Whether you visit an emergency room or make an appointment with your primary doctor may depend on the severity of your symptoms and how sick you feel,” notes Weathers. “If you have a new or different symptom that is concerning you or a family member, err on the side of caution. Brain tumor symptoms can mimic those of other medical conditions, so it’s important to see a doctor to get checked out.”
Request an appointment at MD Anderson online or call 1-877-632-6789.

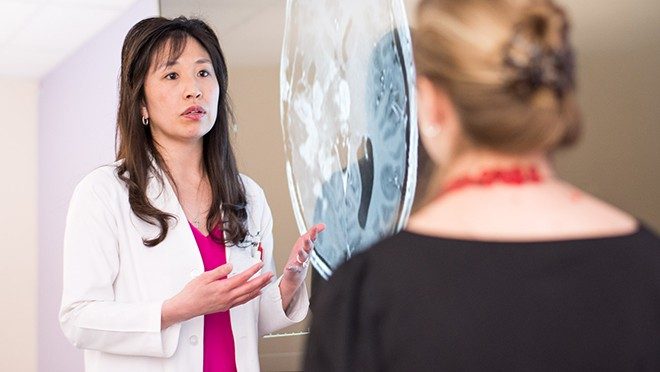
The BrainSuite intraoperative MRI images the brain during surgery, helping neurosurgeons safely remove as much of the tumor as possible.

Stereotactic radiosurgery (SRS) uses dozens of tiny radiation beams to accurately target brain tumors with a single high dose of radiation.
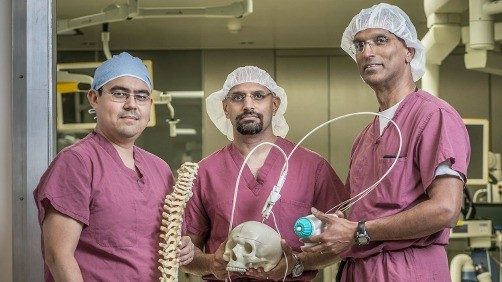
Neurosurgeons Cludio Tatsui, M.D., Ganesh Rao, M.D. and Sujit Prabhu, M.D., are pioneers in the field of laser interstitial thermal therapy.

The Brain and Spine Center at MD Anderson conducts neuro-assessments that help doctors understand and manage the impact of glioblastoma treatment.

Intensity modulated radiation therapy focuses multiple beams of radiation with different intensity levels directly on the tumor.

Navigated transcranial magnetic stimulation highlight key areas of speech and motor function in the brain, helping surgeons plan their procedures.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention and Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
