request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Glioblastoma
Glioblastoma is the most common and most aggressive form of primary brain cancer, or cancer that starts in the brain. All glioblastomas are classified as grade 4 tumors, meaning they contain the most abnormal-looking cells and grow rapidly.
Glioblastoma is the most common and most aggressive form of primary brain cancer, or cancer that starts in the brain. All glioblastomas are classified as grade 4 tumors, meaning they contain the most abnormal-looking cells and grow rapidly.
What is glioblastoma?
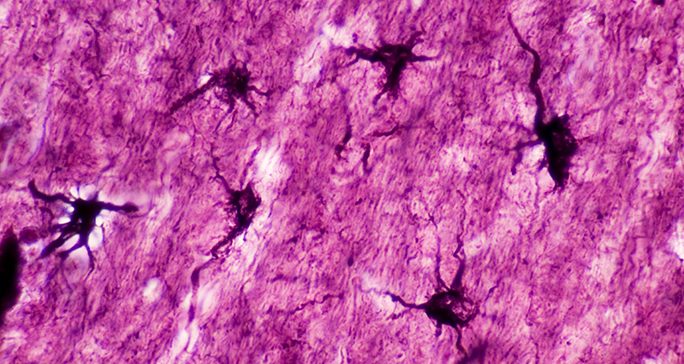
Glioblastoma begins in star-shaped brain cells called astrocytes. Astrocytes help protect the brain from diseases in the blood and provide it with nutrients.
Astrocytes are a type of glial cell. Glial cells supply the brain with nutrients and give the brain its shape. They also protect neurons from one another and create a stable chemical environment in the brain.
Glioblastoma develops when a glial cell mutates and starts multiplying rapidly.
The disease can start anywhere in the brain, but it usually begins near the forehead or the bottom of the brain.
The area near the forehead is the frontal lobe. It plays important roles in speech, voluntary movement, behavior and memory.
The area near the bottom of the brain is the temporal lobe. It creates new memories, processes language, and processes input from the senses of hearing, sight, taste and touch.
Who gets glioblastoma?
Most glioblastomas are random, with no known cause.
Glioblastoma is most common among men, people age 50 and older and white people.
Patients who had a prior cancer that was treated with radiation therapy to the head have a slightly increased chance of developing glioblastoma. Most patients who get radiation to the head do not develop this cancer, and the benefits of radiation therapy are far greater than the risks.
Symptoms
Glioblastoma symptoms include headaches, seizures and changes in mood and behavior.
Get more information, including other possible diagnoses and when to see a doctor, on our glioblastoma symptoms page.
Diagnosis
Doctors diagnose glioblastoma by removing suspected cancer tissue and studying it under a microscope. They also conduct tests to learn the genetic mutations in the tumor cells.
Learn more about how glioblastoma is diagnosed.
Treatments
Glioblastoma treatments include surgery, radiation therapy, chemotherapy and tumor treating fields.
Learn more about these treatments, including side effects and recovery times, on our glioblastoma treatment page.
Glioblastoma survival rate
There is currently no cure for glioblastoma. The median length of survival after a diagnosis is 15-18 months, while the disease’s five-year survival rate is less than 10%.
These statistics reflect the challenges of treating the disease.
As glioblastoma grows, it forms microscopic branches that can spread into different parts of the brain. These branches make it nearly impossible to remove the entire tumor with surgery. In addition, a single tumor contains many different types of cells. A drug that works for some cells may not work for all.
Glioblastomas are also aggressive because they do not have a genetic mutation in the IDH gene. Brain tumors with IDH mutations tend to grow more slowly and respond better to treatment than tumors without the mutation.
While glioblastoma is difficult to treat, clinical trials at MD Anderson are exploring new radiation therapy, chemotherapy and immunotherapy strategies to fight this disease. Other trials are designed to improve patients’ quality of life.
Seeking a second opinion on a glioblastoma diagnosis
Glioblastoma is a complex disease that requires expert treatment. Understanding the exact subtype of glioblastoma can help doctors develop the best treatment plan for each patient. A second opinion can help ensure every patient is getting the best treatment. Learn more about second opinions at MD Anderson.
What are the risk factors for glioblastoma?
Anything that increases the chance of developing a particular disease is a risk factor. The risk factors for glioblastoma are:
- Biological sex: Males are more likely to develop glioblastoma than females.
- Age: Most cases of glioblastoma are diagnosed in people age 50 and older.
- Race: White people are at an increased risk for developing glioblastoma compared to people of other races.
- Prior radiation to the head to treat another cancer. This is only a small risk, though. Most patients who get radiation to the head do not develop the disease. The benefits of radiation therapy are far greater than the risks.
Is glioblastoma hereditary?
Certain genetic changes that are passed down from parent to child are connected to glioblastoma. These include Li Fraumeni syndrome, neurofibromatosis type 1 and Turcot syndrome. Learn more about hereditary cancer syndromes.
MD Anderson is #1 in Cancer Care
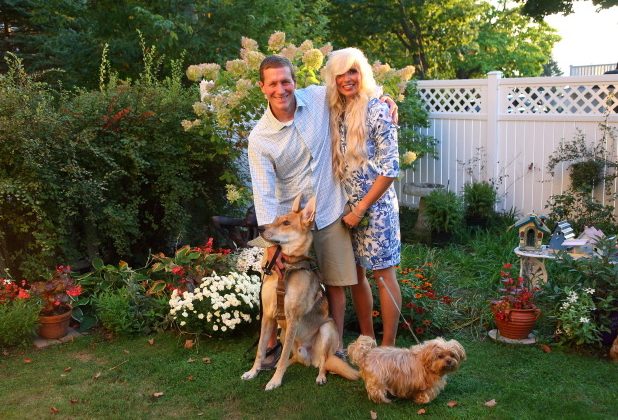
Glioblastoma survivor: ‘MD Anderson is a blessing’
When it comes to his glioblastoma diagnosis, Chris Cook is inspired by his faith, his family and his doctors at MD Anderson.
Post-holiday run leads to glioblastoma diagnosis
On Dec. 26, 2022, Chris was relaxing at home in Holland, Michigan. When his then-fiancée, Essie, left for work, Chris went on a six-mile training run with his German Shepherd, Sully.
“Around mile four, I got this metal taste in my mouth. I thought it was because of old cavities,” Chris recalls. “By mile five, I was feeling nauseous. I was starting to see white and felt my body going down.”
Chris awoke to police officers, bystanders and Sully. He was alert but could not speak. Paramedics took him to a hospital where doctors administered tests and a CT scan. “Everything was clear, I was able to speak with the doctors, and the hospital sent me home,” says Chris.
Weeks later, Chris received a letter from the State of Michigan, documenting his case as a “possible seizure.” He would need a doctor’s note clearing him to drive or to wait six months before driving again. Chris’ primary care doctor recommended that he see a neurologist.
“Things got a little more concerning when I saw the neurologist because my non-contrast CT scan showed a mass,” he says. Chris and his family immediately began searching to find the best cancer hospital when they learned he had a brain tumor. “Our research kept showing that MD Anderson was No. 1.”
Putting his trust in his MD Anderson care team
Chris first came to MD Anderson in February 2023. He met with neurosurgeon Sherise Ferguson, M.D., and neuro-oncologist Ashley Aaroe, M.D.
“Dr. Ferguson explained all aspects of the surgery, including risks to mobility connected with operating near the right vessel,” Chris says. “She discussed her plan to get around that vessel and jumped into this whirlwind, literally fighting with me.”
Reflecting on his meeting with Aaroe, Chris says, “I couldn’t have asked for a better head coach in this tough battle. She went above and beyond in answering my questions and in making sure I was able to digest the details about chemotherapy, radiation and medication.”
Leading up to surgery, Chris thought about the meetings with his doctors. “I remember asking Dr. Ferguson, ‘Looking back on your life, is this something you always wanted to do?’ She responded, ‘When I was a little girl, the only other thing I wanted to be was a ninja.’”
Chris’ brain tumor treatment
In February, Dr. Ferguson removed a 1.54-centimeter tumor in Chris’ brain. The operation involved the right middle cerebral artery and lasted more than 9 hours. “My ninja did a great job,” says Chris. “Our lives collided for her to save mine. As a surgeon, she didn’t just become a ninja; she became a samurai. And instead of a sword, she has a scalpel and knows how to operate with the best of them.”
Four weeks after surgery, Chris started 42 days of chemotherapy followed by six weeks of radiation therapy. A month after that, he started interval chemotherapy.
Aaroe manages Chris’ treatment plan. “We have a true partnership,” says Chris. “She keeps expectations real, keeps me centered about the medication I’m taking, and does a great job of coaching me.”
Chris travels to MD Anderson every other month for an MRI and a checkup with Dr. Aaroe’s team. In the non-MRI months, Chris sees doctors in Michigan for blood work and chemotherapy release-to-start sequence. His MD Anderson team collaborates with his local care team as needed.
Thankful for his MD Anderson care team
Chris says he received the same level of exceptional care from other MD Anderson specialists, such as radiation oncologist Subha Perni, M.D., and her team of nurses, as he did from Aaroe and Ferguson.
“It’s humbling how these professionals are so compassionate and genuinely care for me,” says Chris, calling MD Anderson a blessing. “Everyone who is going through cancer hopes that miracles are true. I met an entire team of miracles with my doctors, nurses and dietitians.”
Chris adds that MD Anderson did more than save his life. “The success of my surgery made it possible for me and Essie to get married on Sept. 30, 2023,” he says. “Everyone talks about bucket lists. Mine is all about the people who matter in my life and letting them know how amazing they are to me.”
Request an appointment at MD Anderson online or call 1-877-632-6789.

Glioblastoma survivor: ‘You can live with cancer and still have a really good life’
Focal seizures are not what you might typically imagine when you first hear the word “seizure.” They’re not the kind that makes you suddenly fall to the floor and start writhing around. These just make you space out for a few minutes, or maybe smell chocolate strongly for a second, or yawn 15 times in a row really quickly.
I was having brain fog and at least a handful of those seizures every day by January 2024. I just didn’t understand why. I knew something was wrong. But I never imagined it was a brain tumor. And, I made every excuse in the book to try to explain it: getting overheated, eating something questionable, even drinking too much the night before at a whiskey tasting party.
Finally, I couldn’t make any more excuses. The brain tumor symptoms weren’t going away. And, I wasn’t getting any better. I asked my wife to take me to the emergency room.
My glioblastoma diagnosis
CT and MRI scans done at the ER revealed a mass about the size of a thumb in my brain. It was located deep inside the hippocampus, one of that organ’s innermost structures. The neurologist on duty said it was likely cancerous, and the tumor needed to come out ASAP.
I believed him, but I also wanted a second opinion. I was only 57 at the time and otherwise perfectly healthy. It was pretty shocking to hear something was growing inside my head that needed to come out.
My wife, Wendy, works as an administrator in Pediatrics at MD Anderson. So, I knew its reputation as the best place in the world for cancer treatment. I also knew that nothing was really new to its doctors, because they see things daily that other doctors see maybe once in a lifetime. Plus, we only live about 20 miles away from the Texas Medical Center Campus.
My glioblastoma treatment
At MD Anderson, I met first with neurosurgeon Dr. Jeffrey Weinberg. After conducting his examination, Dr. Weinberg agreed that I needed brain surgery right away.
We scheduled the 9-hour craniotomy for Feb. 19, 2024. Then, I had six weeks of chemoradiation under radiation oncologist Dr. Martin Tom, followed by six more months of standard chemotherapy under neuro-oncologist Dr. Shiao-Pei Weathers.
I was hoping to try something new through AGILE, a clinical trial I joined at MD Anderson for glioblastoma patients. Sometimes you have to experiment a little to make things better. That’s why I volunteered right away to join a clinical trial.
But the standard of care for glioblastoma hasn’t really changed much over the past 20 or 30 years. So, I wasn’t terribly disappointed when I was randomly assigned to the control group. Whatever doctors were using back then was what they were still using now, so at least I’d be getting the most effective known treatment.
My life today, after glioblastoma treatment
I finished my treatments at MD Anderson in November 2024. Unfortunately, glioblastoma is likely not finished with me.
The pathology report after surgery showed my tumor cells were rated Grade 4, which is the worst one possible. Statistically speaking, a glioblastoma recurrence is almost a certainty. You can never quite get rid of all of it, no matter how skilled your surgeons are or how much they cut out. Glioblastoma always leaves little particles of itself behind.
But Dr. Weinberg and his team got out as much as they could safely. And I trust both him and MD Anderson. The average lifespan after a glioblastoma diagnosis is only 18 months. I’m already at month 16, though, and my scans are still totally clear. So, I’m already a statistical outlier.
I’m not even taking any medications right now to treat cancer. I have hardly any cognitive deficits, either, which is pretty unusual after that complex of a brain surgery. Fatigue is really the only side effect I’m still dealing with.
Even so, I couldn’t keep doing what I’d been doing as a professional firefighter. I just didn’t have the stamina. So, I had to take early retirement in April.
I wasn’t quite ready to make that transition. But it is what it is, so I tried to take it in stride. Now, I spend a lot of my time volunteering. I find a great deal of joy in that. It’s taught me that a cancer diagnosis is not necessarily the end of the line. You can live with cancer and still have a really good life.
Request an appointment at MD Anderson online or call 1-877-632-6789.
How to tie your own headscarf
An MD Anderson nurse shares how you can tie your own headscarf.
Why Choose MD Anderson for glioblastoma care?
After learning they have a brain tumor, many people feel they must schedule surgery as soon as possible. However, most brain tumor patients, including those with glioblastoma, have time to research their options.
As MD Anderson neurosurgeons have shown, removing as much of the tumor as possible, known as maximal safe resection, during the first surgery leads to better survival for glioblastoma patients. Choosing the right hospital for your first surgery or treatment is one of the most important decisions you can make as a glioblastoma patient.
Because this is a difficult cancer to treat, finding doctors with experience and expertise in treating glioblastoma is key. At MD Anderson Cancer Center, we have many of the world leaders in glioblastoma care, including top neurosurgeons, neuro-oncologists and radiation oncologists who specialize in the central nervous system. In most cases, the experts at MD Anderson are able to identify the unique characteristics of the patient's glioblastoma on a molecular level. This information may support the creation of a personalized treatment plan tailored specifically to the patient’s disease.
As a top-ranked cancer hospital, MD Anderson also is home to one of the world’s largest collections of glioblastoma clinical trials designed to improve outcomes for patients. These trials include studies of new chemotherapies, radiation therapies and immunotherapies, among other treatments.
In addition to treating the disease directly, MD Anderson’s Brain and Spine Center offers leading neuropsychology care. We monitor the impact of the disease and its treatments on patients’ cognitive health. If needed, we can adjust treatments to improve patients’ quality of life and ability to function day-to-day.
Some glioblastoma treatments are even offered beyond MD Anderson’s campus in the Texas Medical Center. Through our five Houston-area locations, glioblastoma patients throughout the region may be able to receive radiation therapy or chemotherapy from MD Anderson physicians close to home.
Learn more about glioblastoma:
You've got to believe in yourself and believe that you will beat this cancer.
Nicole Adams
Survivor
How to tie a headscarf on someone else
MD Anderson nurses share how you can tie a headscarf on another person.
Treatment at MD Anderson
Glioblastoma is treated at our Brain and Spine Center and Proton Therapy Center
Clinical Trials
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
MyCancerConnection
Prevention & Screening
Counseling
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.