request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Childhood Brain Tumors
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsBrain and spine tumors are the second most common cancers in children after leukemia. Brain tumors affect nearly 2,500 children in the United States every year, accounting for 20% of childhood cancers.
Brain and spine tumors are the second most common cancers in children after leukemia. Brain tumors affect nearly 2,500 children in the United States every year, accounting for 20% of childhood cancers.
The brain controls many important facets of everyday life, including emotions, thought, speech, vision, hearing and movement. The brain sends messages throughout the body via the spinal cord and cranial nerves in the head. The network of the brain and spinal cord is called the central nervous system (CNS). Tumors can develop in the spinal cord and cranial nerves.
The hard, bony skull protects the brain, and the bones (vertebrae) of the spine protect the spinal cord. A liquid called cerebrospinal fluid (CSF) surrounds both the brain and the spinal cord.
The brain has four main parts:
Basal ganglia: Found deeper inside the brain, these play a part in muscle movement.
Brain stem: Located at the base of the brain, the brain stem has nerve fibers that carry messages between the cerebrum and the rest of the body. A small but important area, the brain stem plays a part in breathing and heartbeat.
Cerebellum: At the back of the brain, this section helps control and coordinate movement, such as walking and swallowing.
Cerebrum: The outer and largest part of the brain. It has two halves called hemispheres and is responsible for emotions, reasoning, language, movement and the senses of seeing, hearing, smelling and touch; and the perception of pain.
Childhood brain tumor types
Because the brain and spinal cord are made up of many kinds of tissues and cells, many types of tumors – both benign and malignant– can develop in these areas. These tumors may require different treatment and have different outlooks.
Even when brain tumors are benign, they can cause serious problems. Although non-cancerous brain tumors usually grow slower than cancerous brain tumors, they may damage and press against normal brain tissue or the spine as they grow.
Childhood brain and spinal cord tumors differ from adult tumors. The location where they develop, the type of cell in which they develop, and their treatment and outlook often are different. Brain tumors are classified by the types of cells they contain. This determines how they grow and what kind of treatment they require. The brain tumors found most often in children are the following.
Medulloblastoma: This is the most common type of malignant brain tumor in children. Learn more about medulloblastoma.
Astrocytoma: These form in the cerebrum in cells called astrocytes. They usually grow slowly, but higher-grade tumors spread more quickly. Since they mix with normal brain tissue, they can be difficult to remove surgically. They may spread along pathways of CSF but seldom spread outside the brain or spinal cord. Glioblastoma is the highest grade astrocytoma and the fastest growing.
Diffuse intrinsic pontine glioma: This dangerous tumor often has a poor prognosis. It grows in a vital area of the brain called the pons, which is in the brain stem.
Ependymomas develop in the brain lining, usually in the posterior fossa or along the spinal cord in glial cells. About five percent of childhood brain tumors are ependymomas. They begin in cells that line the ventricles or central canal of the spine. Ependymomas do not usually spread outside the brain or spinal cord, but they may block CSF, causing hydrocephalus.
Primitive neuroectodermal tumors (PNET): These aggressive tumors can develop anywhere in the brain, but they are usually in the frontal, temporal or parietal lobes.
Pineoblastomas: A type of PNET that develops in pineal gland and can be difficult to treat.
Craniopharyngiomas: These slow-growing tumors start above the pituitary gland but below the brain. They may press on the pituitary gland and hypothalamus, causing hormone problems. Since they start near the optic nerves, they can cause vision problems and be difficult to remove without damaging vision.
Mixed glial and neuronal tumors: Certain tumors that develop in children and young adults (and rarely in older adults) have both glial and neuronal cell components. They tend to have a fairly good prognosis.
- Pleomorphic xanthoastrocytoma (PXA) and dysembryoplastic neuroepithelial tumors (DNETs) look as if they could grow quickly when viewed under the microscope, but these tumors tend to be fairly benign, and most are cured by surgery alone.
- Ganglioglioma is a type of tumor that has both mature neurons and glial cells. Most can be cured by surgery alone or surgery combined with radiation therapy.
Choroid plexus tumors: These rare tumors start in the choroid plexus within the ventricles of the brain. Most are benign and can be removed by surgery.
Other tumors that start in or near the brain
Meningiomas: These tumors begin in the meninges, the tissue around the outer part of the brain and spine. They may press on the brain or spinal cord. Meningiomas are almost always benign and are usually cured by surgery. If they are near vital structures in the brain, they may need additional treatment.
Chordomas start in the bone at the base of the skull or at the lower end of the spine. They can injure the nervous system by pressing on it. They usually do not spread to other areas.
Germ cell tumors: Developing from germ cells, which normally form eggs in women and sperm in men, these are rare tumors. They form in the fetus when germ cells move to abnormal locations, including the brain. Germ cell tumors of the nervous system are usually found in children, most commonly in the pineal gland or above the pituitary gland. Learn more about childhood germ cell tumors.
Brain metastases: Cancers that metastasize (spread) to the brain from other areas of the body are called metastases. These are treated differently than primary brain cancers.
Childhood brain tumors risk factors
Anything that increases your child’s chance of getting a brain tumor is a risk factor. While no definite risk factors have been found for childhood brain tumors, some things may put your child at increased risk, including:
- Radiation exposure, particularly if your child was treated with radiation to the brain for leukemia. This late effect usually is seen between 10 to 15 years after treatment.
- Rare inherited genetic conditions, including:
- Tuberous sclerosis
- Neurofibromatosis types 1 and 2
- Von Hippel-Lindau disease
- Li-Fraumeni syndrome
- Other diseases that run in certain families, including:
- Turcot syndrome
- Rubinstein-Taybi syndrome
- Gorlin syndrome (basal cell nevus syndrome)
Some cases of brain cancer can be passed down from one generation to the next. Genetic counseling may be right for you. Learn more about the risk to you and your family on our genetic testing page.
Learn more about childhood brain tumors:
Learn more about pediatric clinical trials for childhood brain tumors.
MD Anderson is #1 in Cancer Care
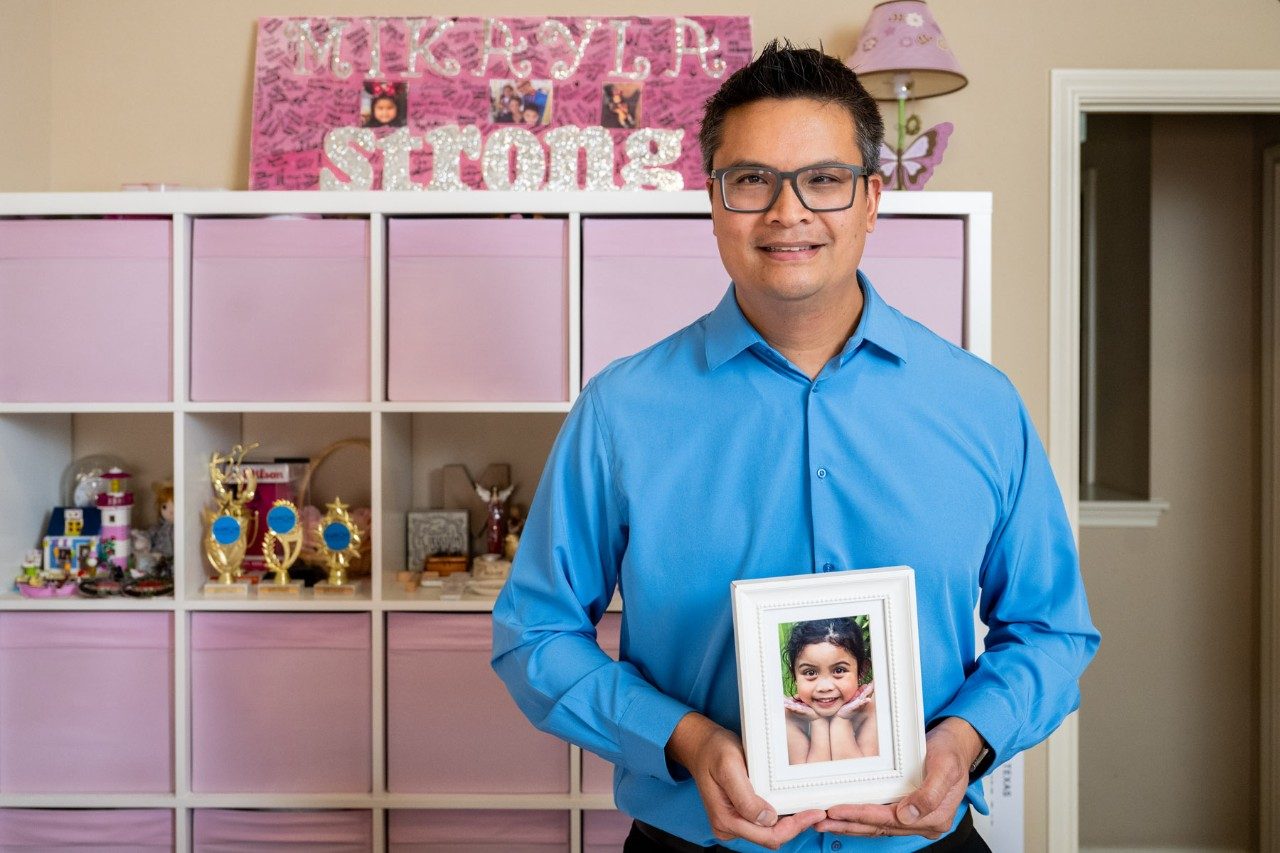
A father’s joy turns to purpose
Early in his career, Rodney Quindoy thrived on being a critical care nurse who helped patients recover from medical emergencies. Little could prepare him, though, for his own daughter’s terminal cancer diagnosis shortly after he joined MD Anderson’s Patient Safety department in 2014.
“She had such a radiant smile and charisma,” he says of Mikayla, who was diagnosed on New Year’s Eve with Diffuse Intrinsic Pontine Glioma (DIPG). “As parents, we can recall how protective we were: child-proofing the house, feeling bad when she had her first boo-boo. She was a thriving 6-year-old girl; then, out of the blue, she was diagnosed with this.”
DIPG is a rare and aggressive brain tumor that primarily affects children and is notoriously difficult to treat. In Mikayla’s case, a clinical trial at MD Anderson provided a few weeks of symptom relief before she passed away in December 2015.
A passion for patient safety
Quindoy left MD Anderson to pursue other career opportunities. During his time away, he quickly realized that MD Anderson’s commitment to safety is unparalleled. “I knew one day I would return,” he says. “The organization holds a sentimental place in our family’s heart.”
Quindoy returned to MD Anderson as a clinical patient safety specialist in 2022 – this time with a personal mission to inspire hope in caregivers, especially parents of young patients.
“MD Anderson has always set the benchmark in terms of what safety should be,” he says, citing its commitment to daily safety briefings, deep analyses of safety risks, and recent training of all employees in the principles of High Reliability Organizations. Based on data from 2023, MD Anderson maintains a five-star rating in national quality and safety rankings from Vizient and the No. 1 spot in safety.
“My passion for patient safety originated at MD Anderson,” Quindoy says. “It’s embedded in the culture.”
Carrying on his daughter’s legacy
To honor Mikayla, Quindoy picked up a set of drumsticks in May and won MD Anderson’s 2023 employee talent show, known as Anderson’s Got Talent. He dedicated his performance to Mikayla and placed her picture at the base of his drums.
“My goal was to share a message of inspiration, especially for those who've lost loved ones,” he says. “Suffering a loss is traumatic, but you have the power to rise above and become stronger than you ever thought. That’s how I carry on Mikayla’s memory and legacy.”
Request an appointment at MD Anderson online or call 1-877-632-6789.
Pediatric brain tumor parent: We're grateful for MD Anderson
When Ben Gadot’s brain tumor symptoms began in 2013, he was just 3 months old. The first sign was a visual change in his eyes.
“It was as if he was always looking down,” says Cecilia Gadot, Ben’s mom. “We could see mostly just the white part of his eyes.”
ER trip reveals childhood brain tumor
When Cecilia and her husband, Raphael, took Ben to their pediatrician, they were referred to an ophthalmologist. But Ben's health quickly started to decline. Cecilia remembers him being very fussy, crying and vomiting. They took him to a local emergency room.
A CT scan revealed a childhood brain tumor called pilomyxoid astrocytoma. Ben’s diagnosis was a Grade 2 optic pathway glioma.
Ben started chemotherapy to slow the growth of the tumor at a nearby hospital.
In 2016, he underwent tumor debulking surgery to remove as much of the tumor as possible. The tumor impaired Ben’s vision, and he started to experience precocious puberty at age 3.
In April 2021, Ben’s care team considered treating him with proton therapy but decided to keep him on chemotherapy to slow the tumor’s growth. In July 2022, Ben underwent a ventriculoperitoneal shunt surgery. By draining extra fluid in his brain, the shunt would help control pressure there.
Brain tumor growth leads to proton therapy treatments
But that September, an MRI showed a slight progression of the tumor. Ben’s care team decided it was time to start proton therapy at MD Anderson under the care of radiation oncologist David Grosshans, M.D., Ph.D. Because protons can be precisely controlled, pediatric proton beam radiation is ideal for tumors near growing healthy tissues.
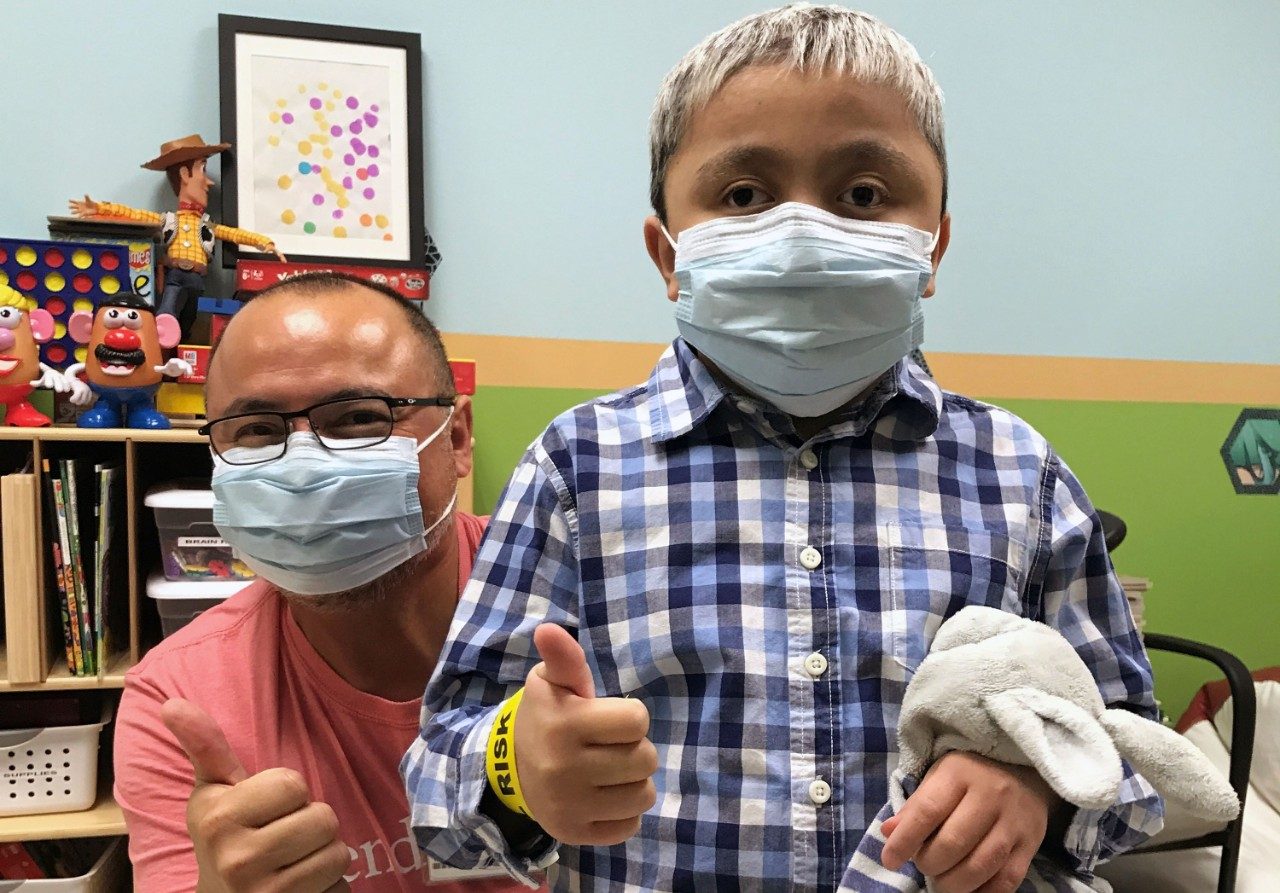
On Oct. 17, 2022, Ben started 28 days of proton therapy. With his positive attitude and the help of the child life team, he underwent treatments and MRIs without sedation. “The bond he had with his care team brought him a lot of trust and comfort,” says Cecilia.
Ben enjoyed playtime with child life assistant Leon Benavides in the playroom at the Proton Therapy Center before and after treatment.
“MD Anderson’s staff is very supportive and caring, from the front desk to the nurses, doctors, radiation therapists and, most importantly, child life specialists,” says Cecilia. “Ben’s time in the playroom with Mr. Leon was his daily reward and incentive.”
Finding gratitude with a child in cancer treatment
Cecilia encourages other parents of pediatric cancer patients to find something to be grateful for each day. “The hardest part of treatment is waiting for it to start. Once it starts, it goes pretty smoothly and quickly,” she says. “So, take time to make each day a good day.”
Ben’s appointments were scheduled early in the morning so he could continue his daily routine. Most days he was able to go to school.
On Nov. 23, 2022, a few days before Thanksgiving, Ben rang the gong with his family and care team cheering him on. “We are so grateful for MD Anderson for not only being the best place to receive proton therapy but for making Ben feel comfortable and cared for along the way.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.

How proton therapy helped my son with a childhood brain tumor
My son Benjamin was born weighing only 3 pounds. He stayed in the NICU for seven months. It was challenging and financially draining. We had a kindergartener and toddler at home, while also visiting Benjamin at the hospital every day.
When Benjamin was able to come home, he had a total parenteral nutrition (TPN) central line, an ostomy bag and a gastrostomy tube (G-tube) to receive nutrition.
By the time he was 1, he was able to eat and have the ostomy bag and G-tube removed. Life was beginning to feel normal.
At 2 years old, he jumped into a foam pit at a birthday party and came out holding his head to the side. When I asked if he felt hurt, he said no. I waited a few days thinking he had pulled a muscle in his neck. But the head tilt remained.
When I took him to his pediatrician, they sent us to physical therapy. After two weeks, nothing had improved. We saw a neurologist who said he seemed happy and healthy with no other symptoms other than a head tilt. The neurologist ordered an MRI to be safe, but I remember her telling me that she did not think they would find anything.
Before we left the hospital parking lot, I received a call saying the MRI results were in.
A childhood brain tumor diagnosis
That is when Benjamin was diagnosed with a type of brain tumor called a Grade 1 pilocytic astrocytoma. His oncologist at our local hospital recommended he start chemotherapy but suggested waiting on radiation therapy to give his body and brain time to grow so they could access the tumor better.
A few months later, tests showed the tumor had grown. His care team decided to operate. Benjamin had just turned 3 years old when he underwent brain surgery. He then had two weeks of inpatient rehabilitation. This was rough on our family because we had two little girls at home.
After six years of trying several types of chemotherapy, including two clinical trials, we were ready to try radiation therapy. I knew the tumor was still growing and Benjamin was having symptoms such as sleepiness and increased face paralysis. So, we decided to take a leap of faith, trust God and go to MD Anderson to have his tumor treated with proton beam therapy.
Proton therapy is an advanced type of radiation treatment that uses a beam of protons to deliver radiation directly to the tumor, destroying cancer cells while sparing healthy tissues. As a result, it minimizes side effects to prevent long-term complications. Because of the physical properties of proton beams, it is ideal for pediatric cancer patients with tumors located near growing tissues, especially in the brain, spine, eyes, ears or mouth.
Perseverance through proton therapy treatment
In Sept. 2022, when Benjamin was 10 years old, he started proton therapy at MD Anderson under the care of Dr. David Grosshans. He had a wonderful experience at MD Anderson Proton Therapy Center. Benjamin told me it was the easiest treatment he has been through. He bonded with his care team and loved taking naps during treatment. On Nov. 4, he celebrated his last treatment by ringing the gong.
During treatments, he did not have side effects. But after he completed proton therapy, he experienced some numbness on the left side of his body and weakness in his leg. He continues to go to physical therapy and that helps improve his strength.
Benjamin is doing well, and the tumor is stable. He is working hard to get caught up at school. Missing school for treatment affected his learning the most.
My advice to other parents is to bring a book and a snack to treatment. Keep a watchful eye on the patient and most of all, remember to take it one day at a time.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.

Childhood brain tumor diagnosis fuels commitment to future generations
As he approaches his 30th birthday, Harrison Elias often looks around and cannot believe how far he has come. After completing his master’s degree in exercise science/strength and conditioning at Springfield College and stints as a Division I college strength and conditioning coach at the University of Rhode Island and Boston College, he is now the founder/owner of a sports performance facility in Glastonbury, Connecticut. He also is a pediatric brain cancer survivor who has been in remission for more than 20 years.
“Some days I can deadlift 400 pounds but can barely pick up a pencil with my left hand,” says Harrison, who has limited motor function on the left side of his body, a lasting reminder of the brain tumor surgery he underwent as a child. “I have had bad days, actually a lot of bad days, but focusing on the type of person I wanted to be in the future has always gotten me through.”
The first symptoms of a childhood brain tumor
Because he was so young at the time of his diagnosis, Harrison does not remember many of the specifics of his cancer experience. But his family began noticing something strange in the summer of 2000 when Harrison was visiting relatives in Michigan with his mother and siblings.
“They were playing cards, but he was having trouble holding the cards in the right direction. His hand was turned, so the cards were facing the others playing,” recalls Howard Elias, Harrison’s father, who hadn’t yet joined the family on their trip. “He was only 6 at the time, and I remember them saying ‘Harrison, you’re not supposed to show your cards to the other players.’ And he said, ‘I’m not doing that; I’m not turning my hand.’ That is when they knew something was seriously wrong.”
Second opinion at MD Anderson brings comfort and confidence
Harrison had a CT at a local hospital, followed by an MRI at a different hospital. They revealed a lesion on the right side of his brain, in the hypothalamus, a deep part of the brain. The doctor said his prognosis was not good. Howard knew they needed a second opinion and immediately began researching options and seeking opinions around the country.
One of those opinions came from the nation’s No. 1 cancer center. “We were living in The Woodlands at the time, so we had heard about MD Anderson,” says Howard. “We met with a pediatric oncologist, Dr. Joann Ater, and really appreciated the comprehensive, collaborative efforts of all the MD Anderson teams to work together to provide the best, all-encompassing plan of action. Within weeks, Harrison was in surgery.”
MD Anderson’s specialists determined that Harrison’s original diagnosis was not completely accurate, and they concluded he had a pilocytic astrocytoma, a type of brain cancer that is slower growing and, if surgically removed, can potentially be cured. Unfortunately, because of the location in the hypothalamus, the chance of complete surgical resection was considered low.
The Elias family met with neurosurgeon Frederick Lang, M.D., who successfully removed Harrison’s entire tumor in July 2000 and vigilantly checked his routine scans for regrowth throughout Harrison’s childhood.
Harrison’s cancer never returned, so he did not need to undergo radiation or chemotherapy treatment. Post-surgery, Harrison spent many months and years building back up his physical strength and regaining motor skills that were impacted by the cancer and surgery.
“As a young child, it was a lot of ‘sit here, do this, do that,’” remembers Harrison. “But everyone at MD Anderson knew what they were doing and that was a comfort to me, even as a kid.”
A commitment to advancing brain tumor and cancer neuroscience research
The Elias’ relationship with MD Anderson and Dr. Lang has grown over the years. They have doubled down on supporting and advancing treatment options for pediatric and adult brain cancer patients.
“As a family, we have supported Dr. Lang’s research in neuro-oncology through the Elias Family Fund for Brain Tumor Research as well as the Howard and Susan Elias Foundation for many years,” says Howard, who lost his father to glioblastoma at age 59. “Now it is time for us to increase our commitment significantly so we can play a bigger role in advancing cancer neuroscience research specifically focused on brain tumors and the nervous system.”
Howard and Susan, Harrison’s stepmother, recently made a $16.25 million gift to MD Anderson to accelerate brain tumor and cancer neuroscience research, an emerging field focused on integrating the nervous system’s role in cancer. The gift aims to extend patients’ lives and eliminate suffering through a comprehensive understanding of the interactions of the nervous system with cancer. The Elias’ generosity and foresight will also provide secure, sustainable support for generations of researchers to come as they push the limits in searching for new therapies and cures.
Inspiring others to make it through
Back in Glastonbury, Harrison continues his transformational work as he helps young athletes pursue their own dreams.
“One day I looked around the gym and all the new kids were doing their pushups with one hand closed,” Harrison remembers fondly with a smile. “That’s how I always do my pushups due to my limitations on one side, but they had no idea. They just thought that was the way to do them.”
The strength and courage that got him through surgery and recovery at age 7 continue to carry him today.
“There is no better feeling than getting stronger in the face of a challenge,” Harrison says. “Keep going, keep going, and you will make it through.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Why come to MD Anderson for childhood brain tumor care?
The Children's Cancer Hospital offers comprehensive, personalized care for benign (non-cancerous) and malignant (cancerous) brain tumors in children. Our expert, highly specialized physicians and a dedicated support staff follow your child every step of the way, collaborating and communicating closely.
Advanced diagnosis and treatment
We provide the most advanced diagnostic and treatment approaches, many of which are available at only a few hospitals in the nation. Our surgeons are top in their fields, and their expertise helps target the tumor while saving as much of the surrounding tissue as possible.
In collaboration with Children's Memorial Hermann Hospital, our pediatric brain tumor program brings together expertise from two renowned hospitals. The program ensures that patients receive timely and accurate diagnosis and individualized treatment for all types of childhood brain tumors.
Children's Cancer Hospital offers clinical trials for innovative new treatments for brain tumors in children. And, behind the scenes we are working on groundbreaking basic science research to change the future of pediatric cancer.
Treating the whole child
Children's Cancer Hospital is designed just for children, with a full range of services and amenities that help make the child and family's experience as comfortable as possible. We go beyond medical care to deliver a comprehensive experience that treats the whole child. And at Children's Cancer Hospital, you're surrounded by the strength of one of the nation's top cancer centers.
The one gift cancer gave me is perspective. Now, each day is a new day and is filled with possibilities.
Denise Rager
Caregiver
Treatment at MD Anderson
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
