Benefits of proton therapy for childhood cancer
Proton Therapy for Childhood Cancers
Proton therapy is an excellent treatment option for children, adolescents and young adults with cancerous and non-cancerous tumors that can be treated with traditional radiation. Proton therapy may limit the radiation exposure to healthy, growing tissue in pediatric cancer patients. Because protons can be precisely controlled, pediatric proton therapy is ideal for tumors located near growing tissues in the spinal cord and brain, eyes, ears or mouth.
Children with tumors in the brain, head, neck, spinal cord, heart, lungs and other areas that are sensitive to radiation can benefit from treatment with proton therapy because physicians can target treatment directly to the tumor area. This limits the possible damage to children whose bodies are still developing.
Types of childhood cancer that may be treated with proton therapy include:
- Astrocytoma
- Brain tumors
- Choriocarcinoma
- Craniopharyngioma
- Ependymoma
- Ewing’s sarcoma
- Glioblastoma
- Glioma
- Intracranial germ cell tumors (germinoma)
- Optic pathway/hypothalamic glioma
- Medulloblastoma
- Meningioma
- Neuroblastoma
- Optic Nerve Tumors
- Retinoblastoma
- Primitive neuro-ectodermal tumor (PNET)
- Rhabdomyosarcoma
- Osteosarcoma
- Teratoma
Leaders in research and treatment of childhood cancer
At the MD Anderson Proton Therapy Center, we are world leaders in the research and treatment of childhood cancer with proton therapy, an advanced form of radiation precisely targets tumors while sparing surrounding healthy tissue.
Our pediatric team includes physicians, nurses, radiation therapists and other cancer experts that specializes in treating children with cancer. From its inception, the MD Anderson Proton Therapy Center was designed with children and their families in mind – from our child-friendly waiting and play areas to our special, early appointment times for many of our young patients.
We're here for you
If your child’s type of tumor is not listed, please contact the Proton Therapy Center for more information. Because the center is part of one of the nation’s top cancer centers, we treat more types of cancer in children with proton therapy than any other center.
Our multidisciplinary team of pediatric cancer experts evaluates each individual child’s specific type of cancer and recommends the best course of treatment.
Pediatric cancer parents: Why we traveled from Denmark for proton therapy at MD Anderson
When our son Lue was about 18 months old, we noticed he was sweating a lot. He was a happy toddler with no other visible symptoms. But when we had him checked by a doctor in Denmark, a lab test showed his blood counts were off. An ultrasound revealed neuroblastoma in his stomach and spine.
Traveling to Houston for proton therapy
In 2015, Lue started chemotherapy followed by surgery in Denmark. At the time, there were no proton treatment facilities available for children in Denmark, and proton therapy is the optimal radiation therapy treatment for pediatric patients. Because protons can be precisely controlled, pediatric proton therapy is ideal for tumors located near growing healthy tissues in the spinal cord, brain, eyes, ears or mouth.
So when the doctors in Denmark offered us the opportunity for Lue to receive treatment at MD Anderson, we made the trip to Houston. While Lue received proton therapy, he continued his chemotherapy.
We were fortunate to stay in Houston with other Danish families who also had children undergoing cancer treatment. It was encouraging to share our journey with them, and we remain in touch with some of the families.
Lue received a lot of love and care from Leo Flores and Yvette Rosenthal, the pediatric nurses at MD Anderson Proton Therapy Center. They took care of Lue as he underwent anesthesia for proton therapy. Their support and encouragement helped us get through each day.
Family bonding through a childhood cancer diagnosis
When we traveled to Houston, we brought along Lue’s two older brothers. It was tough for us to be away from home at such a crucial time. But it strengthened us as a family. Having his brothers there helped Lue get through each day of treatment. We found comfort in spending time together every day and facing Lue’s diagnosis as a family.
There was a guestbook in the lobby that we read often. A former patient wrote a reminder to not walk like a sheep but to walk and fight like a tiger. We took this to heart and reminded ourselves that we wanted to hold on to hope and fight like the tiger. A former patient at the Proton Therapy Center gave us bracelets with the slogan: “Never ever give up.” We wore those bracelets as a daily reminder for years after Lue’s treatment.
After Lue finished proton therapy, we returned home to Denmark. He had follow-up visits from his doctors in Denmark every three months, then yearly until he was in remission.
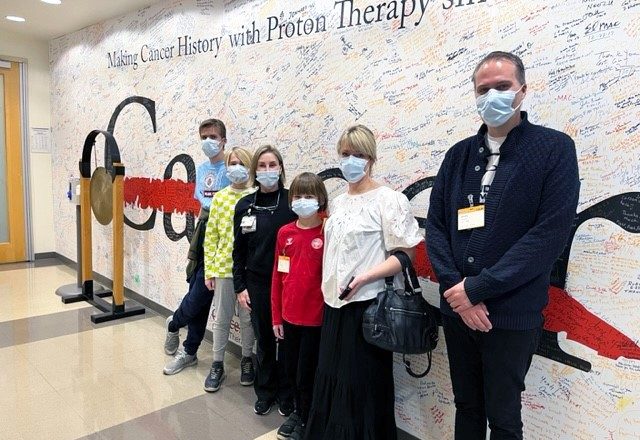
Return to MD Anderson provides perspective
Because Lue was so young when he underwent treatment in Houston, we wanted to give him memories he could remember. So in February 2023, we returned to Houston to let him tour MD Anderson. It was amazing to see the gong at the Proton Therapy Center that Lue hit after he completed treatment. We also got to reconnect with some of his care team. It was an emotional experience for all of us. It was important to us for Lue and his brothers to make new memories of visiting the zoo and parks in Houston as we had done so many times in 2015.
On one of the walking trails in Hermann Park, we saw a quote that put our experience into perspective. It said: “If you think in terms of a year, plant a seed. If you think in terms of 10 years, plant trees. If you think in terms of 100 years, teach the people.” It reminded us that when we were in Houston in 2015, we did not know what the future would have in store for us in just one year. All we could do was address the here and now and “plant a seed.”
Returning years later with our son in complete remission, we could see how our time had changed.
Today Lue is a healthy 9-year-old boy. He goes to school and loves playing soccer, reading, and spending time with his brothers. He has no side effects from the neuroblastoma or its treatment. He is in complete remission and sees his doctors in Denmark every year.
We are thankful for our time at MD Anderson and know it has shaped our son's path to never giving up.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.

How proton therapy helped my son with a childhood brain tumor
My son Benjamin was born weighing only 3 pounds. He stayed in the NICU for seven months. It was challenging and financially draining. We had a kindergartener and toddler at home, while also visiting Benjamin at the hospital every day.
When Benjamin was able to come home, he had a total parenteral nutrition (TPN) central line, an ostomy bag and a gastrostomy tube (G-tube) to receive nutrition.
By the time he was 1, he was able to eat and have the ostomy bag and G-tube removed. Life was beginning to feel normal.
At 2 years old, he jumped into a foam pit at a birthday party and came out holding his head to the side. When I asked if he felt hurt, he said no. I waited a few days thinking he had pulled a muscle in his neck. But the head tilt remained.
When I took him to his pediatrician, they sent us to physical therapy. After two weeks, nothing had improved. We saw a neurologist who said he seemed happy and healthy with no other symptoms other than a head tilt. The neurologist ordered an MRI to be safe, but I remember her telling me that she did not think they would find anything.
Before we left the hospital parking lot, I received a call saying the MRI results were in.
A childhood brain tumor diagnosis
That is when Benjamin was diagnosed with a type of brain tumor called a Grade 1 pilocytic astrocytoma. His oncologist at our local hospital recommended he start chemotherapy but suggested waiting on radiation therapy to give his body and brain time to grow so they could access the tumor better.
A few months later, tests showed the tumor had grown. His care team decided to operate. Benjamin had just turned 3 years old when he underwent brain surgery. He then had two weeks of inpatient rehabilitation. This was rough on our family because we had two little girls at home.
After six years of trying several types of chemotherapy, including two clinical trials, we were ready to try radiation therapy. I knew the tumor was still growing and Benjamin was having symptoms such as sleepiness and increased face paralysis. So, we decided to take a leap of faith, trust God and go to MD Anderson to have his tumor treated with proton beam therapy.
Proton therapy is an advanced type of radiation treatment that uses a beam of protons to deliver radiation directly to the tumor, destroying cancer cells while sparing healthy tissues. As a result, it minimizes side effects to prevent long-term complications. Because of the physical properties of proton beams, it is ideal for pediatric cancer patients with tumors located near growing tissues, especially in the brain, spine, eyes, ears or mouth.
Perseverance through proton therapy treatment
In Sept. 2022, when Benjamin was 10 years old, he started proton therapy at MD Anderson under the care of Dr. David Grosshans. He had a wonderful experience at MD Anderson Proton Therapy Center. Benjamin told me it was the easiest treatment he has been through. He bonded with his care team and loved taking naps during treatment. On Nov. 4, he celebrated his last treatment by ringing the gong.
During treatments, he did not have side effects. But after he completed proton therapy, he experienced some numbness on the left side of his body and weakness in his leg. He continues to go to physical therapy and that helps improve his strength.
Benjamin is doing well, and the tumor is stable. He is working hard to get caught up at school. Missing school for treatment affected his learning the most.
My advice to other parents is to bring a book and a snack to treatment. Keep a watchful eye on the patient and most of all, remember to take it one day at a time.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Pediatric brain tumor parent: We're grateful for MD Anderson
When Ben Gadot’s brain tumor symptoms began in 2013, he was just 3 months old. The first sign was a visual change in his eyes.
“It was as if he was always looking down,” says Cecilia Gadot, Ben’s mom. “We could see mostly just the white part of his eyes.”
ER trip reveals childhood brain tumor
When Cecilia and her husband, Raphael, took Ben to their pediatrician, they were referred to an ophthalmologist. But Ben's health quickly started to decline. Cecilia remembers him being very fussy, crying and vomiting. They took him to a local emergency room.
A CT scan revealed a childhood brain tumor called pilomyxoid astrocytoma. Ben’s diagnosis was a Grade 2 optic pathway glioma.
Ben started chemotherapy to slow the growth of the tumor at a nearby hospital.
In 2016, he underwent tumor debulking surgery to remove as much of the tumor as possible. The tumor impaired Ben’s vision, and he started to experience precocious puberty at age 3.
In April 2021, Ben’s care team considered treating him with proton therapy but decided to keep him on chemotherapy to slow the tumor’s growth. In July 2022, Ben underwent a ventriculoperitoneal shunt surgery. By draining extra fluid in his brain, the shunt would help control pressure there.
Brain tumor growth leads to proton therapy treatments
But that September, an MRI showed a slight progression of the tumor. Ben’s care team decided it was time to start proton therapy at MD Anderson under the care of radiation oncologist David Grosshans, M.D., Ph.D. Because protons can be precisely controlled, pediatric proton beam radiation is ideal for tumors near growing healthy tissues.
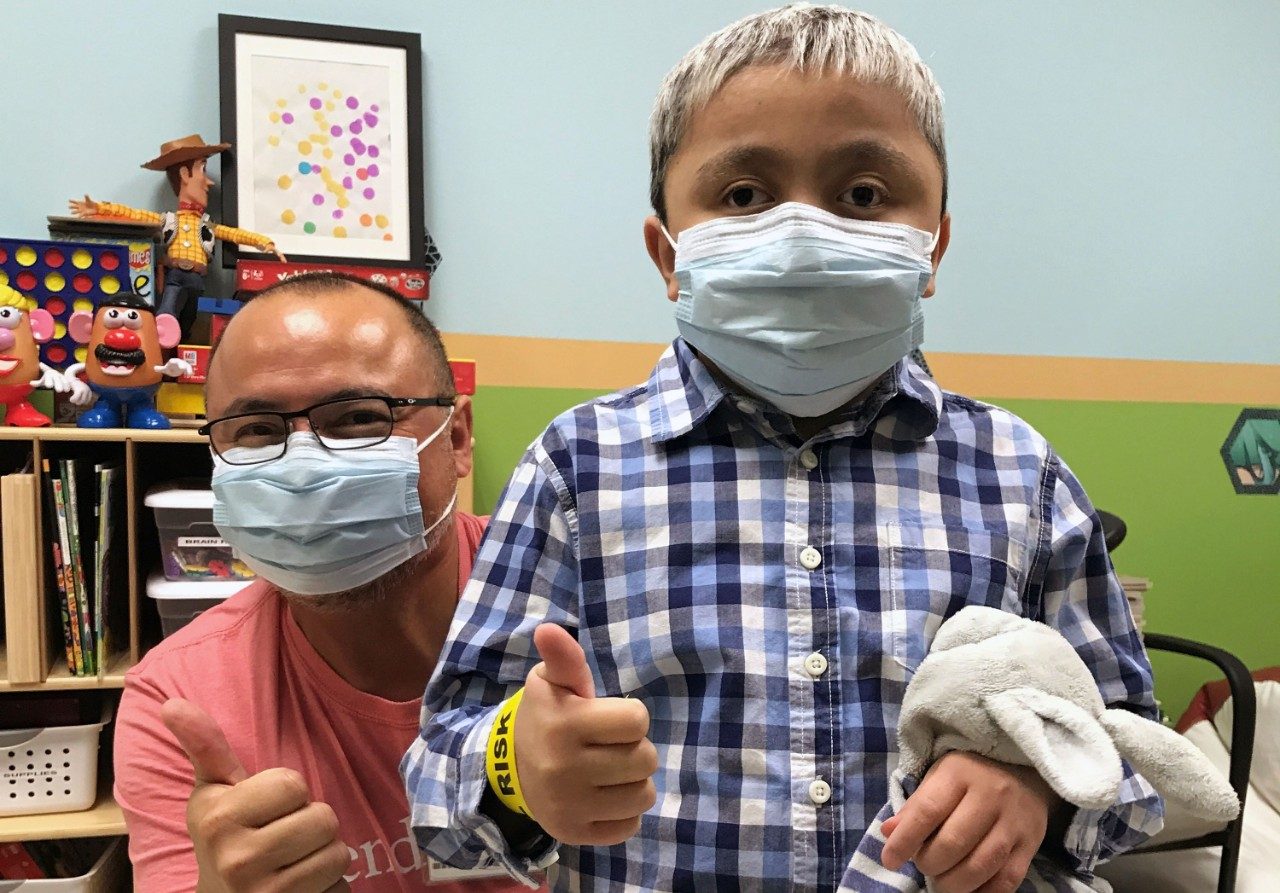
On Oct. 17, 2022, Ben started 28 days of proton therapy. With his positive attitude and the help of the child life team, he underwent treatments and MRIs without sedation. “The bond he had with his care team brought him a lot of trust and comfort,” says Cecilia.
Ben enjoyed playtime with child life assistant Leon Benavides in the playroom at the Proton Therapy Center before and after treatment.
“MD Anderson’s staff is very supportive and caring, from the front desk to the nurses, doctors, radiation therapists and, most importantly, child life specialists,” says Cecilia. “Ben’s time in the playroom with Mr. Leon was his daily reward and incentive.”
Finding gratitude with a child in cancer treatment
Cecilia encourages other parents of pediatric cancer patients to find something to be grateful for each day. “The hardest part of treatment is waiting for it to start. Once it starts, it goes pretty smoothly and quickly,” she says. “So, take time to make each day a good day.”
Ben’s appointments were scheduled early in the morning so he could continue his daily routine. Most days he was able to go to school.
On Nov. 23, 2022, a few days before Thanksgiving, Ben rang the gong with his family and care team cheering him on. “We are so grateful for MD Anderson for not only being the best place to receive proton therapy but for making Ben feel comfortable and cared for along the way.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Benefits of proton therapy for children
Most tumors in children are treated with surgery, chemotherapy and radiation therapy. While traditional radiation therapy with X-ray beams can be effective, it also can produce documented long-term side effects in some children, such as a decrease in bone and soft tissue growth in the treated area, hormonal deficiencies, intellectual impairment, including neuro-cognitive deficits, and secondary cancers later in life.
The ability to precisely target tumors makes proton therapy ideal for treating pediatric cancer. It provides accurate treatment of tumors near or within sensitive organs while limiting radiation exposure to healthy tissues, which is vital in children whose bodies are still growing and developing. This may reduce side effects during treatment, often allowing children to better tolerate proton therapy. Additionally, studies show that proton therapy can also result in fewer late effects from treatment, a major concern among physicians and families when a child – especially a very young child – is undergoing radiation treatment. This includes potentially fewer issues with brain development for children who have been treated for brain tumors.
Though treatment can vary for each patient’s specific case, most children are treated daily, Monday through Friday, for five to six weeks. Treatment can take anywhere from 30 minutes to 1 ½ hours daily, depending on whether the child is sedated.
Watch this video for more information on proton therapy for childhood cancer
Pencil beam proton therapy
MD Anderson pioneered pencil beam scanning proton therapy, also called spot scanning, and has extended its benefits to children with cancer.
Pencil beam proton therapy is an even more precise form of proton therapy treatment; it can be directed to move throughout the tumor’s depth to "paint" the treatment volume with spots of radiation, conforming to the shape of the tumor and delivering thousands of spots of radiation in just a few minutes. This can provide even greater benefits to young patients with brain or other types of tumors, especially those that are oddly shaped or within or near critical structures or vital organs in the body.
MD Anderson Proton Therapy Center is the only center in North America and one of three in the world to use pencil beam scanning proton therapy to treat both pediatric and adult patients.
Dedicated pediatric team
At MD Anderson Proton Therapy Center, we have a dedicated pediatric team that includes radiation oncologists, nurses, therapists, social workers, a child life specialist and other cancer specialists – all experts in treating children with cancer.
We also have a dedicated pediatric anesthesia team to provide anesthesia to very young children who may require daily sedation to help them remain still for their proton therapy treatment. MD Anderson Proton Therapy Center is one of the few proton therapy centers with a dedicated, on-site pediatric anesthesia team dedicated to caring for children. The specialized, experienced anesthesia support is essential for the safety and effectiveness of proton radiation delivery.
Watch this video of Shannon Popovich, M.D., explaining what parents can expect with daily anesthetic treatments in an effort to ease any apprehensions and fears parents have about their children being put to sleep for proton therapy treatment.
Protocols for proton therapy

At MD Anderson Proton Therapy Center, we collaborate with all of the cooperative groups for pediatric cancer, including the Children’s Oncology Group (COG) and the Pediatric Brain Tumor Consortium. Our physicians worked with COG to refine proton radiation guidelines for the organization’s protocols.Proton therapy radiation is now an acceptable form of radiation treatment for nearly all COG clinical trials that call for radiation therapy.
The Pediatric Proton Consortium Registry (PPCR) was established in 2012 to expedite proton outcomes research to assure access to those pediatric patients who can benefit the most from it. It is the most comprehensive multi-institutional radiation based patient registry in existence and unique in its scope and depth.
Registry for Pediatric Patients Treated With Proton Radiation Therapy
NCT01696721 - In previous studies, Proton Beam Radiation Therapy (PBRT) has been found to show better results in treating patients with cancer, both because there is better control of where in the body the radiation is directed and because it is associated with less severe long term side effects. However, there is limited published data demonstrating these results. The goal of the Pediatric Proton Consortium Registry (PPCR) is to enroll children treated with proton radiation in the United States in order to describe the population that currently receives protons and better evaluate its benefits over other therapies. The data collected from this study will help facilitate research on proton beam radiation therapy and allow for collaborative research. The PPCR will collect demographic and clinical data that many centers that deliver proton radiation therapy already collect in routine operations.
For more information, please contact:
Nancy Philip, MD Anderson Clinical Studies Coordinator
Tel: 713-563-9322
Expertise and convenience in a family-friendly setting
Because we are a part of MD Anderson Cancer Center, which has ranked as one of the nation’s top two cancer centers in U.S. News & World Report’s annual “Best Hospitals” survey for the past 25 years, our pediatric patients and their families have access to all of the resources of an internationally respected academic medical center within reach, including the Children’s Cancer Hospital at MD Anderson.
As part of the world-renowned Texas Medical Center, we have the greatest capacity for treating young patients from other major hospitals, both in our community and from around the world.
We also offer convenient, free surface lot parking at the center to help ease the burden of daily parking charges on families during treatment.

How proton therapy spared my baby of paralysis
"Always remember that treatment will end, and life does get better."

Choosing targeted radiation therapy at MD Anderson
"Communication with your child during treatment is key," says Ewing’s sarcoma caregiver Christine Pena.

Rhabdomyosarcoma cancer survivor Sawyer Hack
“Proton therapy was able to target the tumor in Sawyer’s jaw and save sensitive tissue such as his eyes and ears.”
Share Your Story
Tell us how you are confronting cancer.
Your story may provide support to others who are facing cancer.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Proton Therapy Glossary
Understanding commonly used proton therapy terms can help you prepare for treatment.
request an appointment online.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
