request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Ewing Sarcoma
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsEwing sarcomas, or Ewing tumors, are rare cancers that develop in the bones or soft tissues around bones. They most often begin in the pelvis, chest or legs—especially in the long bones such as the thighbone or shinbone. In rare cases, tumors can grow in the skull or the flat bones of the trunk.
Ewing sarcomas, or Ewing tumors, are rare cancers that develop in the bones or soft tissues around bones. They most often begin in the pelvis, chest or legs—especially in the long bones such as the thighbone or shinbone. In rare cases, tumors can grow in the skull or the flat bones of the trunk.
Ewing sarcomas account for about 1% of all childhood cancers. In the United States, the American Cancer Society estimates that about 200 children and teens are diagnosed with Ewing sarcoma each year. While it most often affects teenagers, it can also occur in younger children, young adults and even older adults. In fact, about 40% of cases are diagnosed in adults.
These tumors are caused by genetic changes that occur after birth, but they are not inherited and do not run in families.
Types of Ewing sarcomas
There are two main types of Ewing sarcoma. Although they look slightly different, they share the same genetic changes and are treated in similar ways.
- Ewing sarcoma of the bone: The most common type, starting in the bones themselves.
- Extraosseous Ewing tumor (EOE): A tumor that develops in soft tissues near bones.
Symptoms of Ewing sarcomas
Symptoms can vary depending on the location and size of the tumor. They may include:
- Pain at the tumor site, often worse with activity or at night
- Swelling, redness or warmth in the affected area
- Limping or difficulty walking if the tumor is in the leg
- A lump or mass that may be felt under the skin
- Fever or night sweats
- Unexplained weight loss
- Fatigue
- Bone fractures with little or no injury
Because these symptoms can overlap with sports injuries, infections or other conditions, it is important to see a doctor for a proper diagnosis.
Learn more about Ewing sarcoma symptoms.
Treatment for Ewing sarcomas
Treatment for Ewing sarcomas usually involves a combination of therapies designed to remove the cancer and prevent it from coming back. Options may include:
- Chemotherapy: This is usually the first step in treatment. It is used to shrink the tumor and kill cancer cells, and it is often given again after surgery.
- Surgery: The goal of surgery is to remove the tumor along with some of the surrounding healthy tissue. Doctors aim to remove all of the cancer while preserving as much normal function as possible.
- Radiation therapy: Radiation may be used when surgery is not possible or would cause too much loss of function. Sometimes, it is also combined with surgery to destroy any cancer cells that remain.
- Targeted therapy and clinical trials: For some patients, newer treatments may be available through clinical research studies.
Learn more about treatments for Ewing sarcoma.
Survival rates for Ewing sarcomas
Ewing sarcoma survival depends largely on the extent of disease at diagnosis. According to the American Cancer Society, patients with localized tumors, confined to one area, have the best outcomes, with a five-year relative survival of about 81%. Those with regional spread to nearby tissues or lymph nodes generally have slightly lower survival, around 77%, while prognosis is poorest for patients with metastatic or advanced disease, where cancer has spread to distant sites such as the lungs or other bones, with five-year survival around 41%.
Other factors influencing outcomes include the patient’s age, tumor size and location, and how well the cancer responds to initial treatment.
Risk factors for Ewing sarcoma
Although the exact cause of Ewing sarcoma is not known, researchers have identified certain factors linked to increased risk:
- Age: Ewing sarcoma is most common in teenagers.
- Gender: The disease occurs slightly more often in males than in females.
- Race: The risk is higher in white people, both non-Hispanic and Hispanic.
- Genetic changes: Ewing sarcomas are caused by specific chromosomal changes in cells. These changes occur after birth and are not inherited.
Ewing sarcomas are not passed down from parents to children. Families concerned about cancer risk may consider speaking with a genetic counselor for guidance.
Learn more about Ewing sarcomas:
Learn more about clinical trials for Ewing sarcoma.
MD Anderson is #1 in Cancer Care
Why choose MD Anderson for Ewing sarcoma care?
At MD Anderson's Children's Cancer Hospital, each child with Ewing sarcoma has a team of highly specialized experts who customize your child's treatment to ensure the most effective therapy with the least impact on the body – now and in the future.
Ewing's sarcoma is rare, and many doctors have little experience with treating it. Our physicians are among the world's most highly trained and experienced in treating Ewing sarcoma. This can translate into a better outcome in many cases.
Diagnosis and treatment
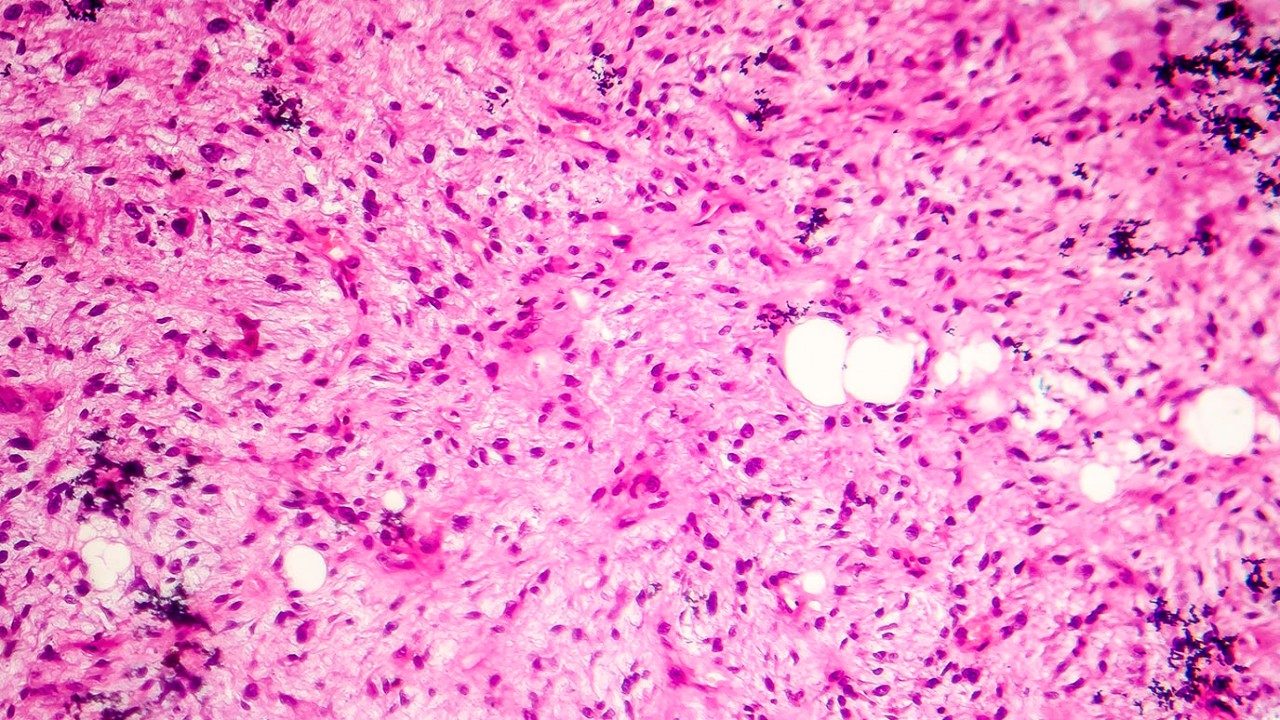
Accurate diagnosis of Ewing sarcoma can be challenging, but it is essential to successful treatment. Our pathologists are dedicated to sarcoma, and they use the latest, most-sophisticated tests to pinpoint the type and extent of the cancer.
Ewing sarcoma often requires a multi-therapy approach. Using the latest advances in complex limb-sparing surgeries, our surgeons are often able to avoid amputation if the cancer is in an arm or leg. If amputation is needed, we offer specialized rehabilitation.
Advancing research
Many children with Ewing sarcoma are treated with clinical trials. We participate in trials of the Children's Oncology Group and offer other innovative therapies available at only a few hospitals in the nation. Our researchers have helped make many advances, including using drug combinations to treat Ewing sarcoma.
Our Osteosarcoma and Ewing's Sarcoma Center coordinates care and streamlines and speeds access to clinical trials. In addition, sarcoma researchers work with physicians to translate laboratory research into new clinical trials, which are especially beneficial for patients with relapsed or refractorysarcoma.
Comprehensive care
Children's Cancer Hospital is designed just for children, with a full range of services and amenities that help make the child and family's experience as comfortable as possible. We go beyond medical care to deliver a comprehensive experience that treats the whole child. And at Children's Cancer Hospital, you're surrounded by the strength of one of the nation's top cancer centers.
If your child has been diagnosed with Ewing sarcoma, we're here to help. Call 877-632-6789 to make an appointment or request an appointment online.
I can body surf, bike and hike and still enjoy those things. On stage, I can still play music and jam with my friends. It’s awesome.
Matt Alcantara
Survivor
Newest research in sarcoma
Sarcomas are a broad group of cancers that originate from connective tissues, such as the blood or lymph vessels, gastrointestinal tract, fat tissue, tendons, smooth muscles and tissue around the joints. These tumors are broadly divided into bone sarcomas and soft tissue sarcomas. With more than 70 subtypes of sarcoma, there are also a wide variety of treatment approaches and prognoses, and everything about the disease, from diagnosis onward, is complex.
“If we look back over the last decade, we’ve made some tremendous improvements,” says Anthony Conley, M.D., associate professor of Sarcoma Medical Oncology. “However, there is still more we can do to improve therapeutics for sarcoma.”
Conley and his colleagues will present some of these new approaches at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting.
A virus to help the immune system attack tumors
Conley’s oral presentation (Abstract 2506) is about the results of a multicenter clinical trial using a genetically modified adenovirus combined with an immune checkpoint inhibitor to treat sarcoma, along with several other cancer types, that didn’t respond to immunotherapy alone. “There needs to be something else to invigorate the immune system to help fight the cancer,” he says.
Adenoviruses cause the common cold, but this one, called AdAPT-001, is genetically modified to help cause inflammation in the cancerous tumor, which then attracts the immune system to attack. It also changes the environment around the tumor to make it more responsive to immunotherapy. “It does that by introducing what is called TGF-β trap,” Conley says. “The virus has been engineered to soak up different forms of TGF-β. This then allows your T-cells, which are an important part of the immune system, to now activate, recruit other cells and damage the tumors.”
Side effects from AdAPT-001 were generally mild.
Conley and his team found that injecting AdAPT-001 directly into one or more tumors and also giving the patient an immune checkpoint inhibitor had a clinical benefit rate of 62.5% at 12 weeks. “It was a small study, but we found some really interesting results,” he says. “For example, in several cutaneous sarcomas treated with the combination therapy, the tumors visually looked better in scans — smaller and less irregular.” Furthermore, tumors that were not directly injected were improving as well.
In patients treated previously with immune checkpoint inhibitors, the combination treatment with AdAPT-001 allowed them once again to see a response.
An earlier part of this study was among the presentations related to sarcoma at last year’s ASCO annual meeting.
Risk stratifying sarcoma patients
Ryan Denu M.D., Ph.D., a second-year medical oncology fellow who was recognized with both the Conquer Cancer Merit Award and the 2024 ASCO Young Investigator Award, will present research (Abstract 11511) he completed under the supervision of Elise Nassif Haddad, M.D., Ph.D., assistant professor of Sarcoma Medical Oncology. “He took a gene he was interested in studying in the lab, ATRX, and wanted to find out what it could tell us about treatment or even about prognosis in a variety of soft tissue sarcomas,” Conley says.
The ATRX gene is involved with chromatin remodeling and acts as a regulator of transcription, meaning the process of creating an RNA copy of a DNA sequence. Denu’s research indicates that a number of different sarcomas have a loss of ATRX gene expression and function. “We think this may be essential to the development of the cancer and may also have prognostic value,” Conley says.
Denu correlated the presence of the ATRX gene and the protein it codes for with different aspects of the immune system. It seems that without the gene, the tumor is better able to avoid contact with the immune system and protect itself from the body’s defenses. Therefore, loss of ATRX is associated with both a distinct type of microenvironment — one that suppresses the immune system around the tumor — and worse overall survival.
“This has important implications for us as a way to potentially determine which patients might benefit from certain types of immunotherapy,” Conley says. “If this is validated in further studies, it might be something that we will routinely test for in a clinical setting.”
Potential for a blood test to predict outcomes
Richard Gorlick, M.D., division head of Pediatrics and interim department chair of Sarcoma Medical Oncology, was the middle author of research (Abstract 10018) about patients with metastatic Ewing sarcoma that were treated in the Children’s Oncology Group trial. Although Ewing sarcoma is commonly thought of as a disease affecting children, adolescents and young adults can also be diagnosed. The research found an association between increased levels of circulating tumor DNA (ctDNA) in the bloodstream following one cycle of chemotherapy and inferior outcomes.
“It might lead to people getting routine blood tests to look for ctDNA levels while they are being treated for Ewing sarcoma,” Conley says.
Gorlick, recipient of the ASCO 2024 Pediatric Oncology Award, will also be a discussant on the sarcoma oral abstract session as ASCO.
Poster presentations also highlight sarcoma research
J. Andrew Livingston, M.D., associate professor of Sarcoma Medical Oncology and both an adult medical oncologist and a pediatrician, is presenting a “trials in progress” poster (Abstract TPS11586) about a T cell membrane-anchored tumor-targeted IL12 (ATTIL12) -T cell therapy for sarcoma. “It is a cool and innovative study,” Conley says. “MD Anderson is the only place in the world that has this technology, which was developed by the pediatric oncology group.”
Alicia Gingrich, M.D., a complex general surgical oncology fellow, will be presenting a poster (Abstract 11546) about the immune microenvironment of leiomyosarcomas, which are smooth muscle sarcomas. Under the direction of Nassif Haddad, she looked at tissue samples of leiomyosarcomas under a microscope to find common characteristics and try to determine which patients need to be considered for immunotherapy and which immunotherapy treatments would be best for them. “This is great work that will hopefully lead to clinicians being better able to tailor treatments to the individual patients,” Conley says.
What’s next in sarcoma research
Sarcoma research at MD Anderson goes beyond these presentations at ASCO.
For example, Dejka Araujo, M.D., professor of Sarcoma Medical Oncology, and her colleagues recently published findings in The Lancet of a clinical trial of the first T cell therapy for patients with metastatic or unresectable synovial sarcoma or myxoid round cell liposarcoma. These patients had few options if the standard treatment of high-dose chemotherapy didn’t work. With the T-cell receptor therapy, many had durable responses, meaning their cancer responded to the treatment for at least six months and possibly longer, as the follow-up of these patients is still ongoing.
In addition, new research led by Christina Roland, M.D., associate professor of Surgical Oncology and Neeta Somaiah, M.D., associate professor of Sarcoma Medical Oncology, has found that immunotherapy before surgery leads to promising long-term survival in sarcoma patients.
“Our department has moved toward participating in multi-center clinical trials and leading clinical trials,” Conley says. “We are also very interested in incorporating immunotherapy into our treatments for sarcomas or even replacing some of the therapies we once used to treat these diseases. It’s an exciting time.”
Learn about research careers at MD Anderson.
Treatment at MD Anderson
Clinical Trials
MD Anderson patients have access to Ewing sarcoma clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.