News and Media
New advances in our understanding of cancer metabolism
Metabolism is the process by which the cells in your body use nutrients from the food you eat to get the energy you need.
When we talk about cancer metabolism, we’re talking about the process in which cancer cells make the energy they need to grow and spread. For nearly a century, cancer researchers have been working to develop a deeper understanding of cancer metabolism in hopes that it could lead to better treatment and prevention techniques.
In 2025, several MD Anderson research teams helped push cancer metabolism from a biochemical curiosity to a central framework for understanding, and potentially treating, metastatic disease. Two recent publications illustrate how metabolic rewiring shapes tumor aggression, how organs function and what therapeutic opportunities may lie ahead.
1. Sugary Drinks and Colorectal Cancer Metastasis — A Metabolic Mechanism With Real-World Impact (Nature Metabolism, Jihye Yun Lab)
What do sugar-sweetened beverages do to cancer cells? A group led by Jihye Yun, Ph.D., assistant professor, Genetics, uncovered a surprisingly potent metabolic driver of metastasis, or how cancer spreads.
Their study, published in Nature Metabolism, demonstrates that a glucose–fructose mixture, mimicking common sugary drinks, reprograms colorectal cancer metabolism as sugar breaks down. This shift increases the ratio of energy production to energy consumption at the cellular level and funnels carbon into the cholesterol biosynthesis pathway, which promotes cell migration and the start of metastasis.
Highlights of this work:
- It provides a mechanistic explanation for how dietary sugar can enhance the potential for metastasis.
- It shows that two parts of how cells process energy — the breakdown of sugar, and the pathway the body uses to create cholesterol, known as cholesterol biosynthesis — can be targeted to change cell metabolism.
- It raises the intriguing possibility that statins, common cholesterol-lowering prescription drugs, may dampen this metastasis-promoting circuit.
Takeaway: Diet is not just about your lifestyle. It is a metabolic input that can modulate metastasis through rewired biochemical pathways.
2. Fatty Acid Metabolism as a Driver of Bone Metastasis — ACBP as a Key Regulator (Science Translational Medicine, Li Ma Lab)
The second highlight comes from Li Ma, Ph.D., professor, Experimental Radiation Oncology, who uncovered a metabolic determinant of bone metastasis that goes far beyond glycolysis, the process of converting sugar to energy.
Their translational medicine study shows that ACBP, a specific protein that binds to acyl-CoA, a form of fatty acid, supports the spread of cancer to bone by tuning fatty-acid oxidation (FAO) and protecting tumor cells from ferroptosis, an iron-dependent form of cell death. Tumor cells that rely on this ACBP-FAO axis gain a survival advantage in the lipid-rich, high-stress bone microenvironment.
Highlights of this work:
- It places lipid metabolism, the process of breaking down fats for energy, at the center of metastatic biology.
- It suggests fatty-acid oxidation inhibitors or ferroptosis-sensitizing strategies as therapeutic avenues for bone metastatic disease.
- It strengthens a broader theme: metastatic cells survive by re-wiring metabolic stress responses.
Takeaway: Bone metastasis is not just about niche interactions; it is powered by a lipid-metabolic adaptation that can be targeted.
Across these studies, a unifying concept emerges: Metastasis is a metabolic state. Tumor cells that spread must reshape their nutrient use, redox balance, and stress-survival pathways. Those adaptations expose new intervention points.
Whether it is sugary beverages driving pro-metastatic fluctuation via SORD, or lipid metabolism sustaining bone-tropic cancer cells through ACBP, these papers highlight how understanding cancer metabolism is reshaping both prevention and therapy.
Eyal Gottlieb, Ph.D., is vice president of Research at MD Anderson.

RNA thought to spread cancer shows ability to suppress breast cancer metastasis
Researchers at The University of Texas MD Anderson Cancer Center have discovered that a form of RNA called metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) appears to suppress breast cancer metastasis in mice, suggesting a potential new area of therapeutic investigation. The findings, published in the Oct. 22 online issue of Nature Genetics, were surprising given that MALAT1, a long non-coding RNA (lncRNA), previously was described as a metastasis promoter.
“Our six-year study unearthed the unexpected metastasis-suppressing function of MALAT1 through highly rigorous genetics approaches,” said Li Ma, Ph.D., associate professor of Experimental Radiation Oncology and principal investigator for the study. “Our findings defy the conclusions drawn from previous MALAT1 studies and suggest the potential value of therapeutic agents targeting a cellular pathway linked to MALAT1. However, this will require further clinical investigation.”
Halting a key protein behind metastasis
Ma’s team observed that MALAT1 sequestered and inactivated a protein known as TEAD, a transcription factor, which when combined with a “co-activator” called YAP, causes cancer proliferation and metastatic progression. The researchers discovered that MALAT1 binds and inactivates TEAD, preventing it from partnering with YAP and targeting genes in promoting metastasis.
Although MALAT1 had been associated with metastasis, the team, using a breast cancer transgenic mouse model, inactivated the MALAT1 gene without altering expression of its adjacent genes and observed that MALAT1 inactivation promoted lung metastasis, which was reversed when MALAT1 was re-introduced.
Similarly, knockout of MALAT1 in human breast cancer cells induced their metastatic ability, which was reversed by the re-introduction of MALAT1. Additionally, overexpression of MALAT1 suppressed breast cancer metastasis in several mouse models.
“Taken together, our study reveals the unexpected function of MALAT1 through comprehensive gene targeting and genetic rescue approaches in multiple in vivo models,” said Ma. “These findings call for a reassessment of ongoing efforts to target MALAT1 as an anti-metastatic therapeutic strategy, and provide a general framework for pursuing a better understanding of lncRNAs.”
MD Anderson study team members included: Jongchan Kim, Ph.D., Hai-Long Piao, Ph.D., Fan Yao, Ph.D., Zhenna Xiao, Ashley Siverly, Sarah Lawhon, Baochau Ton, Hyemin Lee, Ph.D., Zhicheng Zhou, Ph.D., and Boyi Gan, Ph.D., all of the Department of Experimental Radiation Oncology; Mien-Chie Hung, Ph.D., Zhenbo Han, M.D., Ph.D., and Yutong Sun, Ph.D., of the Department of Molecular and Cellular Oncology; Yumeng Wang, Ph.D., and Han Liang, Ph.D., of the Department of Bioinformatics and Computational Biology; and M. James You, M.D., Ph.D., of the Department of Hematopathology.
Other participating institutions included: Dalian Institute of Chemical Physics, Dalian, China; Baylor College of Medicine, Houston; Hokkaido University, Sapporo, Japan; and China Medical University, Taichung, Taiwan.
MD Anderson Research Highlights for January 12, 2022
The University of Texas MD Anderson Cancer Center’s Research Highlights provides a glimpse into recently published studies in basic, translational and clinical cancer research from MD Anderson experts. Current advances include an anti-CD19 chimeric antigen receptor (CAR) T cell therapy to treat follicular lymphoma, targeted therapies for urothelial cancers and advanced breast cancers, understanding the tumor microenvironment and immune landscape in pancreatic cancer, a link between depression risk and androgen deprivation for prostate cancer, and the discovery of new therapeutic targets for Alzheimer’s disease, liver cancer and aggressive breast cancer.
Tisagenlecleucel safe and effective against relapsed and refractory follicular lymphoma
While follicular lymphoma (FL), a type of non-Hodgkin lymphoma, is usually slow-growing, most patients relapse, and it is rarely curable. A research team led by Nathan Fowler, M.D., examined the use of tisagenlecleucel — an autologous anti-CD19 chimeric antigen receptor (CAR) T cell therapy — to treat patients with relapsed or refractory FL who had already undergone two or more treatment lines or had an autologous stem cell transplant. In an interim analysis of 94 patients treated on the Phase II international ELARA trial, the complete response rate was 69% and the overall response rate was 86%. The therapy was well tolerated by the majority of patients, with mild to moderate cytokine release syndrome, immune effector cell-associated neurotoxicity syndrome (ICANS) and neurological events, and no treatment-related deaths . These results suggest that tisagenlecleucel is a safe and effective option for treating patients with relapsed or refractory FL, including patients who have high-risk or advanced disease characteristics. Learn more in Nature Medicine.
Erdafitinib shows consistent results in follow-up of patients with urothelial cancer and FGFR mutations
Mutations in fibroblast growth factor receptor (FGFR) are present in approximately 15 to 20% of patients with metastatic bladder cancer and up to 35% of patients with other urothelial cancers of the renal pelvis or ureter. In the primary analysis, published in 2019, research led by Arlene Siefker-Radtke, M.D., showed that the FGFR inhibitor erdafitinib was effective after median 11 months follow-up. Those results led to approval of erdafitinib by the Food and Drug Administration, making it the first oral targeted therapy approved for advanced bladder cancer. In this final analysis, with a median follow-up of 24 months, the objective response rate was 40%. Responses lasted for a median of six months, while 31% of responses lasted for at least one year. Treatment benefit with erdafitinib was observed in patients regardless of previous chemotherapy or immunotherapy, and there were no new safety signals. Erdafitinib is currently being studied in other treatment settings. Learn more in Lancet Oncology.
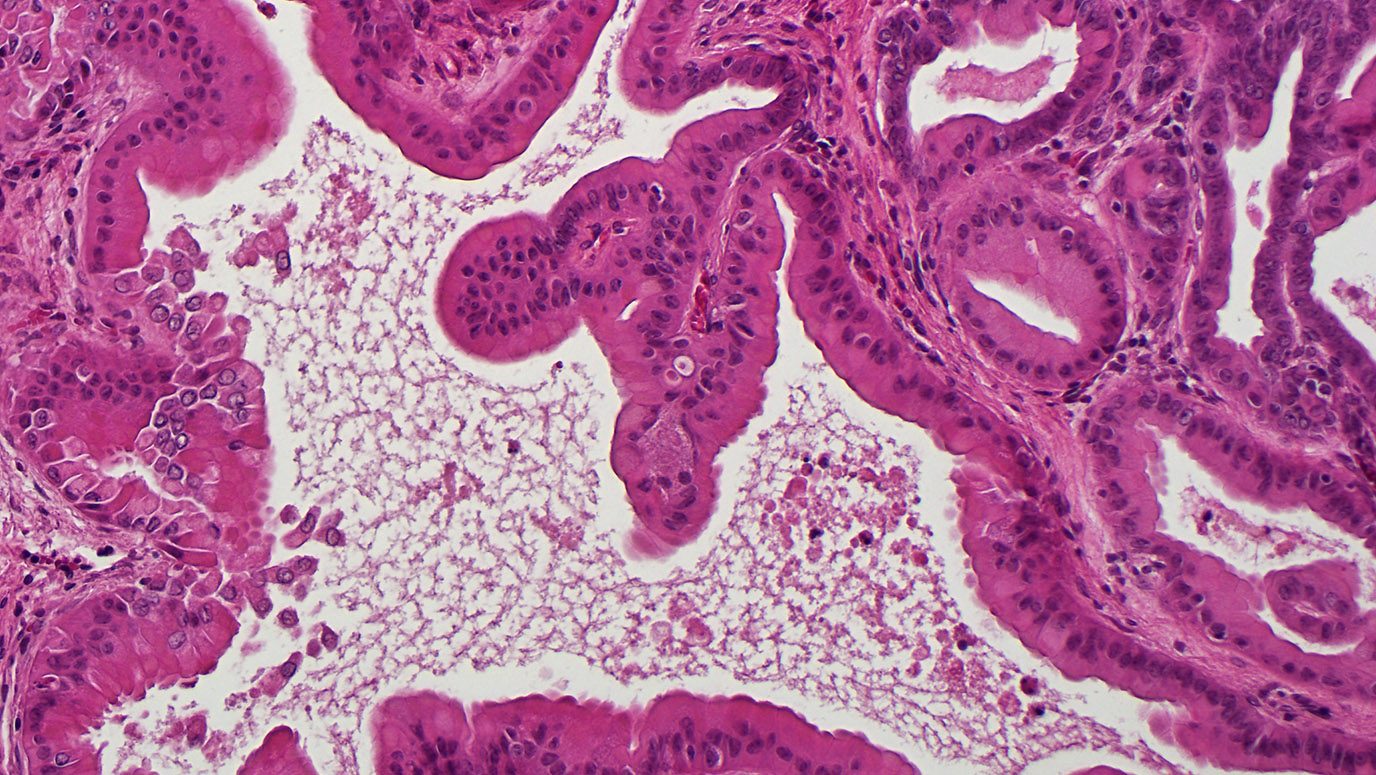
RNF43 mutations accelerate KRAS-driven pancreatic cancer, stimulate immune microenvironment remodeling
Roughly 5-10% of all pancreatic cancers have loss-of-function mutations in the ring finger protein 43 (RNF43) gene, and this is one of the most commonly mutated genes in pancreatic pre-cancerous cysts. Unfortunately, no effective targeted therapies are available to treat patients with RNF43 mutations. Using a genetically engineered mouse model, researchers led by Abdel Nasser Hosein, M.D., Sonja Woermann, M.D., and Anirban Maitra, M.B.B.S., studied RNF43 in the context of mutant KRAS. They discovered that RNF43 acts as a tumor suppressor and its deletion cooperates with mutant KRAS to accelerate the development pre-cancerous lesions and pancreatic cancers. Additionally, RNF43 loss resulted in a distinct tumor immune microenvironment marked by increased numbers of anti-tumor lymphocytes and fewer suppressive myeloid cells, suggesting these tumors may be susceptible to immune checkpoint inhibitors. The immune signaling protein CXCL5 was decreased in RNF43-deficient tumors, pointing to a possible target to mediate the unique immune landscape in these cancers. Learn more in Gastroenterology.
Telomerase gene TERT identified as a novel therapeutic target for Alzheimer’s disease
Dysfunction in telomeres — the protective caps at the ends of chromosomes — can cause premature aging and neurodegeneration. The telomerase reverse transcriptase (TERT) gene is critical for maintaining telomeres. In a new study, researchers led by Hong Seok Shim, Ph.D., Y. Alan Wang, Ph.D., and Ronald A. DePinho, M.D., demonstrated that, independent of its role in telomere synthesis, TERT plays a key role in regulating gene networks central to the development of Alzheimer’s disease (AD). They discovered that epigenetic TERT repression is an early molecular event occurring before the development of AD. Experimental maintenance of physiological levels of TERT in mouse models and in neurons from AD patients alleviated toxic amyloid-β accumulation and blocked cognitive decline. Mechanistically, the researchers showed TERT interacts with β-catenin transcription complex to regulate genes governing neuron survival, amyloid clearance, learning and memory. The findings suggest that activating TERT therapeutically could be a novel strategy to slow or prevent AD progression. Learn more in Nature Aging.
Study identifies new therapeutic target to stimulate ferroptosis in liver cancer
Available systemic therapies for advanced hepatocellular carcinoma (HCC) provide only limited benefit, but evidence suggests that targeting ferroptosis — an iron-dependent form of controlled cell death — may have therapeutic potential. The liver cancer treatment sorafenib can stimulate ferroptosis, but many cancer cells are resistant. In a new study, researchers led by Fan Yao, Ph.D., Yalan Deng, Ph.D., and Li Ma, Ph.D., identified leukemia inhibitory factor receptor (LIFR) as a novel tumor suppressor and regulator of ferroptosis in HCC. Using genetically engineered mouse models and HCC patient-derived xenografts (PDXs), the researchers demonstrated that loss of LIFR activates the NF-kB signaling pathway to elevate levels of the iron-sequestering cytokine LCN2, leading to iron depletion and resistance to sorafenib-induced ferroptosis. In preclinical studies, an LCN2-neutralizing antibody enhanced sorafenib’s ability to induce ferroptosis and eliminate cancer cells in PDX tumors with low LIFR and high LCN2 levels. The findings suggest that anti-LCN2 therapy should be further explored to target ferroptosis and improve liver cancer treatment. Learn more in Nature Communications.
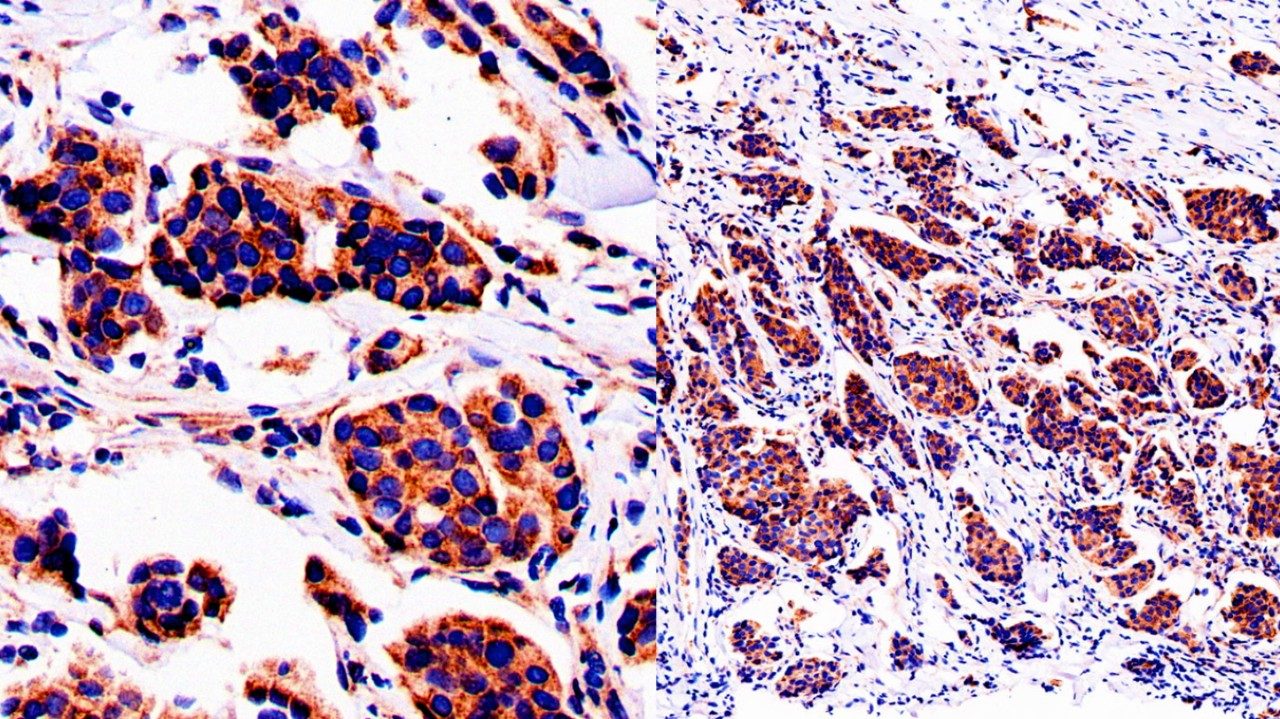
NDRG1 promotes brain metastasis in aggressive breast cancers
Up to 30% of patients with advanced breast cancer may develop brain metastases, which have limited treatment options and are associated with poorer outcomes. The stress response protein N-myc downstream regulated gene 1 (NDRG1) has a controversial role in metastasis, as it appears to block metastasis in certain cancer types while promoting it in others. Researchers led by Emilly Villodre, Ph.D., and Bisrat Debeb, D.V.M., Ph.D., discovered that NDRG1 drives tumor progression and brain metastasis in aggressive breast cancers. In laboratory models, cancer cells with high levels of NDRG1 were associated with a higher prevalence of brain metastases, greater tumor burden and reduced survival. In patient samples, high NDRG1 was associated with aggressiveness and served as an independent predictor of poor survival outcome. Blocking NDRG1 in preclinical studies slowed tumor growth and inhibited brain metastasis, suggesting this may be a novel therapeutic target for aggressive breast cancers. Learn more in the Journal of the National Cancer Institute.
Ribociclib and hormone therapy continue to demonstrate survival advantage in premenopausal advanced breast cancer patients
Breast cancers in younger women are known to be more aggressive and typically have a poorer prognosis. In the only trial of its kind dedicated to premenopausal women, the Phase III MONALEESA-7 trial led by Debu Tripathy, M.D., evaluated the CDK4/6 inhibitor, ribociclib, plus hormone therapy versus placebo plus hormone therapy for advanced hormone receptor-positive (HR+) breast cancer. Initial results published in 2019 were the first to show an overall survival benefit with a CDK inhibitor, which was reported at 42 months of follow-up. This analysis at a median follow-up of 53.5 months revealed a median overall survival of 58.7 months for patients receiving ribociclib compared to 48 months in patients receiving hormone therapy plus placebo. These results confirm the benefit of ribociclib and hormone therapy in the first-line setting and were consistent across multiple subsets in premenopausal HR+/human epithelial growth factor 2 negative (HER2-) advanced breast cancer. Learn more in Clinical Cancer Research.
Second-generation antiandrogens associated with depression risk in men with prostate cancer
Hormone therapy, including androgen deprivation therapy, is an established prostate cancer treatment. Most men advance to castration-resistant disease and are treated with second-generation anti-androgens, which work by blocking androgen production or the androgen receptor. Although prior studies showed an association between androgen deprivation therapy and depression, it is unknown if the increased potency of second-generation therapies would also increase the risk of depression. Kevin Nead, M.D., led a retrospective cohort study of 30,069 men and found a statistically significant twofold increase in depression among patients treated with second-generation antiandrogens compared with traditional forms of hormone therapy and no hormone therapy. These results suggest that additional research is needed to better understand the relationship between newer antiandrogens and the increased risk of depression. Learn more in JAMA Network Open.
In case you missed it
Read below to catch up on recent MD Anderson press releases across the spectrum of cancer research.
MD Anderson Research Highlights for December 6, 2021
The University of Texas MD Anderson Cancer Center’s Research Highlights provides a glimpse into recently published studies in basic, translational and clinical cancer research from MD Anderson experts. Clinical advances include positive data with targeted therapies for HER2 exon 20 mutant lung cancer, for older patients with mantle cell lymphoma and for BRAFV600E-mutant gliomas. Additional discoveries include insights into chromosomal instability and immunotherapy resistance in pancreatic cancer, the genomic landscape of small-cell lung cancer, hematopoietic stem cell decline with telomere shortening, identifying tumor suppressors in CRISPR screens, and physiological responses to fasting.
Multi-center study demonstrates clinical benefit for poziotinib in HER2 exon 20 mutant lung cancer
There is currently an unmet need for targeted therapies to treat the 2% to 5% of non-small cell lung cancers (NSCLC) with HER2 exon 20 oncogenic driver mutations. Cohort 2 of the Phase II ZENITH20 clinical trial assessed the small molecule inhibitor poziotinib in 90 patients with previously treated HER2 exon 20 mutant NSCLC. Xiuning Le, M.D., Ph.D., John Heymach, M.D., Ph.D., and colleagues reported an objective response rate of 27.8% after a median follow-up of nine months. Most patients (74%) saw their tumors shrink. The disease control rate was 70%, median progression-free survival was 5.5 months and median duration of response was 5.1 months. Thirteen percent of patients permanently discontinued treatment due to adverse events. The results echo the findings from a smaller, single-institution study previously published by MD Anderson researchers. Based on the results of this smaller study, the FDA granted fast-track designation to poziotinib in March 2021. Learn more in the Journal of Clinical Oncology.
Utilizing ibrutinib and rituximab combination as first-line “chemotherapy-free” treatment of older patients with mantle cell lymphoma
Patients with mantle cell lymphoma (MCL) are generally treated with systemic chemotherapy, although older patients tend to have poorer tolerance, quality of life and outcomes with chemotherapy. Since most MCL patients are older, alternative treatments are needed. A research study led by Preetesh Jain, M.D. Ph.D., and Michael Wang, M.D., investigated the safety and efficacy of a chemotherapy-free combination of ibrutinib and rituximab administered to 50 previously untreated older (≥ 65 years) patients with MCL. This single-institution single-arm Phase II trial treated patients with the combination for two years, then continued ibrutinib therapy alone. The overall response rate was 96%, and 71% of trial enrollees experienced a complete response. While 22% of patients experienced atrial fibrillation, the combination was found to be safe and no on-study deaths were noted. The combination of ibrutinib and rituximab is promising for MCL treatment, and the researchers suggest conducting a randomized trial to definitively prove its effectiveness. Learn more in the Journal of Clinical Oncology.
New combination therapy offers promising treatment for BRAFV600E-mutant gliomas
Standard treatments for gliomas — the most common primary brain tumors — consist of a combination of surgery, radiation and temozolomide-based or lomustine-based chemotherapy. However, because current options have been associated with poor response rates and prognoses, especially for patients with the BRAFV600E mutations, finding an effective treatment to improve outcomes remains an unmet clinical need. A team of researchers led by Vivek Subbiah, M.D., conducted the Phase II Rare Oncology Agnostic Research (ROAR) basket trial to assess the activity and safety of dabrafenib plus trametinib combination treatment in patients with BRAFV600E-mutated high-grade glioma (HGG) and low-grade glioma (LGG), as well as other rare cancers. In the glioma cohorts, the combination therapy demonstrated clinically meaningful activity — a 33% and 69% objective response rate in HGG and LGG, respectively — and was well tolerated, with a safety profile consistent with that in other indications. These findings suggest that BRAFV600E testing could potentially be adopted in clinical practice for patients with glioma. Learn more in The Lancet Oncology.
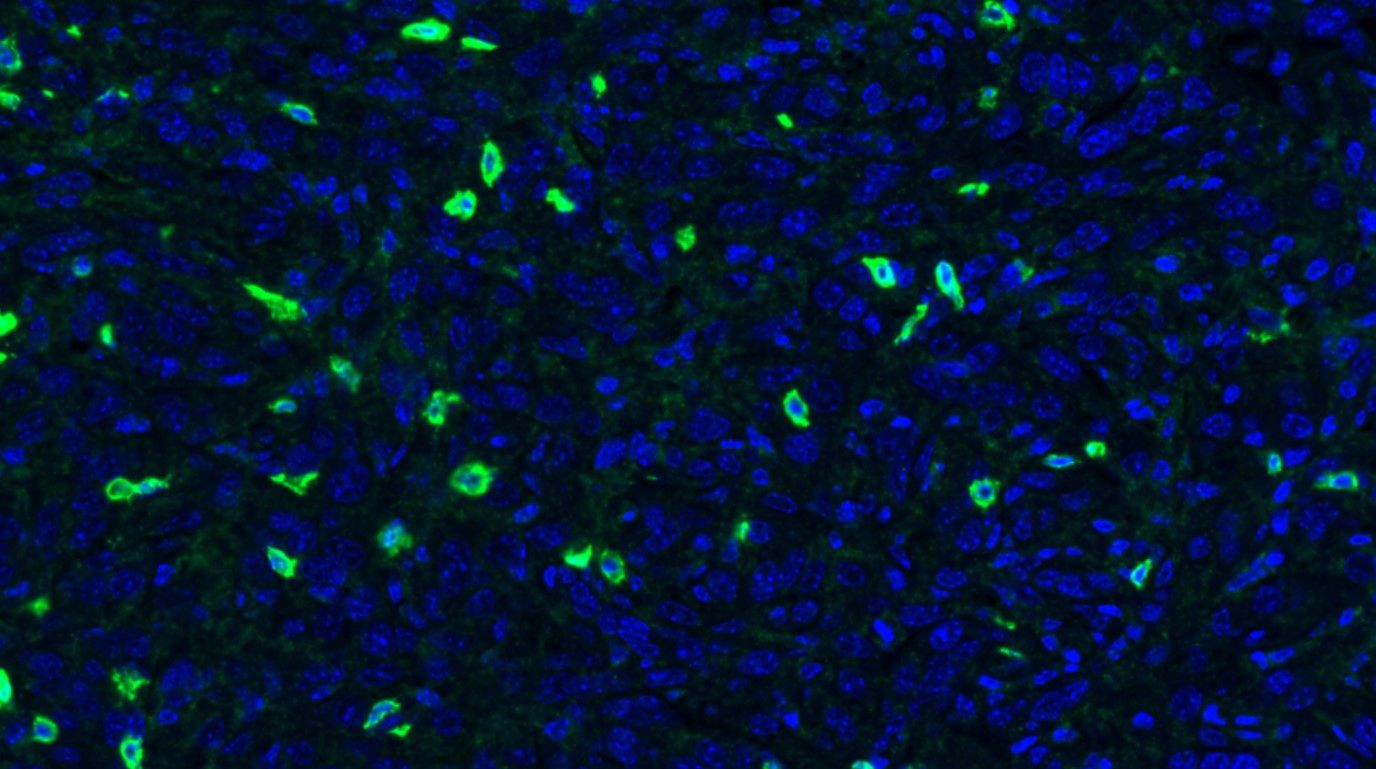
Glucocorticoid receptor in pancreatic cancer cells promotes immunotherapy resistance
Immune checkpoint inhibitors have not been effective in treating patients with pancreatic cancer, in part due to an immune-suppressive tumor microenvironment. Glucocorticoid signaling is thought to suppress immune cell activity, but new research led by Yalan Deng, Ph.D., and Li Ma, Ph.D., discovered an important role for the glucocorticoid receptor (GR) within pancreatic cancer cells. They demonstrated GR signaling in pancreatic cancer cell lines regulates expression of the immune checkpoint protein PD-L1 and the antigen presentation protein MHC-I. In preclinical models, either genetic depletion or therapeutic inhibition of GR lowered PD-L1 and elevated MHC-I levels, sensitizing otherwise immunotherapy-resistant pancreatic tumors to checkpoint inhibitors. High GR expression in pancreatic cancer patient samples correlated with high PD-L1 expression, low MHC-I expression and poorer clinical outcomes. The findings suggest that GR signaling plays an important role in cancer cells to suppress the anti-tumor immune response, pointing to a potential new therapeutic target. Learn more in Nature Communications.
Study provides new insights on genomic landscape of small-cell lung cancer
Small-cell lung cancer (SCLC) is an aggressive form of lung cancer with high rates of recurrence and early metastasis. Research has suggested that complex genomic intratumor heterogeneity contributes to treatment resistance. In this study, researchers applied whole-exome sequencing and T cell receptor sequencing to 50 samples from 19 limited-stage SCLC tumors to investigate the immunogenomic landscape and assess impact on patient survival. Jianjun Zhang, M.D., Ph.D., Lauren Averett Byers, M.D., and Alexandre Reuben, Ph.D., reported finding a homogeneous mutational landscape overall, but an extremely cold and heterogeneous T cell receptor repertoire, which was associated with higher chromosomal copy number aberration burden and lower overall survival. Learn more in Nature Communications.
Understanding hematopoietic stem cell decline in response to telomere shortening
DNA damage is a major cause of stem cell decline, and one precursor to persistent DNA damage is telomere erosion. Telomeres naturally shorten over time, but erosion can be accelerated by mutations in telomere maintenance genes. It is unclear how shortened telomeres lead to stem cell deg.traver_hartcline, but hematopoietic stem cells (HSCs) are particularly vulnerable to telomere-maintenance defects. Researchers led by Natthakan Thongon, Ph.D., and Simona Colla, Ph.D., sought to understand how shortened telomeres affect HSCs and lead to bone marrow failure syndromes. Using single-cell analysis, they discovered that shortened telomeres activate the innate immune response in HSCs, driving persistent metabolic activation and differentiation processes that limit their self-renewal capacity and lead to cell exhaustion. These processes were overcome by targeting the Ifi20x/IFI16 family of DNA sensors with an oligodeoxynucleotide comprised of telomeric repeats, suggesting that targeting the IFI16 signaling axis may prevent HSCs’ functional decline in the face of telomere shortening. Learn more in Nature Communications.
Harnessing CRISPR genetic screens to identify new tumor suppressors
Genetic screens using CRISPR gene editing allow researchers to efficiently inactivate individual genes to determine effects on cancer cell survival. Most screens look for cell death to identify genes essential for growth, but screens also can point to tumor suppressor genes when knockouts cause increased proliferation. Using more than 1,000 published screens, researchers led by W. Frank Lenoir, Ph.D., and Traver Hart, Ph.D., demonstrated a novel approach to identify potential tumor suppressors. Through this technique, they identified a network of 145 suppressor genes across 22 functional groups. The researchers discovered and validated that components of the fatty acid metabolism act as tumor suppressors in a subset of acute myeloid leukemia (AML) cells, and expression of those genes was correlated with patient survival outcomes. The study provides not only a new technique for identifying tumor suppressors, but also points to a potential prognostic marker and therapeutic target for AML. Learn more in Nature Communications.
A new understanding of how fasting protects against therapy toxicity
Normal tissue toxicity is a major limitation in delivering effective doses of chemotherapy and radiation. Preclinical studies from the laboratory of Helen Piwnica-Worms, Ph.D., showed fasting can blunt the effects of high-dose chemotherapy and — in collaboration with the laboratory of Cullen Taniguchi, M.D., Ph.D. — radiation in part by protecting intestinal stem cells, but the mechanism remains unclear. A new study led by Christopher Terranova, Ph.D., Kristina Stemler, Ph.D., Kunal Rai, Ph.D., and Piwnica-Worms discovered that fasting leads to epigenetic modifications in small intestinal crypt cells that activate specific metabolic pathways. During fasting, the major metabolite produced by the body is β-hydroxybutyrate (β-OHB), which the researchers demonstrated can directly modify histone proteins to trigger the expression of metabolic genes in the small intestine. This mechanistic understanding may help researchers develop approaches to protect against side effects without needing to fast, possibly expanding the therapeutic window of chemotherapy and radiation. Learn more in Cell Reports.
In case you missed it
Read below to catch up on recent MD Anderson press releases across the spectrum of cancer research.
Give Now
Research Areas
Find out about the four types of research taking place at UT MD Anderson.