request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Childhood Acute Lymphocytic Leukemia
- Childhood Acute Lymphocytic Leukemia Treatment
Childhood Acute Lymphocytic Leukemia Treatment
At MD Anderson's Children's Cancer Hospital, we know your child's health and well-being are your number one concern. Our renowned experts customize your child's care for leukemia utilizing the most advanced treatments and techniques with the least impact on your child's growing body. As part of one of the world's most active cancer centers, the Children's Cancer Hospital has remarkable experience and skill in these types of cancer. This can make a difference in your child's outcome.
Customized leukemia care plans
A team of specially trained physicians follows your child throughout treatment, all the way to survivorship. They communicate closely with each other, and with you, to ensure comprehensive, personalized care. They are supported by full complement of health care professionals dedicated to your child's treatment, including nurses, physician assistants, therapists and others.
The Children's Cancer Hospital offers clinical trials for innovative new treatments for leukemia. Behind the scenes, we are working on groundbreaking basic science research to change the future of pediatric cancer.
Treating the whole child
The Children's Cancer Hospital is designed just for children, with a full range of services and amenities that help make the child’s and family's experience as comfortable as possible. We go beyond medical care to deliver a comprehensive experience that treats the whole child, including camp programs, arts in medicine, music therapy and more.
And at the Children's Cancer Hospital, your child benefits from the resources and expertise of one of the nation's top cancer centers.
Acute lymphocytic leukemia (ALL) treatment plans
Newly diagnosed childhood ALL patients typically undergo chemotherapy, which is given in three phases. Depending on the features of the patient’s cancer, targeted therapy may also be prescribed.
If the cancer returns or does not respond to treatment, patients may undergo a stem cell transplant.
Young adult patients under age 25 may qualify for CAR T cell therapy if they have been treated unsuccessfully with other therapies.
Chemotherapy
Chemotherapy drugs kill cancer cells, control their growth or relieve disease-related symptoms. Chemotherapy may involve a single drug or a combination of two or more drugs, depending on the type of cancer and how fast it is growing.
Chemotherapy for ALL is usually given in multiple stages.
The first is induction. This is an intense phase of treatment designed to kill leukemia cells in the blood and bone marrow. It usually requires a hospital stay. The goal is to bring cancer into remission.
Following induction are three to four phases designed to kill any cancer cells that survived induction. These phases include consolidation, interim maintenance, delayed intensification and interim maintenance II.
Maintenance comes after these phases of therapy. In the maintenance phase, patients receive a lower dose of chemotherapy to stop the cancer from returning. ALL patients receive maintenance chemotherapy for about one and half years.
Patients may also be given a small dose of chemotherapy in their central nervous system through a lumbar puncture to prevent the disease from spreading to this area. Stem cell transplant patients also may undergo chemotherapy to prepare their body for the procedure.
Learn more about chemotherapy.
Targeted therapy
Targeted therapy drugs are designed to stop or slow the growth or spread of cancer. This happens on a cellular level. Cancer cells need specific molecules (often in the form of proteins) to survive, multiply and spread. These molecules are usually made by the genes that cause cancer, as well as the cells themselves. Targeted therapies are designed to interfere with, or target, these molecules or the cancer-causing genes that create them.
Learn more about targeted therapy.
Stem cell transplantation
A stem cell transplant (also known as a bone marrow transplant) is a procedure that replaces cancerous bone marrow with new, healthy bone marrow stem cells. Stem cell transplants are usually given after an intense round of chemotherapy that kills the patient’s existing bone marrow cells and prepares the body for transplant. Patients usually must stay in the hospital for three to four weeks after the procedure.
A stem cell transplant may be needed for patients whose leukemia has returned or has not responded to standard treatments. It may also be recommended if the patient has a high-risk form of leukemia that would make a cure with standard treatments unlikely. This treatment can be physically challenging, so it is typically not given to patients who are older or otherwise unhealthy.
Learn more about stem cell transplants.
Radiation therapy
Radiation therapy uses powerful beams of energy to kill cancer cells. Since leukemia cells travel in the blood stream, there is no distinct tumor to target with radiation therapy. Instead, radiation may be used when the disease has spread to the central nervous system.
Learn more about radiation therapy.
CAR T cell therapy
T cells are a type of immune system cell. They help the immune system respond to disease and directly kill diseased cells. In Chimeric Antigen Receptor (CAR) T cell therapy, T cells are modified so they can recognize and attack cancer cells.
Learn more about CAR T cell therapy.
Monoclonal antibody therapy
Monoclonal antibodies treatment is a type of immunotherapy. They attach to specific proteins on the surface of cancer cells or immune cells. They either mark the cancer as a target for the immune system, or boost the ability of immune cells to fight the cancer.
Learn more about immunotherapy.
Clinical trials
As a top-ranked cancer center, MD Anderson offers multiple clinical trials for ALL. Many of these cannot be found anywhere else. Trials explore new drug combinations and new drugs, including targeted therapies and immunotherapies.
Learn more about clinical trials.
Some cases of leukemia can be passed down from one generation to the next. Genetic counseling may be right for you. Learn more about the risk to you and your family on our genetic testing page.
Learn more about childhood acute lymphocytic leukemia (ALL):
Leukemia Treatment at MD Anderson
Childhood Acute Myeloid Leukemia is treated in our Children's Cancer Hospital.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.

CAR T cell therapy for pediatric patients: What parents should know
CAR T cell therapy is a type of immunotherapy that modifies T cells, so they can detect and fight cancer cells. This therapy is increasingly used to treat pediatric patients with B-cell acute lymphoblastic leukemia and, in rare cases, certain types of lymphoma.
But how is CAR T cell therapy for pediatric patients different from the treatment used for adult patients? And what are the side effects?
We spoke with registered nurse and lead pediatric stem cell transplant coordinator Sarah Featherston for answers to these questions and more. Here’s what she wants parents and caregivers to know.
How do you determine if a pediatric patient is a good candidate for CAR T cell therapy?
Currently, we have FDA-approved CAR T cells to treat relapsed and refractory patients up to age 25. These are patients whose cancer has come back or whose cancer has stopped responding to treatment.
They need to have a good performance status and the right expression, such as CD19, on the surface of cancer cells. CD19 is a marker of B cells and the target of CAR T cell therapy.
We often use CAR T cell therapy to get leukemia patients into remission, so that they can have a stem cell transplant.
Can you describe the process of CAR T cell therapy for pediatric patients?
The patient first gets a thorough workup that includes organ evaluations and testing to make sure they will be healthy enough to handle the collection process, chemotherapy and the CAR T infusion itself.
After that, the steps are as follows:
1. Cell collection
A pediatric surgeon will place a special catheter called an apheresis catheter in the patient. This is done while the child is under anesthesia. The same day, the patient undergoes cell collection in which T cells are extracted from the patient’s blood through the new catheter.
Aside from some minor discomfort where the new catheter is placed, pediatric patients generally tolerate the procedure very well. Since the catheter is only in for collection, it’s removed right after collection is complete, usually on the second day. Pediatric patients are put to sleep for catheter placement but not for removal, so they’re awake while they’re getting sutures removed and having pressure applied to that area. Naturally, they aren’t too happy about this, so with the help and expertise of our child life specialists, we talk patients through it and help put them at ease.
We work closely with the pediatric leukemia team for the best time to collect. In some cases, patients with leukemia may be taking steroids, and we try to avoid collecting while the patient is taking steroids.
2. Cell manufacturing
Our cell therapy lab freezes the cells before sending them to a specialized lab where they are genetically modified. Depending on the product, it takes about three weeks before they are sent back to the hospital.
3. Bridging therapy
When the T cells are being modified, patients will receive a small amount of chemotherapy to keep the leukemia at bay. This is called bridging therapy.
If we’ve treated the patient before, we know their treatment history pretty well. So, if a certain treatment wiped them out last time or caused the patient’s blood counts to drop extremely low, we may try something milder this time. We work closely with the pediatric leukemia team to keep the patient’s blood counts in a safe range while they’re receiving chemo.
4. Infusion
Once the modified cells arrive back at MD Anderson, the patient is given lympho-depleting chemotherapy. This means it will wipe out the lymphocytes to make room for the new CAR T cells and allow them to multiply. Then, the CAR T cells are infused into the patient’s blood. This process is quick, usually between 5 and 30 minutes. When this is an inpatient procedure, patients will spend about three weeks at the hospital before it’s safe for them to go home.
Adult CAR T patients can have their infusions done outpatient. Our goal is to offer infusion as an outpatient procedure in the future for pediatric patients as well.
5. Monitor for side effects
After the infusion, we monitor the patient for side effects. We perform several assessments to see how they’re functioning. One of the assessments is a neurological assessment called the Cornell Assessment of Pediatric Delirium (CAPD). It’s a series of questions, including ‘Is the patient making purposeful movements? Is the patient making eye contact? Is the patient expressing needs?’ We also do handwriting assessments, and if the patient is very young, we’ll have them draw pictures.
Once patients are discharged, they usually come in at least twice a week for follow-ups. We also do assessments then, and get the family involved. After all, they know the patient best. We continue assessments for eight weeks after infusion.
Once patients receive the CAR T cell infusion, we continue to follow them long-term. If there’s no disease relapse, they won’t necessarily see their leukemia or lymphoma doctor anymore. Patients will either proceed to bone marrow transplant, or they’ll be in long-term CAR T care, where we’ll watch their B cells and monitor their condition.
What are the side effects of CAR T cell therapy in pediatric patients? How do you manage them?
The two biggest side effects we see are cytokine release syndrome (CRS) and neurotoxicity, also known as Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS). CRS is common, and it almost always occurs first. CRS can cause flu-like symptoms like high fever and fatigue. This is due to the high cytokine levels produced by the T cells multiplying. Generally, we begin seeing these side effects about three days after the infusion, but they can also occur later.
ICANS is identified by different grades, according to the severity of neurological symptoms. The symptoms can range from mild confusion, like the patient saying things they don’t mean by using unintended syllables, to more severe symptoms, like seizures. ICANS can happen along with CRS, but it’s rarely the first side effect. Patients can develop ICANS with CRS or once the CRS resolves.
We usually start by giving the patient an IL-6 inhibitor like tocilizumab to manage CRS symptoms. If the symptoms don’t go away after two or three doses, or symptoms become more severe, we will use additional therapies, like steroids.
Assessments are one of our earliest indicators of neurotoxicity. If a patient writes the same sentence twice a day, we can see a big change in handwriting if they begin to develop neurotoxicity. MD Anderson closely monitors patients, which helps mitigate high levels of CRS and ICANS. We can treat side effects early without destroying the CAR T cells that we want circulating.
CAR T cell therapy targets the patient’s B cells – both cancerous and non-cancerous. This can cause an extremely low count of B cells, a condition known as B-cell aplasia. This is a good indicator that a patient still has CAR T cells circulating. Patients will continue to have their B cells monitored after infusion. We’ve had some patients who have lost their B cells 30 days after infusion; for others, it happens a few months out of treatment. B-cell aplasia is not a bad thing from our perspective. If a patient has it long-term, it’s almost like they’ve got little fighters against cancer continuously monitoring their body. When they start to recover their B cells, we worry that they’re losing their CAR T cells. Luckily, we can live without B cells. B-cell aplasia is not ideal, but it’s better than cancer.
What new research is being done to advance treatment of pediatric patients with CAR T cell therapy?
CAR T cell therapy is still a new treatment, which is available for relapsed and refractory patients. Clinical trials are being conducted to see if it’s beneficial to use them for upfront therapy so that pediatric patients can avoid intense chemotherapy.
Because we’re learning new things about CAR T cell therapy, it’s a viable treatment option for more patients and families. If your child needs it, they’ll be in good hands.
Request an appointment at MD Anderson online or call 1-877-632-6789.
What is minimal residual disease (MRD)?
After completing a course of treatment, there are few words that sound better to a patient than “complete remission.” It’s an indication that the treatment has worked, and there is no evidence of cancer based on scans or lab tests.
However, there is a different phrase that can be somewhat confusing to patients – minimal residual disease (MRD). This term is used often by physicians when treating patients with blood cancers, such as leukemia, lymphoma or multiple myeloma.
MRD refers to cancer cells remaining after treatment that can’t be detected by those same scans or tests. But what exactly does it mean for patients?
To learn more about minimal residual disease, we spoke with leukemia specialist Ghayas Issa, M.D., of MD Anderson’s Myelodysplastic Syndromes (MDS) and Acute Myeloid Leukemia (AML) Moon Shot® team. Here’s what he shared.
How do you explain minimal residual disease to patients?
Minimal residual disease is a small number of cancer cells left in the body after treatment. These cells have the potential to come back and cause relapse in our patients.
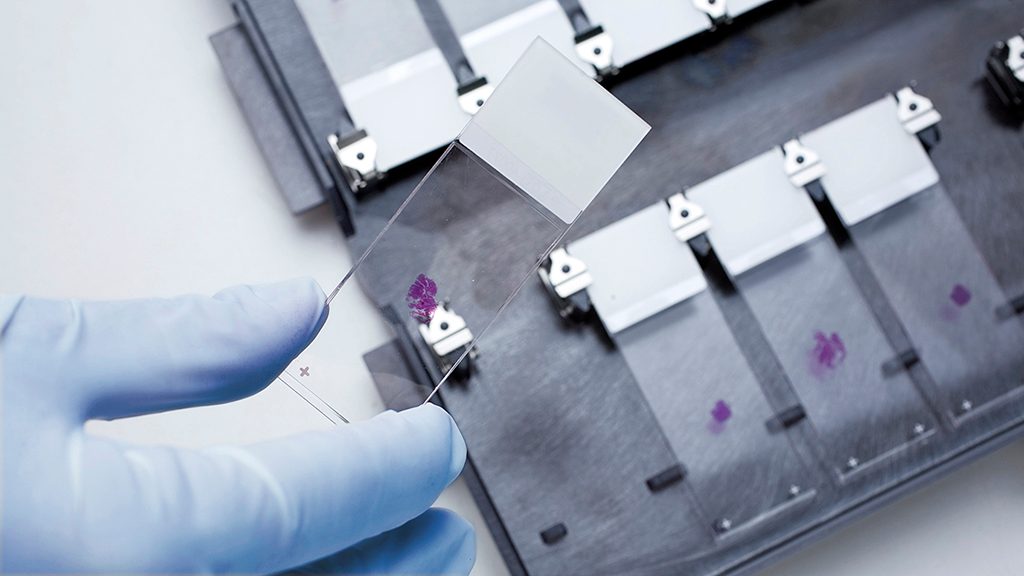
In leukemia, for example, we look for response after chemotherapy treatment by looking under the microscope for cancer cells present in a bone marrow biopsy. When there are no cancer cells present, and the bone marrow is making normal cells, we call that a complete response.
However, we know that if we don’t do further treatment, a portion of these patients will experience a relapse. That means there were some leukemia cells hiding that we weren’t able to detect under the microscope. That is minimal residual disease, or perhaps a better term is measurable residual disease. Typically, these cells don’t cause any symptoms, but they have the potential to lead to a relapse.
If we can’t detect minimal residual disease under the microscope, how do we test for it?
We now have much more sensitive assays available to us that allow us to quantify MRD. These could include next generation genetic sequencing, where we can analyze bone marrow samples for genetic mutations. If there are mutations present, that means there is minimal residual disease, even though we can’t see anything under the microscope.
We can also use a technique called flow cytometry, which allows us look in the same samples for abnormal proteins on the surface of cells. By determining how many cells have abnormal proteins detected, we can get a better sense of residual cancer cells. Using these new assays, we routinely try to quantify whether a patient has MRD following standard treatment.
What are the implications for a patient who has evidence of minimal residual disease after treatment?
That’s difficult to say, because it’s not the same across all types of blood cancers. Some patients with MRD will have different responses than others. In general, if a patient has MRD, we need to do additional treatments to work toward the best outcome. If we do nothing, we know that the residual cells will cause a relapse.
It also depends on the timing of the MRD test. In my leukemia patients, if there is MRD after the first cycle of chemotherapy treatment, it tells me that I probably need to give more treatment — either a different medication or a different course of treatment. If there is still MRD after many rounds of chemotherapy, that is an indication that the patient may need to have a stem cell transplant, when otherwise it might not have been appropriate.
Ultimately, MRD is a marker that we need to be more aggressive in our treatment to try and prevent the cells from coming back.
What can cancer researchers learn from the residual cancer cells?
We can learn a great deal. These cancers can adapt to treatment, meaning the cancer we start with is not the same as what we have after treatment. By studying the minimal residual disease, we can learn more about what is left after treatment.
That helps us to do several things. First, it allows us to modify our treatment, either by adding medications that target specific vulnerabilities in the cancer cells, including medications that are especially good at killing even residual cells, or doing a stem cell transplant, which is able to take care of residual cells.
Currently, I work with a wonderful team through the MDS and AML Moon Shot to study these residual cancer cells in order to find new vulnerabilities. Through our research, we’re hoping to identify new treatments that we can use in the future to specifically eliminate minimal residual disease.
Request an appointment at MD Anderson online or by calling 1-877-632-6789

Pediatric stem cell transplants: What to know
When chemotherapy alone isn’t successful in treating blood cancers like leukemia and lymphoma in pediatric patients, a stem cell transplant may be an option. They can also help treat some non-cancerous bone marrow diseases, like sickle cell disease, thalassemia, severe aplastic anemia and Kostmann syndrome.
To learn about pediatric stem cell transplants and what parents should know, we spoke with Priti Tewari, M.D.
What is a stem cell transplant?
Stem cells are produced in our bone marrow; they mature to become our red blood cells, white blood cells, platelets and the cells of our immune system.
Stem cell transplants replace damaged or defective stem cells with healthy cells. They can also help replace a weakened immune system. There are two types:
- Autologous stem cell transplants use a patient’s own stem cells to help fight cancers like high-risk Hodgkin lymphoma, Ewing’s sarcoma, medulloblastoma and neuroblastoma. These cancers may require high doses of chemotherapy. Autologous transplants use patients’ own healthy stem cells to help with recovery.
- Allogeneic transplants replace patients’ stem cells with healthy cells from a donor.
Are stem cells transplants safe for kids?
Stem cell transplants come with risks, but they can be an option for patients as young as only a couple months old.
With some non-cancerous diseases like severe combined immunodeficiency, the transplant should take place as soon as possible. Pediatric patients with this condition often have weaker immune systems and are at greater risk for infection.
With some inherited disorders, we may watch your child for a few years and allow the organs to mature a little bit before moving ahead with a stem cell transplant.
What are allogeneic stem cell donor options for pediatric patients?
Suitable donated stem cells should match your child’s cells. Siblings are sometimes -- but not always -- a match. If a sibling isn’t an option, we can look for a matched unrelated donor through the National Marrow Donor Program.
If we can’t find a matched donor, we can use an alternate donor. That could be a mismatched unrelated donor, an umbilical cord blood donation or a haploidentical donation, which is a half-matched family member like a parent or sometimes a sibling.
If you have a child with a condition that may require a stem cell transplant and you’re expecting a baby, it could be beneficial to preserve the baby’s umbilical cord in a process called umbilical cord blood banking. If the siblings’ cells are a match, the banked cord may be used for a transplant later.
How are donated stem cells extracted?
They’re extracted in two ways. With peripheral withdrawal, the donor receives growth factor shots to stimulate stem cell production. The cells are then removed intravenously by apheresis, a process like blood donation.
The second approach is called bone marrow harvesting. It removes the stem cells from the pelvic bone through a surgery; it requires general anesthesia.
We decide which approach is best based on the diagnosis, the donor’s physical size and the child’s overall health. If the donor is another child, we take special precautions. We want to ensure the donor is willingly entering this process. At MD Anderson, the donating child meets with a separate doctor on our team, a psychologist, our ethicist and a child life specialist to ensure they understand the procedure.
How do patients prepare for a stem cell transplant?
To wipe out cancer cells and to help make space for the new stem cells, patients receive chemotherapy before the transplant. Some high-risk acute lymphoblastic leukemia patients may also receive total body irradiation, a type of radiation therapy.
If your child is receiving an allogeneic transplant, we often use immunosuppressive agents to help lower the risk of a side effect called graft-versus-host disease, which is when the patient’s body rejects the donated cells.
What are the side effects of a pediatric stem cell transplant?
Many patients experience pancytopenia, which is a decrease in red blood cells, white blood cells and platelet counts.
The conditioning chemotherapy and radiation therapy commonly cause mucositis, which is irritation and ulcers throughout the digestive tract and mouth. Patients also can have painful sores, stomach discomfort and diarrhea, but medications can help.
Also, it’s rare, but the organs that help process chemotherapy -- such as the kidneys, liver and lungs -- are at risk for failure.
Another risk is infection. During and following a stem cell transplant, patients have no immune system to help fight infections. So, even a cold can be dangerous.
But we closely monitor patients to identify side effects before they become life-threatening. That’s one of the reasons why patients stay in the hospital for about four to six weeks, but sometimes it’s more. Our goal before your child leaves the hospital is for the new stem cells to start growing inside the body. We also want to get your child comfortable and walking, taking sips of water and sleeping comfortably until their blood counts are up again. Once they’re well enough to leave the hospital, they’ll start coming in for checkups three to five days a week.
Do stem cell transplants affect fertility?
Cancer and its treatment can affect fertility. Every patient who’s beyond puberty sees our fertility specialists to learn about their risks and options.
It’s also very important to discuss fertility with patients with non-cancerous diseases since these conditions are often hereditary. We want to make sure patients understand what that means for their future children and what options they have for starting a family.
What does life look like after a stem cell transplant?
If all goes well, life typically starts feeling normal about a year after the transplant.
During that year, we’re weaning down the immunosuppressive agents to help build up your child’s immune system. So, if they go back to a traditional school and they get a virus from somebody, their bodies can fight it.
If your child has siblings in school, they’ll be exposed to germs. It can be challenging, but it’s important for everyone to wash their hands and avoid sharing cups, utensils and food. It’s very important to avoid being around others with colds or the flu, too.
What research is underway in kids with blood diseases?
CAR T cell therapy is a new type of immunotherapy that’s given like a stem cell transplant. It’s being used to treat B-cell acute lymphoblastic leukemia and certain lymphomas in patients ages 25 and younger. But the side effects can be severe. MD Anderson has developed the first guidelines for managing these side effects in kids to help more patients receive CAR T cell therapy more safely.
What's your advice for families considering a stem cell transplant?
There's a lot to learn, and it can be overwhelming. Ask your care team for resources to learn more at your own pace.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention and Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
