Dr. Frederick Lang
Sections
Cranial
About the section
Our neurosurgeons perform more complex surgeries on brain tumor patients than any hospital in the nation. The Cranial section manages all brain tumor types including gliomas (glioblastomas, astrocytomas, oligodendrogliomas), intraventricular tumors, pineal region tumors, thalamic and brainstem region tumors, hemangioblastomas, ependymomas and meningiomas. Additionally, our neurosurgeons treat patients with brain metastases, who require advanced treatment approaches provided through a dedicated Brain Metastasis Clinic. Brain tumor treatment involves a multidisciplinary approach which includes surgery, radiation therapy, chemotherapy and targeted therapy. Our team uses cutting-edge technology, including Gamma Knife Radiosurgery, the iMRI Suite, laser interstitial thermal therapy (LITT), 5-ALA fluorescent technique to maximize tumor resections, specialized brain mapping including awake craniotomy and electrocorticography techniques carefully planned with patient's lifestyle in mind. All these interventions have resulted in superior oncological outcomes and improved survival for the patients. Our surgeons are also actively involved in recruiting patients to clinical trials to provide comprehensive surgical care that fits their specific tumor type and location.
Cranial cases by fiscal year
- 2020: 1,074
- 2021: 1,116
- 2022: 1,063
- 2023: 941
- 2024: 1,229
- 2025: 1,380
Faculty

Frederick Lang, M.D., FACS
Professor and Chairman
Director, Brain Tumor Center Executive Committee
Surgery for primary and metastatic brain tumors, surgery for insular brain tumors, surgery for tumors in eloquent brain regions, viral therapies for brain tumors

Ian E. McCutcheon, M.D., FRCS(C)
Professor
Surgery of pituitary neoplasms, spinal and brain tumors, neurofibromatosis, Gamma Knife Radiosurgery

Sherise D. Ferguson, M.D.
Associate Professor | Center Medical Director
Surgery for primary and metastatic brain tumors, Gamma Knife Radiosurgery

Christopher A. Alvarez-Breckenridge, M.D., Ph.D.
Assistant Professor
Surgery for primary and metastatic brain tumors, immunotherapy, Gamma Knife Radiosurgery

Robert North, M.D., Ph.D.
Assistant Professor
Surgery for primary and metastatic brain tumors, Gamma Knife Radiosurgery, laser interstitial thermal therapy

Jeffrey S. Weinberg, M.D.
Professor and Deputy Chairman
Vice Chair of Clinical Operations
Primary and metastatic brain tumors, pediatric brain tumors, computer-assisted surgery for biopsy and tumor resection, surgery for tumors in eloquent brain regions, Gamma Knife Radiosurgery

Sujit Prabhu, M.D., FRCS (Ed)
Professor
Surgery for primary and metastatic brain tumors, surgery for tumors in eloquent brain regions, brain mapping, laser interstitial thermal therapy, Gamma Knife Radiosurgery

Betty Kim, M.D., Ph.D.
Professor
Primary and metastatic brain tumors, nanomedicine and immunotherapy for brain tumors, Gamma Knife Radiosurgery

Chibawanye I. Ene, M.D., Ph.D.
Assistant Professor
Surgery for primary and metastatic brain tumors in eloquent brain regions, Laser interstitial thermal therapy, Gamma Knife Radiosurgery, viral and macrophage therapies for brain tumors.
Featured publication

Noll KR, Asman A, Tasnim I, Hall M, Connelly K, Swamy C, Ene C, Tummala S, Grasu RM, Liu HL, Kumar VA, Muir M, Prinsloo S, Michener H, Wefel JS, Ince NF, Prabhu SS. Intraoperative language mapping guided by real time visualization of gamma band modulation electrocorticograms: Case report and proof of concept.
Brain mapping techniques are used to reduce the risk of cognitive and linguistic deficits that may be acquired during surgery to resect brain tumors. Preoperatively, task-based functional MRI (fMRI) either alone or in combination with transcranial magnetic stimulation (TMS) have been used to identify eloquent language sites. Awake craniotomy with intraoperative direct cortical stimulation (DCS) is considered the gold standard to identify eloquent brain regions. While fMRI alone has modest correlation with DCS, this correlation is improved when fMRI is used in combination with TMS. Electrocorticography (ECoG) however records neuronal activity from electrodes placed directly on the surface of the brain.
In this case study, we evaluated task-based intraoperative ECoG for language mapping by visualizing gamma band electrocorticograms during administration of diverse language tasks in the intraoperative setting. We also compared ECoG recordings with disruption of function during DCS. The patient in this case study presented with migraines and episodic impairment in spelling and reading. Imaging revealed a large non-enhancing mass in the posterior left temporo-occipital area, which was determined by biopsy and pathology to be a WHO grade II IDH-mutant astrocytoma. Preoperative task-based language mapping was performed using fMRI and intraoperative mapping was performed using a dual iPad stimulus presentation system with Object, Action, Auditory and Written naming tasks.
The patient was under general anesthesia until the dura was opened and a 32-channel ECoG grid was placed covering most of the left temporal cortex. The patient was awakened and intraoperative mapping was performed using a Neuromapper coupled to a portable real-time neural signal processing system capable of recording both ECoG cortical activity and delivering DCS in a closed loop. ECoG recordings and real time visualization data were collected first, followed by DCS, during administration of language tasks. Good correlation was observed between ECoG and DCS for Object and Action naming tasks for electrodes located in the anterior to mid-superior temporal gyrus representing language networks. During resection, the patient was monitored with conversation and periodic naming tasks; speech became more variable as the resection proceeded deeper into the brain. A subtotal (85% of the tumor) resection was achieved, and pathology indicated a WHO grade IV IDH-mutant astrocytoma. While these findings are preliminary, our work demonstrates the potential utility of ECoG gamma band data acquisition and processing in the mapping of language functions and suggests further studies examining its use may be warranted.
Related Media
Dr. Jeffrey Weinberg
Awake Craniotomy
Dr. Sujit Prabhu
Featured Case
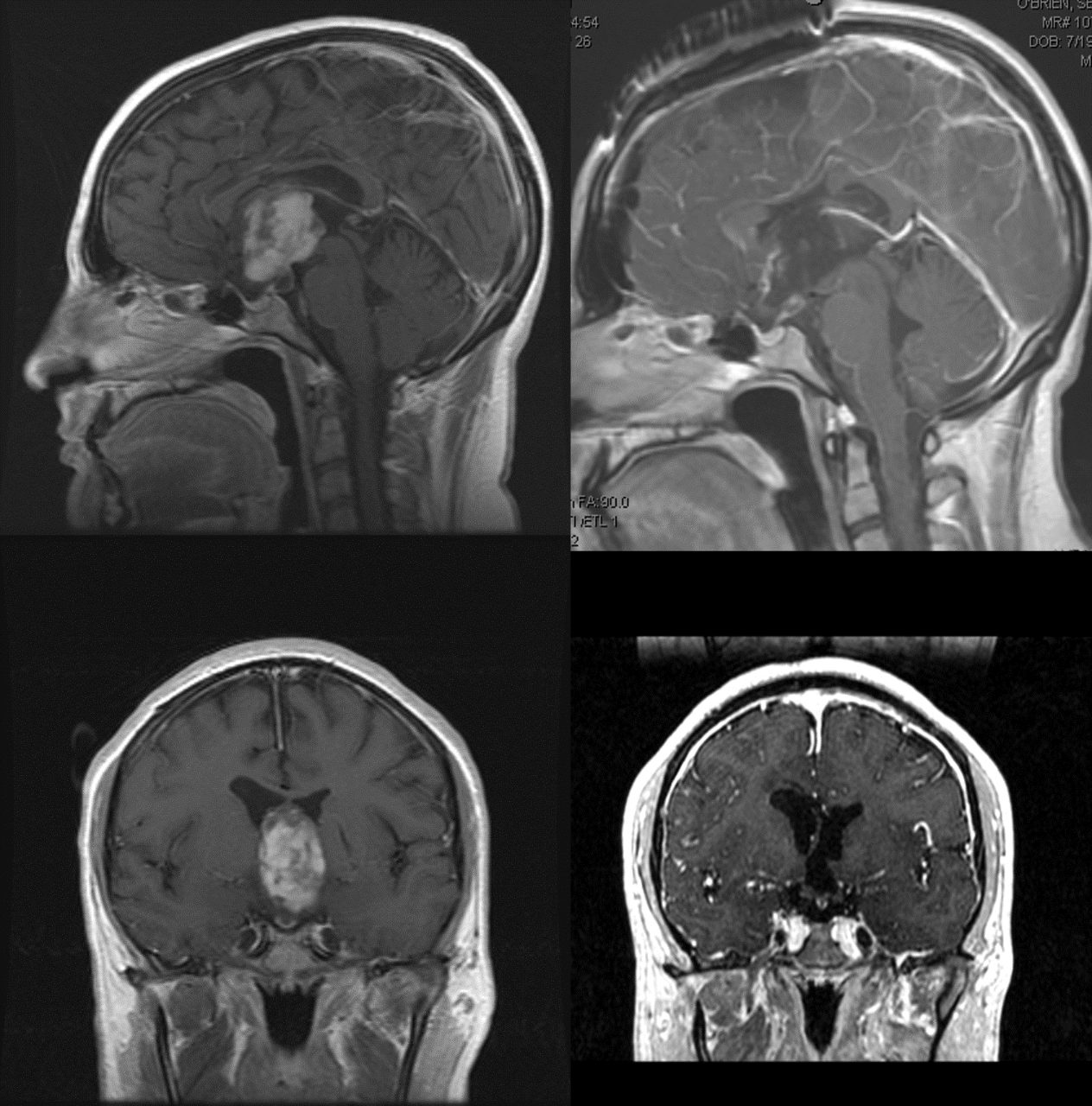
Resection of a Large Third Ventricular Pilocytic Astrocytoma
Brief History
The patient, a 21-year-old left-handed male, presented at another hospital with significant headaches and sudden transient loss of vision. Imaging revealed a large, contrast-enhancing tumor in the third ventricle.
The patient underwent an endoscopic biopsy at another hospital two years before coming to MD Anderson, and a ventriculoperitoneal shunt was placed to resolve hydrocephalus. Pathology was consistent with a pilocytic astrocytoma (PA). Subsequent scans indicated that the tumor was growing. The patient came to MD Anderson for a second opinion, and we recommended surgical resection, given that complete surgical resection of a PA can be curative.
Procedure Details
The surgical strategy was an interhemispheric, transcallosal, transforaminal approach aided by computer-assisted image guidance. The right-sided craniotomy was centered on the coronal suture and the sagittal sinus was exposed. The dura was opened and flapped medially, being careful not to over-retract on the sagittal sinus. We performed the interhemispheric dissection along the falx, first with loupes and then with the operating microscope.
We separated the left and right cingulate gyri, exposing the glistening white the corpus callosum. The two anterior cerebral arteries wereidentified and separated. We then dissected through the corpus callosum, about 3 cm from front to back, opening into the frontal horn of the right lateral ventricle. Dissecting through the septum, we entered the frontal horn of the left lateral ventricle. Draining CSF allowed us to retract the right hemisphere more laterally and permitted a larger window into the lateral ventricle.
A grayish tumor mass was visible as it expanded and came through the right foramen of Monro. Medially, the fornix and the white matter coming around the foramen of Monro were visible. The choroid plexus was more posterior, laying over part of the grayish tumor.
We began by dissecting the edge of the tumor posteriorly. We coagulated the choroid plexus and opened the tela choroidea, which gave us access to the posterior part of the third ventricle. This offered access to the posterior and opposite portion of the tumor, which we followed around.We then dissected the anterior portion of the tumor. Both that portion and the tumor base were increasingly adhesive to the surrounding brain. Laterally, the tumor was essentially infiltrating the brain tissue.We performed a circumferential dissection of the tumor. After the initial dissection, we internally debulked the tumor with bipolar cautery and suction, as well as CUSA. As the tumor was internally debulked, we were able to dissect the tumor off the walls. We used the CUSA to protect the tissue as it came off the wall, and we coagulated as minimally as possible.
Eventually, we reached the underside of the tumor at the floor of the third ventricle. We lifted the tumor off the floor, revealing arachnoid that gave us exposure to the top of the basilar artery. We then lifted the tumor out.At the end of the procedure, we felt that we had a complete resection of the tumor. We were looking at the floor and the basilar artery. We opened the arachnoid just in front of the basilar artery to create a third ventriculostomy and to open up CSF flow.Both foramen of Monro were wide open at the end of the procedure. We copiously irrigated with normal saline. The patient was valsalvaed on multiple occasions and there was no evidence of bleeding. Having completed the resection, we then slowly backed out our retractors.
Discussion
This complex operation was difficult because of the need to preserve the fornix—which was accomplished—and to remove the tumor from the wall of the ventricle.
The patient awoke able to follow simple commands, move all extremities, and with memory intact. He was brought to the intensive care unit awake. Pathology confirmed the diagnosis of a pilocytic astrocytoma, so he did not require chemotherapy or radiation. He has completed his college education and lives independently, supporting himself as a successful copyeditor. Follow-up visits have revealed no tumor recurrence after 11 years.
Previous Featured Cases
Cranial Cases Fiscal Year 2025
1,380
Total Cases
683
Stereotactic Radiosurgery Cases
Skull Base
About the section
Our skull base team is widely recognized for its extensive experience and surgical expertise. Our surgeons have been at the forefront of surgical advancements in open and endoscopic skull base surgery. For every patient, the team considers whether an open, endoscopic or combination approach will be most effective based on the specific tumor type and location. Providing expertly performed surgery, often as part of a carefully constructed, personalized multimodal care plan, is critical in optimizing our patients' outcomes.
The skull base section manages complex tumors of the skull base, including meningiomas, acoustic neuromas (also known as vestibular schwannomas), trigeminal schwannomas, jugular schwannomas, paragangliomas, glomus tumors, craniopharyngiomas, pituitary tumors, and several types of malignant skull base tumors including chordomas, chondrosarcomas, and sinonasal cancers. The most common skull base tumor locations include the intratemporal fossa, jugular foramen, clivus, foramen magnum, sella turcica, anterior cranial fossa, petrous apex, middle cranial fossa, temporal bone, posterior fossa, sinonasal tract, nasopharynx, orbit, parapharyngeal space, cavernous sinus, cerebellopontine angle and cranial nerves.
Our team utilizes several advanced technologies, including Gamma Knife Radiosurgery, virtual reality surgical planning, proton therapy, a hybrid operating room with intraoperative angiography and intraoperative MRI, endoscopic surgical suites, exoscopic technology and molecular diagnostics.
Skull base tumor cases by fiscal year
- 2020: 155
- 2021: 164
- 2022: 160
- 2023: 172
- 2024: 194
- 2025: 200
Faculty

Franco DeMonte, M.D., FRCS(C), FACS
Professor
Surgery of benign and malignant skull base tumors, meningioma, acoustic neuroma, Gamma Knife Radiosurgery

Shaan Raza, M.D.
Professor
Open and endoscopic skull base surgery, surgery of benign and malignant skull base tumors, surgery of pituitary neoplasms
Featured publication

Mehta GU, Passer JZ, Raza SM, Kim BYS, Su SY, Kupferman ME, Hanna EY, DeMonte F.
J Neurosurg. 2021 Oct 8:1-9. doi: 10.3171/2021.5.JNS21772. Epub ahead of print. PMID: 34624857
Tumors that arise in the nasal cavity and the paranasal sinuses often involve the anterior skull base and may extend intracranially. These malignancies have been managed using a variety of surgical approaches, with a more recent shift towards the incorporation of endoscopic surgical techniques.
The long-term clinical outcomes and risks associated with surgical management of sinonasal tumors extending to the anterior skull base have not been extensively studied. In this study led by Dr. DeMonte, the authors evaluated the clinical outcomes in 225 patients who were treated at MD Anderson over a period of 28 years for these types of tumors.
To account for differences in the surgical techniques and adjuvant multimodal therapies used over time, patients were stratified by the time period (decade) during which they were treated. Interestingly, while the frequency of higher-stage disease at the time of surgery increased over time, median overall survival remained stable. The rate of major complications significantly decreased from the first to the third decade studied. The use of a lumbar drain was a significant predictor of complications.
Overall, this study found that the surgical management of sinonasal malignancies with anterior skull base involvement was safe, and that the safety of surgery has improved over time most likely due to the increased use of endoscopic surgical techniques and the avoidance of the routine use of lumbar spinal drains.
Related Media
Dr. Shaan Raza
Dr. Franco DeMonte
Understanding Meningioma
Surveillance and Survivorship Clinic

The Neurosurgery Surveillance and Survivorship Clinic is a unique program that follows and provides support for patients who have benign tumors of the skull base. These patients have completed surgery or other treatment and have had stable disease for 2 years post-treatment. These patients are long-term survivors, who typically do not succumb to their disease, but may have long-lasting side effects which may appear months or even years after treatment. These side effects may include problems or changes with thinking, memory, concentration, behavior, speech, swallowing, vision, hearing, gait imbalance, fatigue, mood changes, hormone changes, and weight gain or loss. Our APP team members serve as providers for this clinic, evaluating patients using an algorithm for follow-up and maintaining close communication with the attending physicians.
Surveillance and Survivorship Clinic Team

Franco DeMonte, M.D., FRCS(C), FACS
Professor
Surgery of benign and malignant skull base tumors, meningioma, acoustic neuroma, Gamma Knife Radiosurgery

Susan Boutte, APRN, FNP-BC
Manager, advanced practice providers
Supporting: Franco DeMonte, M.D.

Shaan Raza, M.D.
Professor
Open and endoscopic skull base surgery, surgery of benign and malignant skull base tumors, surgery of pituitary neoplasms

Cheryl Martin, APN, FNP-C
APP for Skull Base Surveillance Clinic
Skull Base Fiscal Year 2025
200
Total Skull Base Cases
32
Stereotactic Radiosurgery Cases
Skull Base: Pituitary Tumor Program
About the Program
We provide comprehensive surgical care for the whole range of neuroendocrine tumors and cysts growing from the pituitary gland and for tumors growing from structures next to the pituitary that can affect it secondarily. These include pituitary adenomas (those that secrete hormones and those that do not), craniopharyngiomas, pituitary carcinomas, metastases to the pituitary from cancers elsewhere in the body, meningiomas, chordomas and Rathke’s cleft cysts. We aim to control and cure these tumors to improve patients’ hormone function, protect their vision, and thus enhance their quality of life safely and with compassion.
Our surgeons have 40 years of experience between them and have operated on more than 2,000 patients with pituitary pathology during their careers. We believe in providing safe, effective and expert care for our patients with neuroendocrine tumors, and work hard to maintain good communication with referring physicians about their patients. Our excellent clinical outcomes and extensive record of publications on pituitary disease are foundational to maintaining MD Anderson as a center of excellence for pituitary tumor care.
Pituitary tumor cases by fiscal year
- 2020: 63
- 2021: 96
- 2022: 86
- 2023: 87
- 2024: 91
- 2025: 99
Faculty

Ian
E. McCutcheon, M.D., FRCS(C)
Professor | Director, Pituitary Tumor Program
Surgery of pituitary neoplasms, spinal and brain tumors, neurofibromatosis, Gamma Knife Radiosurgery

Shaan Raza, M.D.
Professor
Open and endoscopic skull base surgery, surgery of benign and malignant skull base tumors, surgery of pituitary neoplasms
Featured Publication

Santos-Pinheiro F, Penas-Prado M, Kamiya-Matsuoka C, Waguespack SG, Mahajan A, Brown PD, Shah KB, Fuller GN, McCutcheon IE. Treatment and long-term outcomes in pituitary carcinoma: a cohort study. Eur J Endocrinol. 2019 Oct;181(4):397-407. doi:10.1530/EJE-18-0795. PMID: 31349217.
Pituitary carcinoma is a rare neuro-endocrine tumor which has historically been difficult to manage. Typically, surgery, radiation therapy or a combination of both are recommended and chemotherapy is used if surgery or radiation is not possible. Unfortunately, response to therapy is not long-term and the disease recurs in many patients, with poor prognosis.
In this article, the authors conducted a retrospective review of 17 adult patients with pituitary carcinoma who were seen over a 22-year period at The University of Texas MD Anderson Cancer Center. These patients had received multiple types of treatment for their pituitary carcinoma including surgery, radiation and chemotherapy.
The study evaluated the time that it took for the patients to have a recurrence or progression of their tumor after each type of treatment. In this group of patients, the median time between diagnosis and first recurrence of the disease was longer in patients who were treated with the chemotherapeutic agent temolozolomide (TMZ) up front.
Additionally, based on their analysis, combination therapy with surgery, radiation and chemotherapy (particularly TMZ) may result in prolonged survival. The authors conclude that management of pituitary carcinoma with multidisciplinary care and multimodality therapy, particularly therapy including TMZ, is beneficial.
Related Media
Dr. Shaan Raza
Dr. Ian McCutcheon
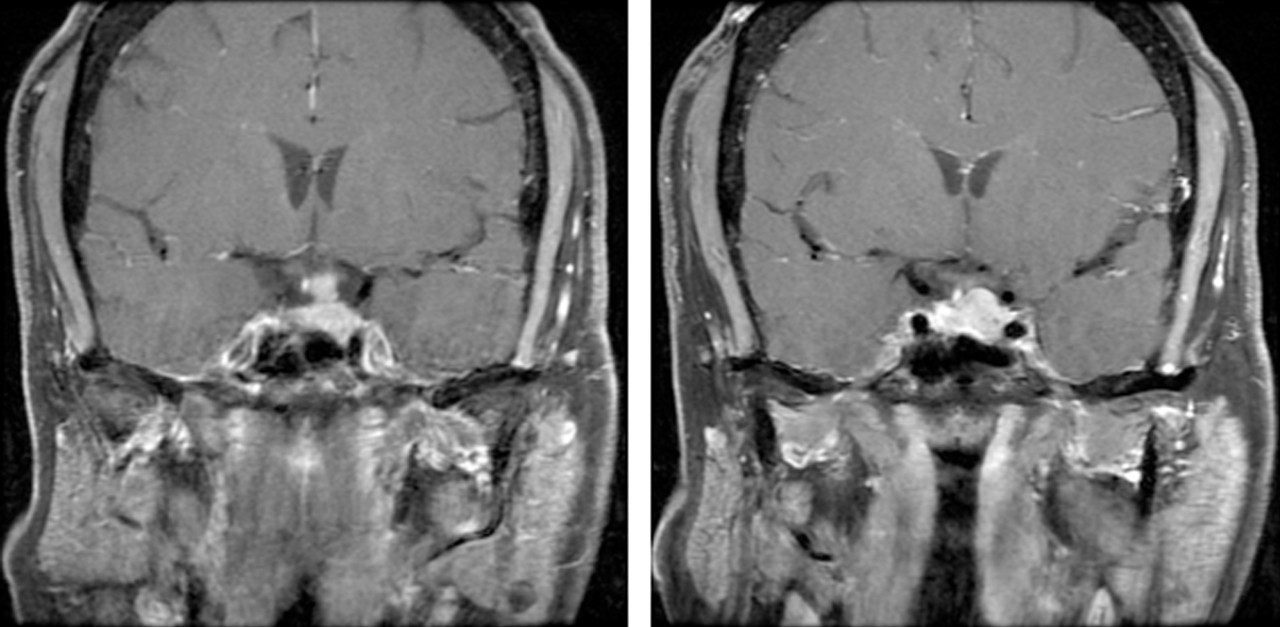
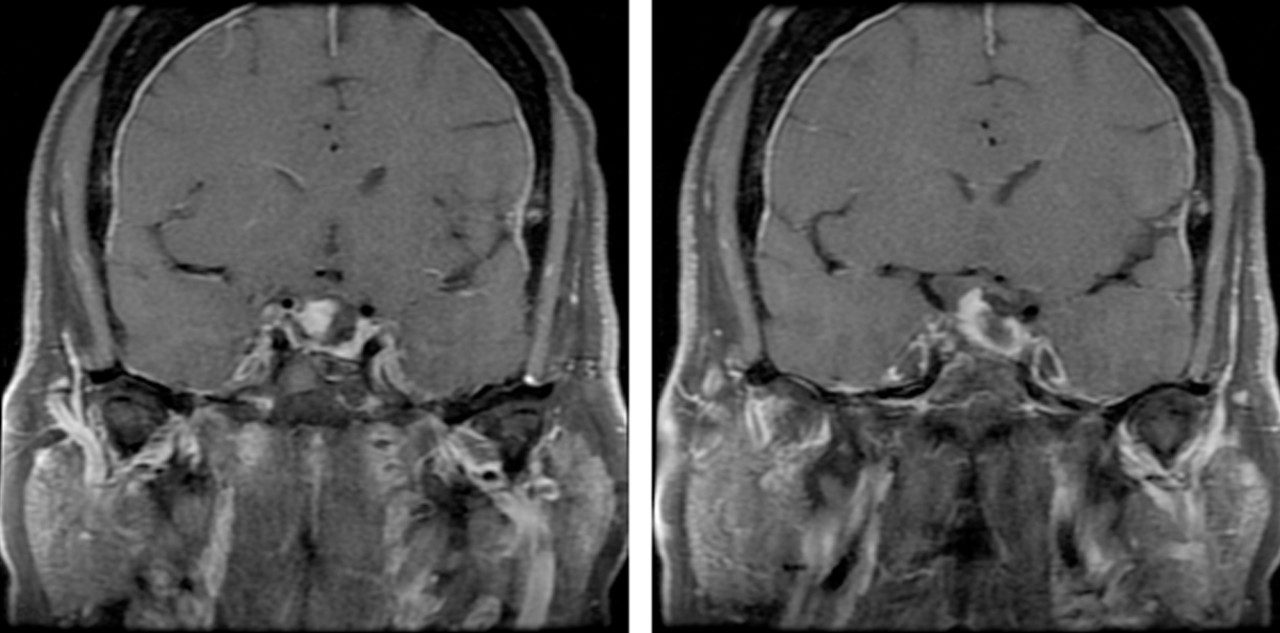
Featured Case
Pituitary Adenoma with Extension into the Subarachnoid Space
Brief History
The patient is a 51-year-old female with a history of pituitary adenoma. She had two prior surgeries to resect the tumor. She was referred to MD Anderson with worsening vision in the left eye and for consideration for a more advanced surgery. Imaging revealed a large pituitary adenoma.
Given the significant extension of the tumor into the subarachnoid space, this was not a standard pituitary tumor resection. We opted to use an endoscopic endonasal approach (EEA) to resect the tumor.
In an endoscopic endonasal approach, neurosurgeons and head and neck surgeons collaborate to access the skull base, pituitary gland and brain via the nose. The otolaryngologist removes the back of the nasal septum and the bone in front of the sphenoid sinus in two procedures: a nasal septectomy and a sphenoidotomy. Then the neurosurgeon uses an endoscope to locate the tumor and remove it.
An endoscopic endonasal approach allows access to the brain in a minimally invasive manner, protecting vital nerves and increasing the changes of complete tumor removal – depending on tumor location.
In this case, the tumor extended into the suprasellar cistern and adhered to the undersurface of the optic nerve apparatus. Furthermore, the tumor adhered to critical neurovascular structures—the supraclinoid internal and the cavernous internal carotid arteries. This complicated the procedure.
As a result, we used an expanded EEA. In an expanded EEA, the tuberculum sellae and planum sphenoidale are also removed. This permits a better view of the optic chiasm. The alternative approach for this case would have been a craniotomy.
Procedure Details
We used frameless stereotactic neuronavigation to confirm accuracy before starting surgery. The head and neck surgeon performed a posterior nasal septectomy and sphenoidotomy. They harvested a nasal septal flap pedicled on the sphenopalatine artery. Then, Neurosurgery entered the field.
Beginning with a 0° endoscope, we used a self-irrigating diamond drill bit to selectively remove parts of the bony skull base. This exposed the optic nerves, pituitary gland and carotid arteries. We used the Doppler to confirm the location of the carotid arteries and the ophthalmic arteries. Then we opened the dura in a manner that exposed the optic nerves, carotid arteries, pituitary gland and tumor.

We identified the pituitary gland along the right lateral aspect of the sella. We also identified the tumor, which extended into the subarachnoid space. We used scissors to cut the arachnoid and access the tumor.
First, we internally debulked the tumor. Then we opened the diaphragma sella and carried out laterally towards the supraclinoid internal carotid artery. We worked posteriorly to sharply dissect the posterior aspect of the tumor away from the optic chiasm and the left optic tract.
The posterior aspect of the tumor extended into the interpeduncular cistern. As we dissected this aspect of the tumor, we could clearly see the basilar apex.
Next, we sharply dissected the superior pole of the tumor away from the undersurface of the left optic nerve. This component of the tumor was extremely adherent to the nerve. A significant amount of sharp dissection was required to preserve the vasculature to the nerve.
Ultimately, we were able to detach the tumor from the lateral aspect of the sella. At this point a gross total resection had been achieved. We had a clear view of the medial cavernous sinus wall along the left side and of the pituitary gland along the right side. The floor and all the gutters were inspected; no evidence of residual disease was noted.

We then began reconstruction of the skull base defect. We used a multilayer technique by using several tissue layers to close the dura—including using vascularized tissue from within the nasal cavity.
Despite the patient’s previous surgical resections before presenting to MD Anderson, a successful closure and tumor removal was performed. A postoperative MRI scan done while in the hospital demonstrated a complete tumor resection. The patient’s native pituitary gland function was preserved.
For several weeks after the procedure, the patient experienced headaches and blurry vision. Over time, these issues resolved.
Discussion
A pituitary adenoma, also called a pituitary tumor, is a growth on the pituitary gland. Pituitary tumors are usually benign. Still, pituitary tumors can cause problems when they grow and impinge on surrounding structures.
People generally do not experience symptoms of pituitary tumors until they have grown large. Symptoms may include headaches or vision problems. Sometimes pituitary tumors cause other glands to make too much hormone.
Some people have conditions that make them prone to pituitary tumors. Pituitary tumors may require surgery to be removed. In other cases, medication or radiation treatments are used to manage pituitary tumors.
Spine
About the Section
Our spine surgeons are widely recognized for their extensive experience and expertise, performing more spine tumor surgeries than any other hospital in the nation. Known for our innovation, we utilize advanced technologies including intraoperative imaging, spinal navigation, laser interstitial thermal therapy (LITT), and minimally invasive techniques to optimize outcomes for each individual patient. Many of these advances have been developed and optimized at M.D. Anderson. Moreover, we collaborate extensively with colleagues in plastic surgery, vascular surgery, colorectal surgery, orthopedic surgery, and head and neck surgery to bring multidisciplinary surgical expertise to our complex patient population.
Beyond the operating room, we work hand-in-hand with our radiation oncologists, medical oncologists, pain management specialists, and physiatrists. We recognize that expertly performed surgery is only one part of the carefully designed, personalized, multimodal plan of care needed to offer the best results for our patients.
The spine section treats patients with primary and metastatic tumors of the spinal column, spinal cord, and peripheral nerves. Primary bone tumors include hemangioma, aneurysmal bone cyst, osteoblastoma, giant cell tumor, chordoma, chondrosarcoma, osteosarcoma, Ewing’s sarcoma, and soft tissue sarcomas. We specialize in techniques of en bloc resection (removing the tumor in one piece) needed to provide patients with malignant bone tumors the best chance of cure. Tumors of the intradural space (including the spinal cord) include meningioma, schwannoma, neurofibroma, ependymoma, astrocytoma, and hemangioblastoma. We also have a world-class program for treating spinal metastases (tumors that have spread to the spine from other organs including the breast, kidney, lung, colon, prostate, etc.).
In collaboration with our radiation oncologists, we have built one of the busiest spinal stereotactic radiosurgery programs in the world. This technology allows us to deliver high-dose, focused, conformal radiation to spine tumors, improving our ability to treat symptoms and protect neurologic function. Used in conjunction with our minimally invasive stabilization techniques, laser interstitial thermal therapy, and vertebral augmentation, we are able to treat spinal metastases with fewer complications and shorter hospital stays, allowing our patients to return to an active life.
Spine tumor cases by fiscal year
- 2020: 234
- 2021: 263
- 2022: 252
- 2023: 263
- 2024: 260
- 2025: 302
Faculty

Laurence D. Rhines,
M.D.
Professor | Director, Spine Tumor Program
Surgery for primary and metastatic spinal tumors, spine stereotactic radiosurgery

Robert North, M.D., Ph.D.
Assistant Professor
Surgery for tumors of the spine and spinal cord

Claudio Tatsui, M.D.
Professor
Surgery for spine and spine tumors, application of local delivery technologies to the treatment of brain and spinal tumors, laser interstitial thermal therapy for spine

Christopher A. Alvarez-Breckenridge, M.D., Ph.D.
Assistant Professor
Spinal tumors, metastatic disease involving the brain and spine, immunotherapy
Featured Publication

Outcomes of Surgery for Sacral Chordoma and Impact of Complications: A Report of 50 Consecutive Patients With Long-Term Follow-Up. Zuckerman SL, Lee SH, Chang GJ, Walsh GL, Mehran RJ, Gokaslan ZL, Rao G, Tatsui CE, Rhines LD Global Spine J. 2021 Jun;11(5):740-750. doi: 10.1177/21925682211011444. PMID: 34047643; PMCID: PMC8165918.
Sacral chordomas are primary bone tumors found along the axial skeleton, most commonly arising in the sacrococcygeal region.
While en bloc resection is the preferred treatment for sacral chordomas due to the limited response of these tumors to radiation and chemotherapy, the large size of many sacral chordomas at diagnosis and complex anatomy of the sacropelvic region often make this approach difficult and increase the risk of surgical complications. As such, it is important to identify whether perioperative factors, such as surgical complications, predict postsurgical outcomes in these patients.
A series of 50 patients who underwent en bloc resection of a sacral chordoma at MD Anderson Cancer Center from January 1995 to June 2016, was reviewed. After a median of 5.3 years of follow-up, our team, led by Laurence Rhines, M.D., found that while negative margin resection was associated with a decreased risk of local recurrence, major complications and reoperation did not significantly impact overall survival, local recurrence, or functional outcome.
Therefore, it appears that the inherently high surgical morbidity associated with these invasive operations does not adversely alter the trajectory of survival and recurrence.
Related Media
Dr. Laurence Rhines
Surgical Management of Spinal Tumors
Q & A : Chordoma Treatments
Dr. Claudio Tatsui
Featured Case
Brief History
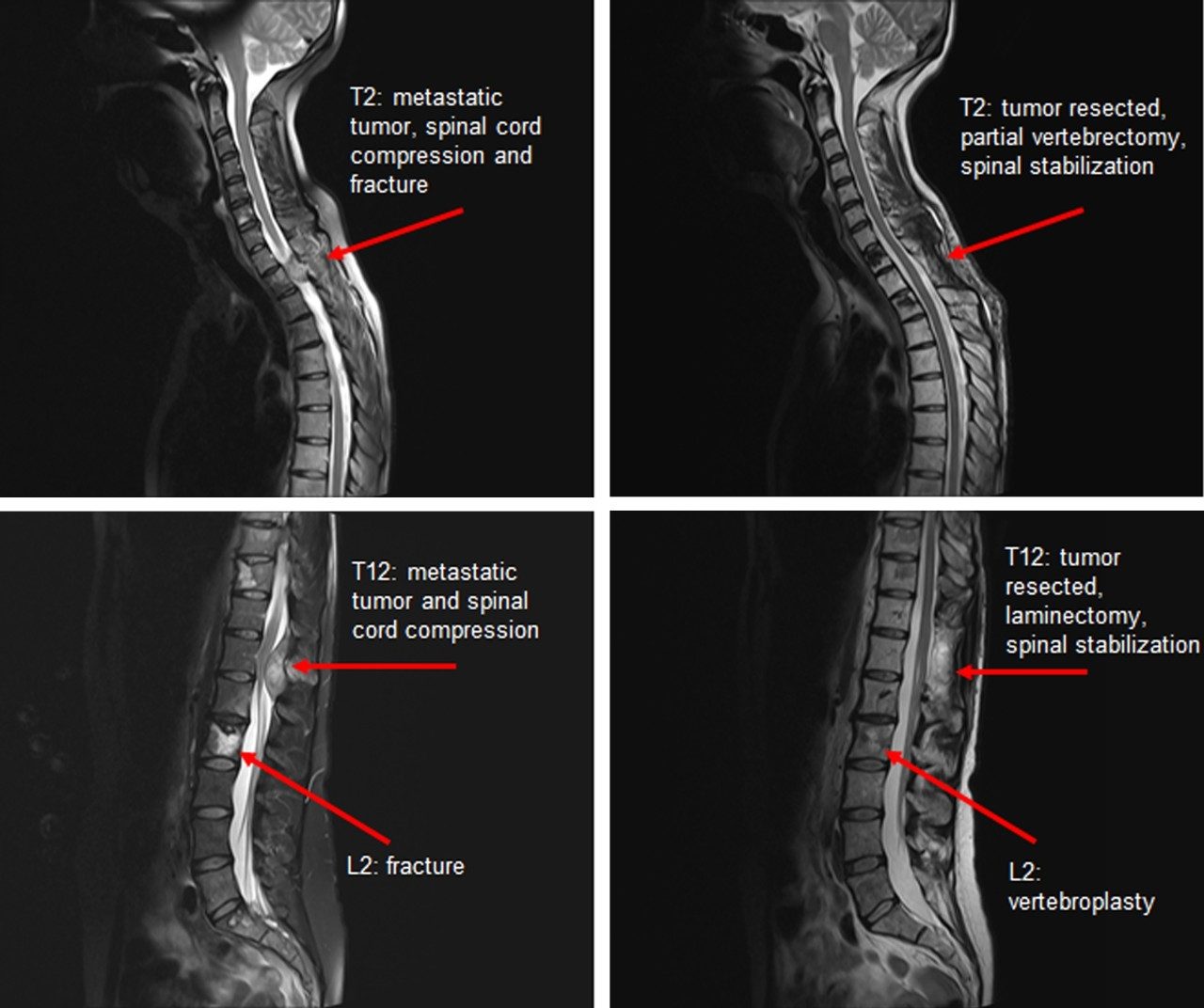
This patient is a 36-year-old female who has a history of metastatic catecholamine-producing sympathetic paraganglioma with widespread skeletal metastasis including the spine. She had previously undergone multiple surgeries for skeletal metastasis including in the thoracic spine, shoulders, hips, and long bones of the extremities.
She presented to the MD Anderson Brain and Spine Center with symptoms of worsening upper and lower back pain as well as imaging findings of multi-site progressive spinal metastatic disease. More specifically, she had pathological fractures of T2 and L2 vertebra, high-grade spinal cord compression from metastatic tumor at two separate sites (T2 and T12), and thoracic radiculopathy (a compressed nerve in the thoracic region).
We recommended a surgical plan to treat all the sites in a single stage surgical procedure with pre-operative embolization to reduce intraoperative blood loss. Specifically, we recommended partial T2 vertebrectomy with instrumented spinal stabilization/fusion, T11-T12 laminectomy with tumor resection and instrumented spinal stabilization/fusion, and a L2 vertebroplasty. Radiolucent carbon-fiber reinforced PEEK spinal instrumentation was utilized to facilitate adjuvant radiosurgery planning and improve surveillance imaging.
Surgery and Post-surgical Recovery
The procedures were completed not only on the same day, but in the same operating session and without complication. After surgery our patient remained neurologically intact and was able to be discharged home from the hospital after a brief, uneventful convalescence. She was able to go on to receive adjuvant stereotactic radiosurgery to progressive tumors to facilitate local control.
After her initial recovery the patient was able to resume normal activities. At three months follow up, an MRI of the spine revealed stability of the lesions. A year later, treated lesions remained stable. MD Anderson’s team of surgeons and physicians, stereotactic radiosurgery program, and world-class intraoperative imaging abilities allowed the best outcome for this patient.
Discussion
Paragangliomas are rare tumors. These tumors can occur on the head or neck, but sites of origin may include the spine or elsewhere in the body. Most paragangliomas are benign, but some become cancerous and spread throughout the body. More specifically, a paraganglioma is a type of neuroendocrine tumor (NET). Neuroendocrine cells are nerve cells that produce hormones. Neuroendocrine tumors (NET) are tumors of these cells.
Paraganglioma usually appears in adults aged 30 – 50. People with paraganglioma may experience symptoms like rapid heartbeat, high blood pressure, shakiness, headache, and sweating. Surgery is usually required to treat paraganglioma. Treatment and management of paraganglioma requires specialized equipment and multidisciplinary expertise. Causes of paraganglioma are unknown. Scientists believe that paragangliomas come from mutations of chromaffin cells – nervous system cells. A paraganglioma that occurs in the adrenal gland is called pheochromocytoma.


Spine Cases Fiscal Year 2025
302
Total Spine Cases
Peripheral Nerve Tumor Program
About the Program
We provide safe, compassionate, careful and effective surgical care for patients with all varieties of tumors arising in peripheral nerves. This includes benign nerve sheath tumors such as neurofibromas and schwannomas that are associated with the genetic syndromes neurofibromatosis and schwannomatosis, more aggressive, malignant nerve sheath tumors such as malignant peripheral nerve sheath tumors (MPNST), perineuromas, ganglioneuromas, desmoid tumors, neuromuscular choristomas, intraneural ganglion cysts and neuromas. We aim to control and cure these tumors to reduce patients’ symptoms, including pain, weakness and numbness, and in so doing, enhance their quality of life.
Our two surgeons specializing in peripheral nerve surgery serve a clinic that follows 1,600 patients, the largest in North America. Many of these patients require surgical care on multiple occasions. We operate in all areas of the body to remove nerve tumors while sparing the nerve of origin and employ intraoperative nerve monitoring. When needed, we are adept at restorative surgery (including nerve grafts, nerve transfers and regenerative peripheral nerve interface). Our excellent clinical outcomes, wide-ranging publications on nerve tumors and collaborative care involving a neurologist who coordinates medical care for these patients make this a center of excellence without peer in this country.
We are leaders in education on surgical techniques for treating peripheral nerve tumors, done both didactically and through directed participation in clinical care. We participate actively in postgraduate education through lectures in national and international forums and our involvement in hands-on courses and workshops. Our innovative clinical trial protocols and basic research in this area make us a unique venue to learn the principles and nuances of serving patients with simple and complex nerve tumors, whether benign or malignant in character.
Peripheral nerve tumor cases by fiscal year
- 2020: 22
- 2021: 21
- 2022: 40
- 2023: 59
- 2024: 57
Faculty

Ian
E. McCutcheon, M.D., FRCS(C)
Professor | Director, Peripheral Nerve Tumor Program
Surgery of peripheral nerve tumors, neurofibromatosis, pituitary neoplasms, spinal and brain tumors, Gamma Knife Radiosurgery

Robert North, M.D., Ph.D.
Assistant Professor
Brachial plexus and peripheral nerve tumors, nerve reconstruction, nerve transfers for functional restoration, nerve entrapments including carpal tunnel syndrome, cubital tunnel syndrome, and peroneal neuropathy
Featured Publication

Landry JP, Schertz KL, Chiang YJ, Bhalla AD, Yi M, Keung EZ, Scally CP, Feig BW, Hunt KK, Roland CL, Guadagnolo A, Bishop AJ, Lazar AJ, Slopis JM, McCutcheon IE, Torres KE. Comparison of Cancer Prevalence in Patients With Neurofibromatosis Type 1 at an Academic Cancer Center vs in the General Population From 1985 to 2020. JAMA Netw Open. 2021 Mar 1;4(3):e210945. doi: 10.1001/jamanetworkopen.2021.0945. PMID: 33734413; PMCID: PMC7974640.
Neurofibromatosis type 1 (NF1) is a complex genetic disorder which can result in the development of benign and malignant tumors. Although it is known that NF1 is associated with the development of tumors, the risk of developing specific types of tumors in those patients with NF1 is not known.
This large study of patients diagnosed with NF1 between 1985 and 2020 was conducted to determine the prevalence of specific tumor types in NF1 patients, collect information on how their disease was treated or managed and what their clinical outcomes were.
This study found that patients with NF1 develop tumors more frequently and at a younger age than the general population, and the most common tumor types were low grade gliomas, malignant peripheral nerve sheath tumors (MPNST), breast cancer, pheochromocytoma, gastrointestinal stromal tumors (GIST) and melanoma. NF1 patients with undifferentiated pleomorphic sarcoma, high grade gliomas, MPNST, ovarian carcinoma and melanoma had significantly lower disease specific survival rates when compared with patients who developed other types of tumors.
The findings from this study may be useful for follow up and counseling of NF-1 patients and supports a multidisciplinary approach to NF1 patient care.
Related Media
Featured Case
Brief History
This patient is a 30-year-old woman with a pilocytic astrocytoma of the upper cervical spinal cord. She was initially diagnosed and treated as a child.
Prior to coming to MD Anderson, she had undergone several surgeries attempting to remove the tumor. She had also undergone radiation therapy and surgery to correct spinal deformity, including screws and rods surgically inserted to fuse and stabilize her spine.
Despite surgical resection and radiotherapy, the tumor continued to grow very slowly. The combination of tumor growth and effects from multiple surgeries and radiation therapy lead to chronic, severe weakness in both her legs and left arm.
When the patient came to us, she had started to develop progressive weakness in her right arm, which she relied on for most of her activities. The weakness was most pronounced in movements of the shoulder and elbow. The weakness in elbow flexion (or bending her elbow) was preventing her from performing many daily tasks of living.
Our clinical examination, electromyography (EMG), and nerve conduction study (NCS) indicated that radiation-induced lower motor neuron disease and cervical spinal cord dysfunction (cervical myelopathy) was the reason for worsening symptoms.
We felt that attempts at resecting the tumor or further correction of the spinal deformity would risk devastating complications, canceling out any possible benefits. Therefore, we chose a more isolated goal: to improve elbow flexion strength.
To that end, we recommended a rerouting of the nerves in her arm, also known as a nerve transfer. In a nerve transfer, a healthy nerve is connected to a damaged nerve. The healthy nerve is the donor nerve. The damaged nerve is the recipient nerve.
In this case, we recommended using a small portion of the ulnar nerve to be rerouted to the brachialis branch of the musculocutaneous nerve. The ulnar nerve primarily helps with hand movements; the musculocutaneous nerve helps with elbow flexion.
Key to the transfer was to only take a small portion of the ulnar nerve so as not to cause problems with hand movements. Still, we had to take enough to provide nerve signals to the muscles for flexing the elbow. A similar nerve transfer of the ulnar nerve to the biceps branch of the musculocutaneous nerve is more commonly performed. However, we chose to transfer to the brachialis branch because the patient’s biceps muscle was stronger to begin with, and we didn’t want to risk damaging its function.
Procedure Details
During surgery, the patient was under general anesthesia with her arm outstretched. Following incision, we identified the relevant nerves. We carefully isolated several branches of the musculocutaneous nerve. We cut one nerve branch to the brachialis muscle proximally along its origin to the musculocutaneous nerve.
We then isolated a portion of the ulnar nerve using internal neurolysis. We confirmed it to have motor function and that the remaining ulnar nerve would still carry signals to control the hand. This isolated portion served as the donor nerve.
We cut the donor nerve and transferred it toward the isolated nerve to brachialis, tunneling underneath the surrounding nerves and soft tissue. We connected the nerve ends using a surgical microscope, very small sutures (with a thickness of only 0.040 mm) and a biocompatible glue.
After seven months, the patient had improved functioning of her right arm. In fact, she could completely actively flex that arm. She could also perform essential activities of daily life: feeding herself with the right hand, washing her face, combing her hair and even writing. She continued physical therapy, and her functioning improved. She was able to work full time.
Discussion
The Peripheral Nerve section at the MD Anderson Neurosurgery department has experience treating many types of nerve disorders. This case is a good example of how our team treats conditions beyond just the primary cancer; we also treat problems associated with cancer treatments.
While this patient did have a history of cancer, further tumor resection was not an option. It was also not possible to repair the damage induced by radiation. Instead, we focused on restoring function and improving quality of life through a unique and novel nerve transfer procedure.
This case involved a novel nerve transfer procedure that was uniquely tailored for our patient and is not part of the standard treatment options. Instead of transferring ulnar fascicle to the biceps branch of the musculocutaneous nerve, we transferred it to the brachialis branch.
The result was the same: successful restoration of elbow flexion and improved quality of life. This case study is also described in a published article by Larkin et al.




Peripheral Nerve Cases Fiscal Year 2025
57
Total Peripheral Nerve Cases
Endovascular Neurosurgical Oncology Program
About the Program
The Endovascular Neurosurgical Oncology program provides standard-of-care endovascular treatment to neuro-oncology patients, pursues clinical trials and performs basic and translational research studies to further this endeavor.
Endovascular neurosurgical oncology is a relatively new sub-specialty discipline that includes neuro-oncology, surgical neuro-oncology, diagnostic radiology, neurointerventional radiology and cerebrovascular neurosurgery. Modern endovascular neurointerventional techniques have significantly enhanced the outcomes for the treatment of cerebrovascular disease and have more recently been applied in the field of neurosurgical oncology.
Our program consists of dual-trained cerebrovascular neurosurgeons, interventional radiologists and a cranial neurosurgeon. We currently provide standard-of-care endovascular diagnostic procedures, including diagnostic cerebral angiogram, balloon test occlusion, Wada test, and inferior petrosal sinus sampling. We also perform surgical adjuncts, including pre-operative brain and spinal tumor embolization, as well as endovascular vessel repair and sacrifice for complex skull base and head and neck tumors.
As part of a broader cancer cerebrovascular neuroscience program, we also focus on treatment of cerebrovascular disease in the cancer patients and survivors with an active clinic to provide tailored cerebrovascular care to our patients at MD Anderson. This includes the management of radiation-induced arteriopathy, ischemic strokes, and brain hemorrhages associated with oncologic treatments.
Read more about our phase 1 clinical trial studying best dose and side effects of oncolytic adenovirus DNX-2401 in treating patients with high-grade glioma that has come back (recurrent).
Endovascular cases by fiscal year:
- 2020: 15
- 2021: 11
- 2022: 9
- 2023: 9
- 2024: 81
Faculty

Christopher Young, M.D., Ph.D.
Assistant Professor
Endovascular and open cerebrovascular surgery for brain aneurysms, arteriovenous malformation (AVM), carotid stenosis, cavernoma, hemorrhagic and ischemic strokes, chronic subdural hematomas, intraarterial therapy for brain tumors

Omar Tanweer, M.D.
Associate Professor (Adjunct)
Open surgical, endovascular and radiosurgical treatment options

Peter Kan, M.D.
Clinical Associate Professor (Adjunct)
Cerebrovascular and neuroendovascular surgery

Steven Chen, M.D.
Associate Professor, Department of Interventional Radiology
Brain and spine tumors, intra-arterial chemotherapy, head and neck cancer, retinoblastoma, and image-guided cancer therapy
Featured Publication

Young CC, Kan P, Chen SR, Lang FF. Endovascular surgical neuro-oncology: advancing a new subspecialty. J Neurooncol. 2024 Sep 2. doi: 10.1007/s11060-024-04782-4. Epub ahead of print. PMID: 39222190.
Endovascular surgical neuro-oncology uses endovascular neuro-interventional techniques for the management of nervous system tumors and tumor-related vascular conditions. There has been a renewed interest to explore endovascular approaches as a means for selective intra-arterial delivery of therapeutic agents to nervous system tumors, including methods for opening the blood brain and blood tumor barriers.
This review discusses the historical development of various forms of endovascular intra-arterial treatment for tumors over the past 40 years, summarizes endovascular approaches that are currently being employed, and highlights current clinical trials.
Related Media
Meet neurosurgeon Christopher Young, M.D., Ph.D.
Featured Case
Bilateral MMA embolization to treat chronic subdural hematoma in preparation for chemotherapy
Brief History
A 56-year-old female patient presented with bilateral chronic subdural hematoma (cSDH). She had been recently newly diagnosed with Burkitt’s lymphoma and severe thrombocytopenia.
Because induction chemotherapy would likely exacerbate the thrombocytopenia, Neurosurgery was consulted to perform a diagnostic angiogram and possible middle meningeal artery (MMA) embolization.
Procedure Details
With the patient positioned supine, we punctured the right radial artery under ultrasound guidance. A 5 French sheath was placed.
Over an exchange length Rosen wire, radial sheath was exchanged for an 071 RIST guide catheter. A Sim2 select catheter was introduced over a Glidewire and reformed in the aortic arch. The left common carotid artery (CCA) was selected. Cerebral angiography demonstrated normal-appearing ophthalmic artery with retinal choroid blush. Under roadmap guidance, the guide catheter was advanced into the distal left external carotid artery (ECA). Cerebral angiogram of the left ECA demonstrated prominent MMA anterior branches, which appeared to supply a cSDH membrane over the convexity and vertex. The microcatheter was navigated over the microwire into the MMA into the prominent anterior branch distally and well above the skull base. The microwire was removed, and the microcatheter was primed with dimethyl sulfoxide. Onyx 18 liquid embolic agent was administered with satisfactory uptake of the Onyx up towards the convexity and vertex with very good penetration of chronic subdural membrane. Repeat cerebral angiogram of the left ECA demonstrated occlusion of the MMA without further opacification with a satisfactory Onyx cast.
Attention was then turned to the right side. The right CCA was selected. Cerebral angiography demonstrated normal-appearing ophthalmic artery with retinal choroid blush and absence of unusual ECA to ICA anastomosis. The guide catheter was advanced into the distal right ECA. Cerebral angiogram of the right ECA demonstrated prominent MMA anterior branches. These branches appear to supply a cSDH membrane over the convexity and vertex. The microcatheter was navigated over the microwire into the MMA into the prominent anterior branch distally and well above the skull base. The microwire was removed and the microcatheter was primed with dimethyl sulfoxide. Under blank road map guidance, Onyx 18 liquid embolic agent was administered. There was satisfactory uptake of the Onyx up towards the convexity and vertex. When no further progression of Onyx was encountered, the microcatheter was retracted and removed. Repeat angiogram of the right ECA demonstrated occlusion of the distal anterior branch. However, there remained a persistent posterior parietal branch. The microcatheter was navigated into a posterior parietal branch and the branch embolized as above with liquid embolics. Repeat cerebral angiogram of the right ECA demonstrated occlusion of the MMA. The RIST catheter was retracted into the right CCA and repeat cerebral angiography was performed without untoward findings.
All catheters were withdrawn uneventfully. A TR band was used for hemostasis.
Chronic subdural hematoma treatment in oncological patients: middle meningeal artery embolization versus surgical drainage
Ramirez-Ferrer, E., Zuluaga-Garcia, J. P., Weinberg, J. S., Ene, C. I., Raza, S. M., Lang, F. F., Kan, P. T., Chen, S. R., & Young, C. C. (2025). Chronic subdural hematoma treatment in oncological patients: middle meningeal artery embolization versus surgical drainage. Neurosurgical Focus, 59(4), E14.
Pre-op CT Scan



Endovascular Cases Fiscal Year 2025
109
Total Endovascular Cases


