request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Skull Base Tumors
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsThe skull base is the area behind the eyes and nose that slopes down to the back of the head. It forms the floor, or base, of the skull and can be imagined as the wall between the brain and the face.
The skull base is the area behind the eyes and nose that slopes down to the back of the head. It forms the floor, or base, of the skull and can be imagined as the wall between the brain and the face.
Many nerves, blood vessels, and the spinal cord pass through openings in the skull base. Several different tumor types start in or extend into this area. These tumors can be malignant (cancer) or benign (not cancer). Even benign tumors can cause symptoms or threaten the health and well-being of the patient.
At MD Anderson, physicians and specialists in the Skull Base Tumor Program treat patients with both cancerous and noncancerous tumors of the skull base.
Skull base tumor classifications
Skull base tumors can be classified based on their specific location in the head (the tumor site) or based on the cell structure and identifying characteristics of the tumor (the tumor type).
Tumor typing is determined during the patient's diagnostic workup. Radiologists and pathologists who have special expertise in tumors of the head and brain work closely with head and neck surgeons and neurosurgeons to determine tumor type.
The tumor type, together with the unique health profile and needs of each patient, helps the skull base team specifically tailor treatment to each patient.
MD Anderson is #1 in Cancer Care
Skull base tumor types and locations
Skull base tumor types
The most common malignant skull base tumors include:
- Adenocarcinoma
- Adenoid cystic carcinoma
- Chondrosarcoma
- Chordoma
- Esthesioneuroblastoma or olfactory neuroblastoma
- Nasopharyngeal carcinoma
- Non-Hodgkin’s lymphoma
- Squamous cell carcinoma
Other malignant skull base tumors:
- Endolymphatic sac tumor
- Mucosal melanoma
- Metastases
- Mucoepidermoid carcinoma
- Myeloma/plasma cell tumors
- Neuroendocrine carcinoma
- Sarcomas. The more common sarcomas are as follows:
- Ewing's sarcoma
- Osteosarcoma
- Rhabdomyosarcoma
- Sinonasal undifferentiated carcinoma
The most common benign skull base tumors include:
- Acoustic neuroma (vestibular schwannoma)
- Cholesteatoma
- Meningioma (the most common skull base tumor)
- Pituitary tumors
Other benign skull base tumors:
- Juvenile angiofibromas
- Cholesterol granuloma, epidermoid and dermoid cysts
- Craniopharyngiomas
- Fibro-osseous lesions. These include the following:
- Fibrous dysplasia
- Ossifying fibroma
- Osteoma
- Hemangioma
- Inverting papilloma
- Lipoma
- Paraganglioma:
- Carotid body tumors
- Glomus jugulare
- Glomus tympanicum
- Glomus vagale
- Schwannomas:
- Jugular foramen schwannoma
- Trigeminal schwannoma
- Schwannomas on other cranial nerves
Head and neck tumors may also extend to the skull base. Examples include:
- Salivary gland tumors. The most common types of salivary gland cancers are mucoepidermoid carcinoma and adenoid cystic carcinoma.
- Skin cancers, such as squamous cell carcinoma, melanoma and basal cell carcinoma, that can travel along nerves and spread to the brain and skull base.
Skull base tumor locations
Tumors of the skull base can occur in various areas within the skull base. Our team of experts apply highly specialized knowledge and skills from across disciplines to treat patients with tumors in all of these locations.
Below is a list of the most common locations for skull base tumors.
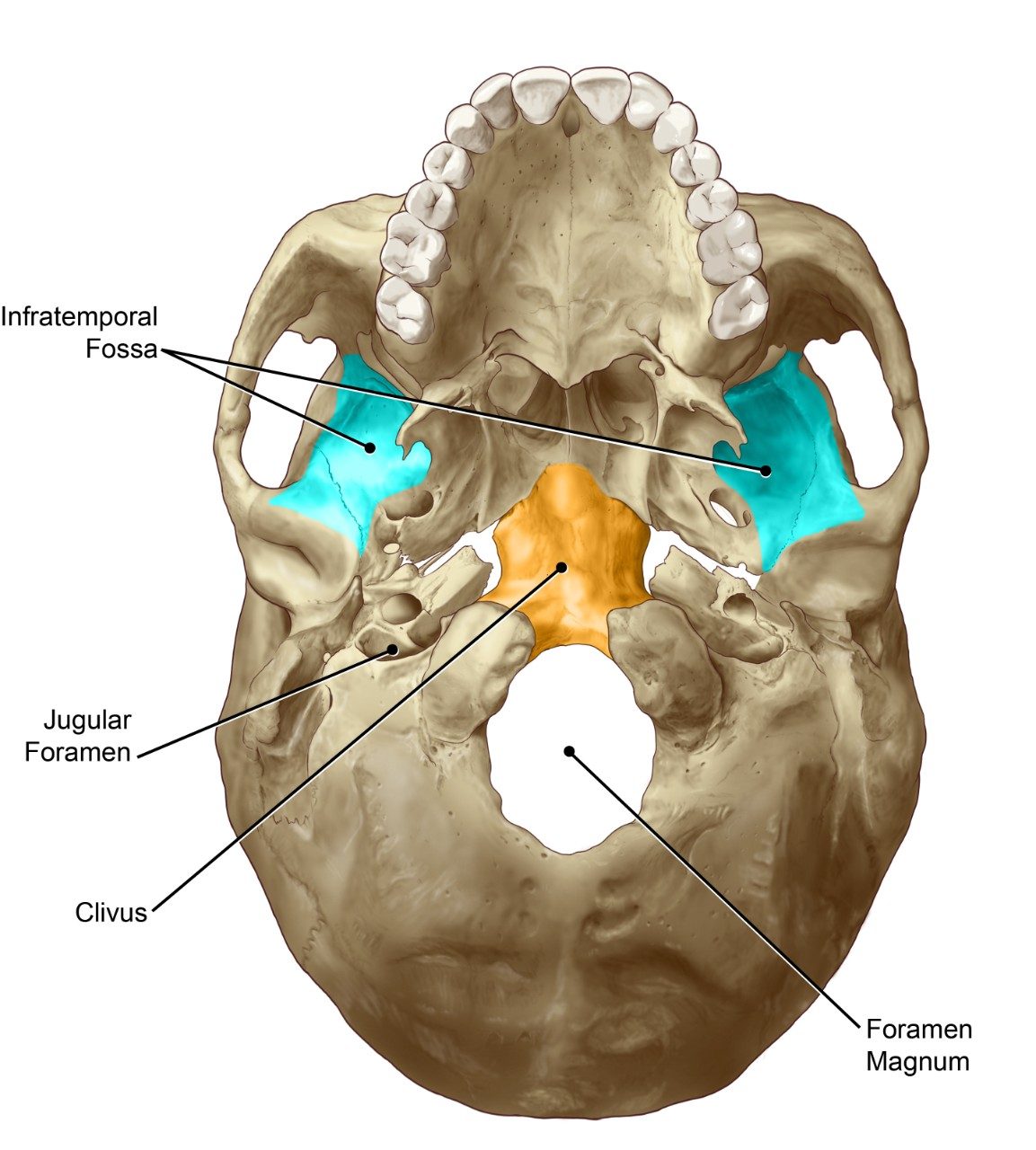
Infratemporal Fossa: This is the space that lies behind the maxilla (the upper jaw) and below the side wall of the skull. It contains several nerves that give sensation to the face, the muscles used for chewing, and several blood vessels, including the carotid artery and the jugular vein. Tumors in this location can come from the ear, the salivary glands and the upper or lower jaw.
Jugular Foramen: The jugular foramen is an opening in the skull base that contains several vital structures. It is located underneath the temporal bone. Blood drains from the brain down to the jugular vein in the neck by passing through the jugular foramen. The lower cranial nerves designated as IX, X and XI pass from the brain through the jugular foramen into the neck.
Clivus: Deep within the head lies the floor of the cranial cavity, which contains the brain. The bone in the central portion of this cranial floor is known as the clivus. Access to this region is often obtained through the nasal cavity and sinuses, thus avoiding external scarring. Common tumors in this region are chordoma, chondrosarcoma and meningioma.
Foramen Mangum: At the base of the skull lies this large, bony opening, through which the lowest portion of the brain joins and becomes continuous with the spinal cord. This region contains the complex joint system that attaches the skull to the spine.

Sella Turcica: The sella turcica is a depression in the midline of the sphenoid bone, an irregular shaped bone at the cranial floor. It contains the pituitary gland. Pituitary tumors typically arise in the pituitary gland within the sella turcica. The cavernous sinuses are on each side of the sella turcica. The sella turcica is most commonly accessed through the nasal cavity.
Anterior Cranial Fossa: The front portion of the cranial floor is known as the anterior cranial fossa. The anterior cranial fossa supports the frontal lobes of the brain. It includes the olfactory grooves where the sense of smell is perceived. The middle part of the anterior cranial fossa forms the roof of the nasal cavity, whereas the outer parts of the anterior cranial fossa form the roofs of the orbits. Meningioma is a common tumor in this area.
Petrous Apex: The tip of the bony portion of the temporal bone is known as the petrous apex. The petrous apex is located close to several cranial nerves, including nerves designated as V through VIII. It is the bony boundary of the cerebellopontine angle.
Middle Cranial Fossa: The middle portion of the cranial floor is known as the middle cranial fossa (includes the Greater Sphenoid Wing). The middle cranial fossa supports the temporal lobes of the brain and forms the outer walls of the orbits. The bone of the middle cranial fossa separates the ear from the brain.
Temporal Bone: Two temporal bones form part of the side surfaces and the base of the skull. The temporal bone is the hardest bone in the body and has a very complex anatomy. It contains the ear canal (external ear) with the eardrum, and small bones (ossicles) in the middle ear. The temporal bones encase the facial nerve and the organs deep within the ear that control hearing and balance (the inner ear). Large air-filled spaces are present in part of the temporal bone. The carotid artery passes from the neck through the temporal bone, and blood from the brain drains through a space underneath the temporal bone.
Posterior Cranial Fossa: The back portion of the cranial floor, known as the posterior cranial fossa, encases the cerebellum (the portion of the brain that controls coordination of movement) and the brainstem (made up of the midbrain, pons and medulla oblongata).
Sinonasal Tract: The sinonasal tract consists of the nasal cavity (or the "nasal passage") and the paranasal sinuses, more commonly known as simply "sinuses." The nasal cavity and the paranasal sinuses form a major portion of the bone skeleton of the face and the anterior or front part of the base of the skull. Four pairs of sinuses are located around the nasal passage and include:
- Maxillary sinuses, which are located to the side of the nose, within the cheek bone;
- Ethmoid sinuses, which are located between the nose and the eye;
- Frontal sinuses, which are located in the forehead; and
- Sphenoid sinuses, which are located deep behind the nose.
Nasopharynx: Behind the nasal cavity and above the soft palate (the back portion of the roof of the mouth) lies the nasopharynx. This is the top portion of the pharynx, which is the passageway that runs from behind the nose and mouth down to the esophagus. The nasopharynx sits right under the middle portion of the skull base.
Orbit: The orbit is the bony cavity that contains the eyeball. Tumors can start within the orbit (these are known as primary orbital tumors) or they can start in the sinuses and invade into the orbit. Tumors in the orbit present unique challenges, given the proximity to structures critical for visual function. Orbital tumors include vascular tumors of the orbit, primary lacrimal gland tumors and metastatic lesions to the orbit.
Parapharyngeal Space: To the side of the throat or pharynx is the parapharyngeal space. It contains the lowest four cranial nerves, which are involved with speech, swallowing and shoulder movement. It also contains the major blood vessels of the neck, such as the carotid artery and the jugular vein. The skull base forms the roof of the parapharyngeal space. The most common tumors in the parapharyngeal space are salivary gland tumors, paragangliomas (or vascular tumors) and tumors of the lower cranial nerves.
Cavernous Sinus: Below the brain and on either side of the pituitary gland and sella turcica lie the two cavernous sinuses. These sinuses contain blood and are part of the venous drainage of the brain. Important nerves run through the cavernous sinus, as do the internal carotid arteries. Cranial nerves III, IV, V and VI are located in this region.
Cerebellopontine Angle: The cerebellopontine angle is the area between the cerebellum (the portion of the brain that controls coordination of movement), the pons (part of the central nervous system's brainstem) and the temporal bone. This space contains several cranial nerves, including nerves designated as V through XII. Acoustic neuroma and meningioma are the most common tumors located at this site.
Cranial Nerves: Twelve pairs of nerves are located in the head and neck. These nerves are known by their anatomic names and by their Roman numeral designation. Tumors, usually benign neuromas, can arise from these nerves. Malignant tumors can involve these nerves and cause pain, numbness or paralysis. Care is taken during surgery to preserve the function of these nerves whenever possible.
Skull base tumor risk factors
Anything that increases your chance of getting a skull base tumor is a risk factor. Since skull base tumors are rare, risk factors are hard to determine. Skull base tumor risk factors include the following:
- Previous radiation treatment to the head and neck area as well as exposure to certain chemicals have been identified as risk factors for meningioma, some sarcomas and some sinonasal cancers.
- Exposure to wood dust, heavy metals and a history of working with leather are risk factors for developing some sinus and nose cancers.
- Certain types of nasopharyngeal cancers are related to childhood exposure to the Epstein-Barr virus.
- Certain inherited genetic conditions are linked to skull base tumors. In these cases, our genetics experts are part of the patient’s care team. The types of tumors that may be caused by genetic conditions include:
- Bilateral acoustic neuromas, as well as other brain and spine tumors, may be caused by the genetic disorder neurofibromatosis type 2.
- Paragangliomas (also called glomus tumors or carotid body tumors) may be caused by a familial predisposition for other tumors.
- Pituitary tumors may be associated with multiple endocrine neoplasia 1 (MEN1) or family isolated pituitary adenoma (FIPA) which may be familial and predispose to other tumors.
Not everyone with risk factors gets skull base tumors. However, if you have risk factors, it’s a good idea to discuss them with your doctor. Research shows that many cancers are curable when caught at an early stage.
Learn more about skull base tumors:
Some cases of skull base tumors can be passed down from one generation to the next. Genetic counseling may be right for you. Learn more about the risk to you and your family on our genetic testing page.
Why choose MD Anderson for your skull base tumor treatment?
At MD Anderson, physicians and specialists in the Skull Base Tumor Program treat patients with both cancerous and noncancerous tumors of the skull base.
MD Anderson's team approach to skull base tumor treatment brings together renowned experts from many specialties to give you comprehensive, personalized care.
A group of specialists meets regularly to discuss your needs and options. This exchange of ideas sets the stage for delivering the highest level of care for skull base tumors.
Our approach begins with your first visit and continues through diagnosis, treatment, rehabilitation and follow-up. Your team may include surgeons, radiation and medical oncologists, ophthalmologists, nutritionists, nurses, speech and language pathologists, audiologists, physical and occupational therapists, and social workers. They have access to the latest technology and techniques to diagnose and treat skull base tumors, including minimally invasive surgery, innovative radiation therapy and the most effective cancer drugs.
Surgical skill
Surgery is often part of the treatment for skull base tumors. Tumors located deep in the structures of the head present significant challenges because important nerves, blood vessels and brain structures may be involved.
Our surgeons have pioneered techniques and surgical approaches that allow for maximum safe removal of tumors in this delicate and complex area. They are experts in open and minimally invasive diagnostic and surgical approaches to skull base tumors.
Our surgeons are members of MD Anderson's Brain and Spine Center or Head and Neck Center. They work together closely and have extensive experience in skull base tumor procedures. They have been recognized in U.S. News & World Report's list of Best Doctors in America, and they are respected around the world.
Advanced radiation therapy
Our radiation oncologists are experts in the treatment of skull base tumors. They have pioneered the use of modern high-precision radiation therapy techniques that target radiation doses precisely to the shape of tumors. These treatments minimize side effects, damage to healthy tissue and long-term toxicity.
Radiation treatment for skull base tumors at MD Anderson can include specialized techniques. Among these are stereotactic radiosurgery, which delivers a powerful dose of treatment radiation in a single session; and proton therapy, a state-of-the-art treatment that is not widely available. There’s even a radiation clinic for patients with recurrent skull base tumors. These patients can benefit from our multidisciplinary team approach to managing complex cases.
Rehabilitation, symptom management, side effects and quality of life issues
Giving patients with skull base tumors the opportunity and the tools to enjoy life fully is an important part of care at MD Anderson. Skull base tumor patients may experience symptoms of tumors and side effects from treatment, like changes in hearing, vision, balance, smell, speech or memory. We understand that quality of life is an important consideration during cancer treatment and recovery.
Many patients can overcome limitations caused by skull base tumors or treatment effects with the help of care providers like audiologists, speech and language and swallowing therapists, behavioral psychologists, neuropsychologists, ophthalmologists, nutritionists, and occupational and physical therapists.
And, as one of the nation's leading cancer center, MD Anderson is able to offer a range of clinical trials of new treatments for skull base tumors.
Personalized treatment
Treatment for tumors of the skull base may involve surgery, radiation therapy, chemotherapy or a combination of therapies. Surgeons in the Skull Base Tumor Program use both open and minimally invasive diagnostic and surgical approaches, depending on each patient's unique characteristics. For patients with tumors that are responsive to irradiation, radiation oncologists plan three-dimensional treatment algorithms for the precise delivery of radiation therapy.
With MD Anderson's Proton Therapy Center, proton radiation therapy now provides an additional treatment option for patients with specific tumors that are well suited to this innovative, state-of-the-art therapy.
And, as one of the nation's leading cancer centers, MD Anderson is able to offer a range of clinical trials of new treatments for skull base tumors.
Every time I see beauty through my eyes, I am reminded of my miracle and how fortunate I was to be treated at MD Anderson.
Donis Lane
Survivor
Treatment at MD Anderson
Featured Articles

Olfactory neuroblastoma didn’t stop this survivor from achieving his goals

Cancer of the nose: Facts about nasal cavity and paranasal sinus cancer

Olfactory neuroblastoma survivor champions self-advocacy and integrative medicine

Basketball coach cancer-free after nasopharyngeal cancer treatment

Finding faith, hope and healing during sinonasal undifferentiated carcinoma treatment

Skull base tumor survivor: Writing music helped me cope with my pain

Skull base tumor survivor: MD Anderson’s expertise saved my life

Olfactory neuroblastoma survivor finds hope at MD Anderson
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients, family members and loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
