request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Myelodysplastic Syndrome
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsMyelodysplastic syndrome is a group of diseases in which the bone marrow doesn’t produce enough healthy blood cells. Instead, it makes too many immature cells, called blasts.
Myelodysplastic syndrome is a group of diseases in which the bone marrow doesn’t produce enough healthy blood cells. Instead, it makes too many immature cells, called blasts.
These blasts die in the marrow or soon after entering the bloodstream, resulting in too few healthy blood cells and low blood counts.
In its mildest form, MDS may be anemia, low platelets or low white blood count, but about 10% to 20% of diagnosed cases progress to acute myeloid leukemia (AML).
To better understand what happens to your blood when you have myelodysplastic syndrome, it helps to know what makes up normal blood and bone marrow.
There are three major types of blood cells: red blood cells (RBCs), white blood cells (WBCs) and platelets. These cells are made in the bone marrow and flow through the bloodstream in a liquid called plasma.
Red blood cells (RBCs), the major part of your blood, carry oxygen and carbon dioxide throughout your body. The percentage of RBCs in the blood is called hematocrit. The part of the RBC that carries oxygen is a protein called hemoglobin. All body tissues need oxygen to work properly. When the bone marrow is working normally, the RBC count remains stable. Anemia occurs when there are too few RBCs in the body. Symptoms of anemia include shortness of breath, weakness and fatigue.
White blood cells (WBCs) include several different types. Each has its own role in protecting the body from germs. The three major types are neutrophils, monocytes and lymphocytes.
- Neutrophils (also known as granulocytes or polys) destroy most bacteria.
- Monocytes destroy germs such as tuberculosis.
- Lymphocytes are responsible for destroying viruses and for overall management of the immune system. When lymphocytes see foreign material, they increase the body’s resistance to infection.
WBCs play a major role in fighting infection. Infections are more likely to occur when there are too few normal WBCs in the body.
Absolute neutrophil count (ANC) is a measure of the number of WBCs you have to fight infections. You can figure out your ANC by multiplying the total number of WBCs by the percentage of neutrophils (“neuts”). The K in the report means thousands. For example:
WBC = 1000 = 1.0K
Neuts = 50% (0.5)
1000 X 0.5 = 500 neutrophils
Also, when you receive your blood counts, this equation may be written as polys plus bands = neutrophils. Further, while anyone can catch a cold or other infections, this is more likely to occur when your ANC falls below 500. Your WBC count generally will fall within the first week you start chemotherapy, but it should be back to normal between 21 to 28 days after starting chemotherapy.
Platelets are the cells that help control bleeding. When you cut yourself, the platelets collect at the site of the injury and form a plug to stop the bleeding.
Bone marrow is the soft tissue within the bones where blood cells are made. The bone marrow is made up of blood cells at different stages of maturity. All blood cells begin in the bone marrow as stem cells. Stem cells are very immature cells. When there is a need, the stem cells are signaled to develop into mature RBCs, WBCs or platelets. This signaling is done with “growth factors.”
As each cell fully matures, it is released from the bone marrow to circulate in the bloodstream. The blood circulating outside of the bone marrow in the heart, veins and arteries is called peripheral blood.
Myelodysplastic syndrome types
There are several types of MDS, and they are classified based on the number of abnormal cells in the blood and bone marrow. Types of myelodysplastic syndrome include:
- Refractory anemia
- Refractory cytopenia with multilineage dysplasia
- Refractory anemia with ringed sideroblasts
- Refractory cytopenia with multilineage dysplasia and ringed sideroblasts
- Refractory anemia with excess blasts
Myelodysplastic syndrome risk factors
Anything that increases your chance of getting a disease is a risk factor. Most cases of myelodysplastic syndrome have no known cause, but some factors have been found to increase the risk.
Risk factors for myelodysplastic syndrome include:
- Age: MDS rarely occurs in people younger than 60
- Smoking tobacco
- Long-term exposure to chemicals, including benzene or other chemicals used in the petroleum and rubber industries
- Exposure to high levels of radiation, such a nuclear reactor accident or atomic bomb
- Prior chemotherapy or radiation therapy
- Inherited disorders, including:
- Fanconi anemia
- Shwachman-Diamond syndromes
- Familial platelet disorder
- Severe congenital neutropenia
Not everyone with risk factors gets MDS. However, if you have risk factors, it’s a good idea to discuss them with your health care provider.
Learn more about myelodysplastic syndrome:
- Myelodysplastic syndrome symptoms
- Myelodysplastic syndrome diagnosis
- Myelodysplastic syndrome treatment
Some cases of myelodysplastic syndrome can be passed down from one generation to the next. Genetic counseling may be right for you. Learn more about the risk to you and your family on our genetic testing page.
MD Anderson is #1 in Cancer Care

How a myelodysplastic syndrome survivor found strength
"It was like a dream come true," Rani says. "I felt like I was on the top of the world. I want to thank all my doctors, family, friends and the whole staff at MD Anderson. I felt an unbelievable sense of accomplishment."
Rani's MDS diagnosis
Rani first started experiencing MDS symptoms in September 1997, but she didn't think they were indicative of cancer.
Heavy periods lasting 10 to 12 days prompted her gynecologist to treat her for early menopause. She started a regimen of hormone pills, which stabilized her, but she became cripplingly ill a few months later. Multiple courses of antibiotics did nothing to allay the symptoms, and she began bruising excessively at the slightest bump. By March, it had become too much.
Rani's paper-white hands alarmed her doctor, and he ordered on-the-spot blood tests. She was diagnosed with a type of MDS. After several recommendations from friends, she and Tej decided to come to MD Anderson for a second opinion.
"If there was one place where this could have been conquered, it was MD Anderson," Tej says.
Rani began her MDS treatment here in late March. She began chemotherapy, but after several treatments, her cancer still persisted.
She decided to undergo an allogeneic stem cell transplant. Three of her sisters were matches, and her youngest sister provided the stem cells that would save Rani's life. After her stem cell transplant, she was cancer-free.
Finding optimism during MDS treatment
Rani and Tej fell apart when they received her MDS diagnosis.
"When I first heard, I thought she was going to die," Tej says. "I thought I was going to lose her."
Even through 21 days of isolation during her stem cell transplant, she made the conscious decision to stay positive. She drew inspiration from her family and was proud to say she was fighting cancer.
"I'd rather laugh and not cry," Rani says. "I choose to laugh in tough times."
Now, nearly 16 years after her MDS treatment, she uses that positive energy to conquer new obstacles.
The ride of a lifetime
Rani has always been active, but wasn't sure her gym routine would be enough to propel her and Tej -- who had participated in four previous MS 150s -- on a bike ride that is longer than many of the stages in the Tour de France.
Rani and Tej began routinely riding 20 to 30 miles around their neighborhood and used visits to see their son in San Antonio as a way to get in some much-needed hill training. Still, they weren't sure they'd actually go through with something that would be grueling for any athlete.
As the two drew near the finish line, they were overcome with emotion. Thoughts turned to Rani's cancer, her treatment and how fortunate they were to be able to ride together all these years later.
"At that moment I felt, 'She is absolutely as normal as every other human being,'" Tej says. And although it was her legs that pushed her past the finish line, she knew it was a team effort -- 16 years in the making.

How a clinical trial gave me my life back after MDS and AML
Five years ago, my spouse and I had settled into our dreamed-of retirement. Although our 28 years as professors at the University of Arizona were rich and rewarding, retirement was much better.
But on Feb. 6, 2012, I was diagnosed with myelodysplastic syndrome (MDS), a rare blood cancer.
Because I was in my early 70s, a bone marrow transplant wasn’t my best option. Instead, I received chemo infusions for seven days every 28 days to improve my bone marrow and blood cell function.
But after nearly 3 1/2 years of this, I learned the chemo was no longer working.
A subsequent bone marrow biopsy demonstrated progression of my MDS, with the identification of an IDH1 mutation.
I sought a second opinion and got a grim prognosis. The oncologist gave me only five to seven months to live. He said I needed to find a clinical trial soon.
Choosing a clinical trial at MD Anderson
During my search, I learned about a Phase II clinical trial at MD Anderson using an experimental drug called AG120. About a week after I applied, Courtney DiNardo, M.D., asked me to travel from my home in Tucson for testing.
Between MD Anderson’s huge campus and the battery of medical tests, our first visit was overwhelming. Yet, when Dr. DiNardo entered the room, she immediately made us feel like we were long-time patients or even friends. She was so cool, young and confident.
Only 24 hours after my spouse and I returned home, Dr. DiNardo called and asked us to return right away. We canceled our holiday plans, packed our motorcoach and arrived in Houston on Dec. 12, 2015.
At MD Anderson, we learned that my MDS had progressed to acute myeloid leukemia (AML). This was shocking, but I felt a strong sense of hope. We were right where we needed to be. People come to MD Anderson from all over the world, and I was grateful to be there with so many other AML patients.
On December 23, I took my first pills for the clinical trial. Then came endless EKGs and every-other-day blood tests to check my blood cell counts.
My amazing AG120 results
Two weeks into the clinical trial, my white cell count was higher than it had been in two years. My spouse and I were amazed.
But the biggest surprise was my blast count. When I’d arrived at MD Anderson, it was at 30% — extremely high. At the end of the first 28-day cycle, it was just 2%, which is normal.
Unlike chemo, which tries to kill the blasts and everything else in the bone marrow, AG120 blocks the mutant IDH1 protein that caused my AML. It allows the blasts to mature properly into normal white cells of the immune system. The bone marrow is no longer crowded out by AML, and the normal red cells and platelets return, too.
I’m now beginning my 12th cycle of AG120, and my blood values, red blood cells, white blood cells and platelets have all reached normal range. I’m in complete remission, but I will continue to take AG120 indefinitely. Whenever Dr. DiNardo’s team asks about side effects, I can’t come up with anything.
‘A small price to pay’
I am so grateful and praise God every day for giving me my life back through the AG120 clinical trial.
I used to always say you have to be your own advocate because no one else will. But I was unable to take charge of my cancer until I met Dr. DiNardo. I’ll always remember what she said the day before I enrolled in the clinical trial: “You are in the right place at the right time with the right mutation.”
She was absolutely right. And the ongoing research that Dr. DiNardo is doing as part of MD Anderson’s MDS/AML Moon Shot is helping to ensure other patients will have this same opportunity.
I still fly back to Houston every 28 days to receive my next cycle of pills. But when the FDA approves AG120, I’ll be able to fill my prescription at my local pharmacy. Until then, returning to Houston is a small price to pay for getting my life back.

My new normal: Life after myelodysplastic syndrome
My friend, Julie, a cord blood transplant survivor, wrote me a sweet note a few weeks ago. She mentioned that she was trying to find her "new normal."
As a stem cell transplant survivor, I've recently been thinking a lot about it myself, and struggling.
I catch myself saying, "Whenever I'm off my immune suppressant drug, sirolimus, I can do such and such," And then, "What if that never happens?"
I had to take off my rose-colored glasses and realize that "normal" will never be the same as it was before cancer.
This doesn't mean it's bad. It just means my life is different.
I think it's impossible to go through cancer without being changed.
In early December, I got sick with a sore throat. It was the first time I'd been sick since my transplant at MD Anderson a year-and-a-half ago.
I now understand why we must go through all the things we do to prevent getting sick after a transplant.
Without much of an immune system, I became very ill quickly and had to be hospitalized.
It took a month for me to get well, which made me realize the importance of compliance with my doctor's orders.
As time goes on, carelessness can creep in.
I now realize the importance of all the things my survivorship nurse at MD Anderson taught me.
I'm really good at hand washing and sanitizing, and staying away from people who are sick. But I also realized I must live like a healthy, normal person instead of staying cooped up at home afraid of getting sick.
Coming to terms with my new normal
A few months ago, I tried to get off of sirolimus, with permission from my doctor Chitra Hosing, M.D.
It didn't work.
It only took a week for me to have symptoms of Graft vs. Host Disease (GVHD), and much, much longer than that to get back to where I was.
Actually, I still don't feel like I'm doing as well as I was before trying to get off of sirolimus.
This brings me back to my new normal.
I can honestly say that the things I occasionally gripe about -- taking a lot of medicine, chemo fried hair, tiredness, frequent blood tests, feeling isolated and lots of other "stuff" -- are really not all that bad.
In fact, I'm proud of where I've been and where I am now in this journey.
It's just a matter of acceptance and compliance. And, remembering all of the many wonderful blessings and friendships that have been given me.
The positive things far outweigh the negative.
So, here's my advice. Find your new normal, follow the instructions of your health care team, live life to the fullest and accept the beauty and wonderfulness of being given a second chance.
Holly Easley began her cancer journey five years ago when she was diagnosed with myelodysplastic syndrome (MDS). After two types of chemotherapy and a stem cell transplant, she loves life, is improving daily and enjoys blogging about her cancer experience.
Why come to MD Anderson for myelodysplastic syndrome treatment?
About 300 people with myelodysplastic syndrome (MDS) are evaluated in MD Anderson's Leukemia Center each year, making our program one of the most active in the nation.
A team of some of the world's most renowned experts works together to give you personalized care, communicating closely with you and each other at every step. Your care team draws from a full range of the latest, most advanced treatments for myelodysplastic syndrome. Since long-term follow up care often is needed, we maintain a close relationship with your referring physician.
And at MD Anderson you're surrounded by the strength of one of the nation's largest and most experienced comprehensive cancer centers, which has all the support and wellness services needed to treat the whole person – not just the disease.
Pioneering advancements
Over the past few years, the care of patients with MDS and the understanding of this disease have improved significantly. This has resulted in the development of new therapies, many of which were studied extensively at MD Anderson, including decitabine (Dacogen®) and azacitidine (Vidaza®), which now are considered standard of care. Our researchers also have been instrumental in finding out how the disease begins on a molecular basis and how to determine potential outlooks.
At MD Anderson's Leukemia Center, you benefit from one of the most active research programs in the United States. This means we are able to offer a range of clinical trials (research studies) of new treatments for myelodysplastic syndrome.
MD Anderson is a big organization, but it’s welcoming and it makes you feel safe.
Sandy Bobet
Caregiver
Treatment at MD Anderson

Myelodysplastic syndrome researcher: Leaps of faith led to my career at MD Anderson
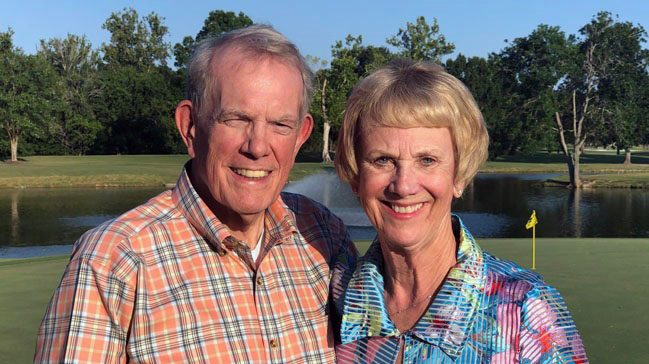
In sickness and in health: Husband and wife face back-to-back cancer diagnoses

Myelodysplastic syndrome survivor: Why I joined a clinical trial

Myelodysplastic syndrome survivor: A targeted therapy clinical trial put me in remission
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be
found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
