request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Childhood Liver Cancer
- Childhood Liver Cancer Treatment
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsChildhood Liver Cancer Treatment
Your child’s treatment will be carefully planned by a team of doctors. They will talk to you about the best treatment for the cancer. This may depend on:
- If the tumor can be removed completely by surgery
- What type of cells are in the tumor
- If the cancer has spread
- The level of alphafetoprotein (AFP) in the tumor
Hepatoblastoma and hepatocellular carcinoma are treated differently. Both require complete surgical removal for treatment to be successful. Hepatoblastoma responds well to chemotherapy, but hepatocellular carcinoma tumors are usually treated with surgery alone.
Surgery
Surgery is almost always part of the treatment for pediatric liver cancer. If all or most of the cancer can be surgically removed, the possibility of successful treatment is better.
Unfortunately, the surgeon may not be able to remove all of the tumor if it is large or has spread to other parts of the liver or the body. If this is the case, the surgeon will remove as much of the tumor as possible while keeping enough of the liver to function.
Since the liver helps with blood clotting, bleeding after surgery may be a problem. And, since the remaining liver still is damaged, the cancer may come back.
The main types of surgery for liver cancer are:
- Liver transplant: After the liver is surgically removed, it is replaced by a healthy donor organ. Liver transplant has a risk of serious infection and other health issues.
- Partial hepatectomy: The part of the liver where the tumor is located is removed surgically
- Tumor ablation: Heat (radiofrequency ablation) or extreme cold (cryosurgery or cryotherapy) is used to freeze or burn away the liver cancer. Ablation may be used when surgical removal of the tumor is not possible.
Embolization
Tiny pellets of plastic or another material are injected into the arteries that carry blood to the tumor. The pellets block blood flow, which makes it harder for liver cancer to grow.
Radiation therapy
Because radiation may destroy normal liver tissue as well as cancer cells, it can be used only in low doses for liver cancer. Radiation therapy cannot cure liver cancer, but it may be used to shrink the tumor or relieve pain.
New radiation therapy techniques and remarkable skill allow MD Anderson doctors to target tumors more precisely, delivering the maximum amount of radiation with the least damage to healthy cells.
Proton therapy
The Proton Therapy Center at MD Anderson is one of the largest and most advanced centers in the world. It’s the only proton therapy facility in the country located within a comprehensive cancer center. This means this cutting-edge therapy is backed by all the expertise and compassionate care for which MD Anderson is famous.
Proton therapy delivers high radiation doses directly to the liver cancer tumor site, with minimal damage to nearby healthy tissue. For some patients, this therapy results in a higher chance for successful treatment with less impact on the body.
Chemotherapy
Chemotherapy is often used to treat hepatoblastoma, but hepatocellular cancer doesn’t respond to it. Our experts also are working on new ways to give chemotherapy drugs directly into the liver, delivering higher doses of drugs than usually possible with fewer side effects. These include:
- Chemoembolization: A needle is inserted into an artery in the groin, and then a tiny tube is threaded into an artery leading to the liver. A high dose of medicine then is given. Afterward, the artery is blocked to prevent it from feeding blood to the liver.
- Hepatic artery infusion: A catheter (tube) is placed in the liver. Drugs are infused into a special implanted pump that delivers them continuously.
Targeted therapies
Children’s Cancer Hospital is among just a few cancer centers in the nation that are able to offer targeted therapies for some types of pediatric liver cancer. These innovative new drugs stop the growth of cancer cells by interfering with proteins and receptors or blood vessels that supply the tumor with what it needs to grow.
Learn more about childhood liver cancer:
Learn more about clinical trials for childhood liver cancer.

Liver regeneration: How the liver’s ability to recover plays into liver cancer surgery
Did you know that the liver is the only internal organ that can regenerate? But it doesn’t grow back like a salamander’s tail. When a portion of the liver is removed, the remaining tissue grows bigger. This process is called hypertrophy.
We spoke with surgical oncologist Ching-Wei Tzeng, M.D., to learn what’s happening when a liver regenerates and what factors can impact success. He shared insights on the phenomenon, including how his team is pioneering a care approach in the United States that anticipates the liver’s ability to bounce back to yield the best results possible for patients with liver cancer.
Let’s start with the basics. What does the liver do?
The liver plays three main roles: It serves as a protein factory, a blood filter and a metabolic processor.
The liver produces important proteins that work to balance the thickness of your blood. If the liver isn’t functioning properly, such as from not getting the right nutrients or because of damage like cirrhosis or surgery, your blood may become too thin. With thin blood, you’re more likely to bruise and/or bleed from something as simple as brushing your teeth or shaving.
You can also think of the liver as a water filter. It cleans the huge volume of blood that flows from the gastrointestinal tract back to the heart. If the liver is damaged, fluid can get backed up and lead to a bloated belly.
Lastly, the liver supports metabolic processing. It creates bile that aids food digestion and that helps the body absorb medication.
We often associate liver dysfunction with yellow skin, but that’s not always the case. If one or all of these functions aren’t fulfilled, it’s considered liver failure. And it’s not always apparent by a person’s outward appearance.
What’s happening when the liver regenerates?
Anytime the blood flow is reduced to one part of the liver, the liver will compensate and get bigger if the remaining part is healthy. The cells that grow bigger or hypertrophy are immature, so they don’t have the full function of the mature liver cells yet. But over time – in many cases, in just a few days – they mature and work just as well as the cells that were removed.
Many patients who receive liver cancer surgery see that their remaining liver tissue grows to be almost as big as what was removed only a month after surgery. We see this in patients who have even up to 50% of their liver removed.
We use a test that measures bilirubin levels to help track the function of the liver. When the liver isn’t working properly, bile builds up, and the bilirubin level increases. Once we see that number peak and then start to drop, we know the liver is fine.
We find that for most patients, the liver performs just as well after surgery. It’s as if we didn’t do the surgery. It’s pretty amazing how the liver can bounce back in such a short time.
How does liver regeneration play into the development of a cancer treatment plan?
When planning treatment, we count on the liver to regrow after surgery. With surgery to the lungs, kidney, pancreas, stomach or intestines, we think very carefully about how much tissue we remove because these organs can’t regenerate. There’s no going back.
With liver surgery, we are still very careful, but we plan for some growth to make up for what we remove. We formulate a plan specific to each patient to remove the necessary portions of the liver while leaving a minimum total 30% to grow back. We calculate that using a computer software that measures the size of the liver in relation to a patient’s body size.
We are also careful to remove only what is necessary. That's important for patients’ quality of life. Also, if the liver cancer comes back, we want to ensure a patient has plenty of liver to take more chemotherapy, if necessary, or even have surgery again. We're not just getting rid of cancer today. We're trying to set up patients to be strong should they ever face a diagnosis again.
What research is being done surrounding liver regeneration and cancer?
For the past two decades, MD Anderson has been the leading group in the United States to study preoperative portal vein embolization (commonly referred to as PVE) to grow the liver before surgery. The approach was originally developed in Japan.
About a month before surgery, we deliver small particles to the portion of the liver that we plan to remove to block the blood flow. It helps to redirect the blood to the healthy portion of the liver, which can help it grow ahead of surgery. By growing the healthy portion of the liver, we can hit the 30% mark. It’s amazing because we’re able to offer life-saving liver surgery to patients who previously weren’t eligible.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Treatment at MD Anderson
Childhood liver cancer is treated in our Children's Cancer Hospital.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.

Uterine leiomyoma patient: An embolization procedure at MD Anderson changed my life
I was diagnosed with an extremely rare myeloproliferative disorder called Rosai-Dorfman disease in 2014. It’s not fatal, but it does cause severely swollen lymph nodes and other benign growths sometimes. I’ve had several growths removed already, including one from my neck and another from my upper back.
I’m very grateful to MD Anderson thoracic surgeon Dr. Garrett Walsh for performing those surgeries. But it’s the uterine fibroid embolization procedure I had at MD Anderson last fall that completely transformed my life.
My uterine leiomyoma symptoms
I’ve had terrible menstrual periods since I was a teenager. Even back then, I was passing large blood clots during almost every cycle. It got so bad that my friends and family would look at me sideways sometimes and ask if I was having a miscarriage instead of just a regular period.
Then, around 2019, my cycles got even worse. My flow had always been very heavy, but at some point, I realized I was going through two cases of sanitary pads a month. I’d also developed severe anemia and was losing so much blood that my normally brown skin looked gray.
My uterine leiomyoma diagnosis
I went to five different gynecologists. None of them could help me. I was getting really depressed.
Then, last September, I happened to mention my problem to Dr. Walsh during one of my routine check-ups. He referred me to gynecologist Dr. Elizabeth Keeler. She ordered a pelvic ultrasound. That scan revealed I had multiple benign fibroids — also called uterine leiomyoma — in my uterus. One was roughly the size of a lemon.
Fibroids — especially large ones — can cause exactly the type of problems I’d been having. So, Dr. Keeler recommended medication to reduce the bleeding and referred me to interventional radiologist Dr. Joshua Kuban for a consultation to discuss a procedure called uterine fibroid embolization (UFE).
MD Anderson treats the whole person
I was so relieved to finally have doctors who listened to and believed me that I just started crying. Dr. Keeler reassured me that I wasn’t crazy and it wasn’t all in my head. To me, that speaks volumes about how MD Anderson treats its patients — we’re seen as whole people, not just our diseases.
Uterine fibroids aren’t the same thing as uterine cancer. They’re not even malignant. They’re also not related to Rosai-Dorfman disease. I didn’t know I had them until I got the ultrasound results. But when I told my MD Anderson doctors about my related problems, they took me very seriously. I felt both safe and heard.
My uterine leiomyoma treatment
I met with Dr. Kuban to discuss the embolization. He told me that the arteries feeding the fibroids would not be removed or destroyed. Instead, they would be permanently blocked using tiny particles administered through a small catheter inserted into my wrist. Cutting off the fibroids’ blood supply would hopefully shrink them, which in turn would reduce my menstrual flow.
All of that sounded really good to me. So, Dr. Kuban performed the embolization on Nov. 16, 2022. My life has completely turned around since then.
Before that procedure, I was virtually housebound whenever I was on my period. Now, I can go to the grocery store without worrying about whether I’m going to bleed through my clothes or ruin anyone’s upholstery. I even participated in a 5K fun run for the first time this past February.
The only side effect I’ve experienced so far is a good one: I’ve had to relearn my body’s signals. One of the biggest fibroids was pressing against my bladder for so long that it distorted my perception of when I needed to urinate. Since then, I feel like my life has been given back to me in every way.
Why I’m spreading the word now
I know in my heart that I’m not the only woman going through this. That’s why I’m on a mission now to share my story.
Because so many other women are enduring the same kind of bleeding and cramping I did, day after day. How many of them will just keep right on suffering because they stopped asking for help after Doctor #1 or #2 couldn’t find a solution?
The type of care I received at MD Anderson should be the type of care every woman receives, simply because she says, “Something’s not right here.” And Dr. Kuban and Dr. Keeler did more for me in two months than my previous five gynecologists did over three years.
That’s why I’m sharing my story today: because no woman should ever have to go through what I did. And if I can save just one of them from the embarrassment of having messed up their clothing or car seats, then my experience will have been worth it.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention and Screening
Many cancers can be prevented with lifestyle changes and regular screening.
What’s new in treating hepatocellular carcinoma, the most common liver cancer?
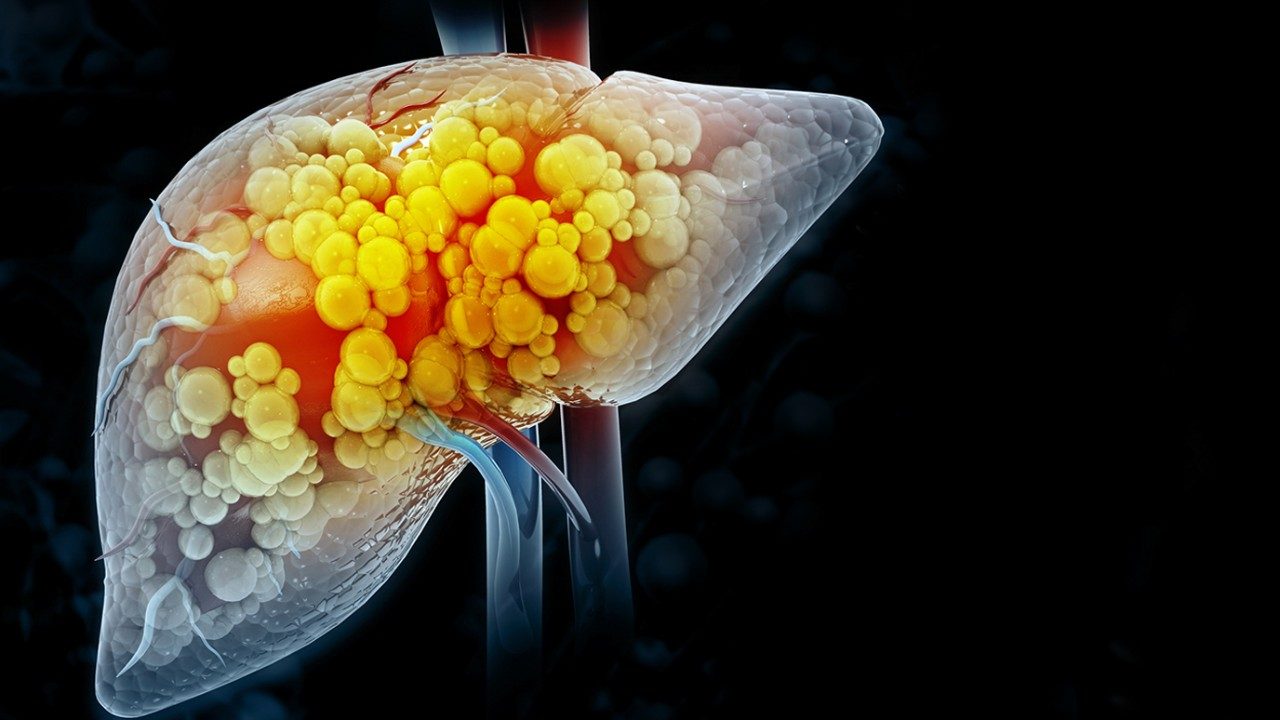
Liver cancer is one of the most quickly increasing types of cancer in the United States due to a poor lifestyle causing obesity, diabetes, high cholesterol and high blood pressure. Once mostly seen in older adults and patients with hepatitis, it is now seen in younger patients and those without hepatitis.
Cancers that begin in the liver are called primary liver cancers. They are named after the types of cells where the cancer begins. Hepatocellular carcinoma is the most common type of primary liver cancer. This tumor begins in the liver’s hepatocyte cells when the cells divide uncontrollably.
Hepatocellular carcinoma is related to underlying chronic liver disease caused by:
- hepatitis B or C
- alcohol use
- fatty liver or metabolic syndrome
Since hepatocellular carcinoma is diagnosed in people with existing liver disease, only 15% to 20% of patients can receive surgery or a liver transplant. But more than 70% of people with hepatocellular carcinoma may have cancer return after surgery, which is associated with a poorer prognosis and shorter survival.
Thanks to new research, there is good news in the treatment of hepatocellular carcinoma. To learn more, we spoke with liver cancer expert Ahmed Kaseb, M.D.
What are the important features of hepatocellular carcinoma?
Hepatocellular carcinoma tumors have a lot of immune cells in the tumor. These immune cells are not active, but treatment with immunotherapy can activate them against the tumor.
Hepatocellular carcinoma tumors are also very vascular tumors. This means they form from blood vessels that grow abnormally. Vascular endothelial growth factor (VEGF) is a signal protein produced by many cells that causes the formation of blood vessels and changes the number and type of immune system cells in and around tumors. The overexpression of VEGF has been seen in hepatocellular carcinoma tumors.
How has hepatocellular carcinoma historically been treated?
One of the first treatments for treating advanced hepatocellular carcinoma was a targeted therapy drug called sorafenib. It targets the VEGF receptor by blocking the growth of blood vessels and cancer cells.
In 2007, sorafenib became the first drug approved by the Food and Drug Administration (FDA) to treat some patients with hepatocellular carcinoma. This drug helped stabilize the tumors, but it only extended patients’ lives by a few months
For the next decade, studies of other treatments showed little progress and were not shown to be better than sorafenib. Between 2017 and 2020, there were a handful of positive trial results.
How did the IMBrave150 clinical trial change hepatocellular carcinoma treatment?
The IMBrave150 Phase III clinical trial combined an immune checkpoint inhibitor called atezolizumab with bevacizumab, a targeted anti-EGFR therapy that starves tumors by preventing new blood vessels from growing. When compared to sorafenib, it showed that patients whose hepatocellular carcinoma was unable to be surgically removed and that was treated with atezolizumab and bevacizumab lived longer than those treated with sorafenib.
On May 29, 2020, the FDA approved this drug combination for people with liver cancer that has spread or that can’t be treated with surgery based on the study results.
What is the IMbrave050 clinical trial?
At the 2023 American Association of Cancer Research (AACR) Annual Meeting, IMbrave investigators will share preliminary results from the IMbrave050 trial. As one of the trial’s global investigators, I worked with an MD Anderson team to develop the study design and biomarker strategy. Based on the antitumor activity seen in the earlier clinical trial, the study evaluated the same drug combination in delaying or preventing cancer returning in patients with high-risk hepatocellular carcinoma after surgery. After surgery, patients either received the drug combination or were monitored through active surveillance.
The results show that atezolizumab plus bevacizumab is the first treatment given after surgery to demonstrate that patients lived longer without their cancer returning compared to those in active surveillance.
Why are these clinical trial results important for the future of hepatocellular carcinoma treatment?
These trial results indicate that this drug combination given after surgery has the potential to set a new standard of care for hepatocellular carcinoma treatment. We will continue to monitor these patients and provide long-term results, but this is a major step for patients with hepatocellular carcinoma.
Is there anything that newly diagnosed patients should know about hepatocellular carcinoma?
One of the major challenges to managing this disease is that patients with advanced disease cannot have surgery. If you have one of the risk factors for this disease, talk to your doctor about screening strategies. National guidelines recommend a blood test and an ultrasound every six months.
This is not a common cancer and needs to be treated by an expert. If you are diagnosed with hepatocellular carcinoma, you need to be treated by a multidisciplinary team like we have here at MD Anderson. That way, your care team can provide a personalized treatment strategy and offer clinical trials for liver cancer to give you the best chance for successful treatment.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
