request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Testicular Cancer
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsTesticular cancer occurs when cells in the testicles grow and multiply uncontrollably, damaging surrounding tissue and interfering with the normal function of the testicle. If the disease spreads, it is still called testicular cancer.
Testicular cancer occurs when cells in the testicles grow and multiply uncontrollably, damaging surrounding tissue and interfering with the normal function of the testicle. If the disease spreads, it is still called testicular cancer.
The testicles (also called testes) are a pair of male sex glands that are in a sac-like pouch (the scrotum) under the penis. They produce and store sperm and also are the body’s main source of male hormones. These hormones control the development of the reproductive organs and male characteristics.
Testicular cancer occurs most often in younger men. It is the most-often diagnosed cancer in men between ages 20 and 34. However, it accounts for only 1% of all cancers that occur in men. When testicular cancer is detected early, there is a nearly 99% chance for successful treatment. Approximately 9,300 new cases of testicular cancer are diagnosed each year. The disease's five-year survival rate is more than 95%
Testicular Cancer Types
There are two basic types of testicular cancer, each with subtypes:
Germ cell tumors occur in the cells that produce sperm. Tumor types include:
- Seminomas, the type found most often, are responsible for half of testicular cancer cases. They are generally slow growing and responsive to treatment.
- Nonseminomas tend to grow and spread faster than seminomas. Tumor types include:
- Embryonal carcinoma (about 20% of testicular cancers)
- Yolk sac carcinoma (most often occurs in infants and young boys)
- Choriocarcinoma, a rare and extremely aggressive cancer
- Teratomas
Stromal tumors occur in the testicular tissue where hormones are produced. Stromal tumor types include:
- Leydig cell tumors, which occur in cells that produce male sex hormones
- Sertoli cell tumors, which occur in cells that nourish germ cells
Testicular Cancer Risk Factors
Anything that increases your chance of getting testicular cancer is a risk factor. These include:
- Age: Most cases occur between the ages of 15 and 40, and testicular cancer is the type of cancer found most often in men ages 20 to 34.
- Race: White men are five to 10 times more likely to develop testicular cancer than men of other races.
- Family or personal history of testicular cancer
- Undescended testicle (cryptorchidism): Men with testicles that did not move down into the scrotum before birth are at increased risk. Men who had surgery to correct this condition are still at high risk of testicular cancer.
- Abnormal testicular development
- Klinefelter's syndrome: A sex chromosome disorder characterized by low levels of male hormones, sterility, breast enlargement, and small testes
- Human immunodeficiency virus (HIV) or AIDS
- Previous treatment for testicular cancer
Not everyone with risk factors gets testicular cancer. However, if you have risk factors, it’s a good idea to discuss them with your doctor.
Research shows that many cancers can be prevented.
Learn more about testicular cancer:
In rare cases, testicular cancer can be passed down from one generation to the next. Genetic counseling may be right for you. Visit our genetic testing page to learn more.
MD Anderson is #1 in Cancer Care
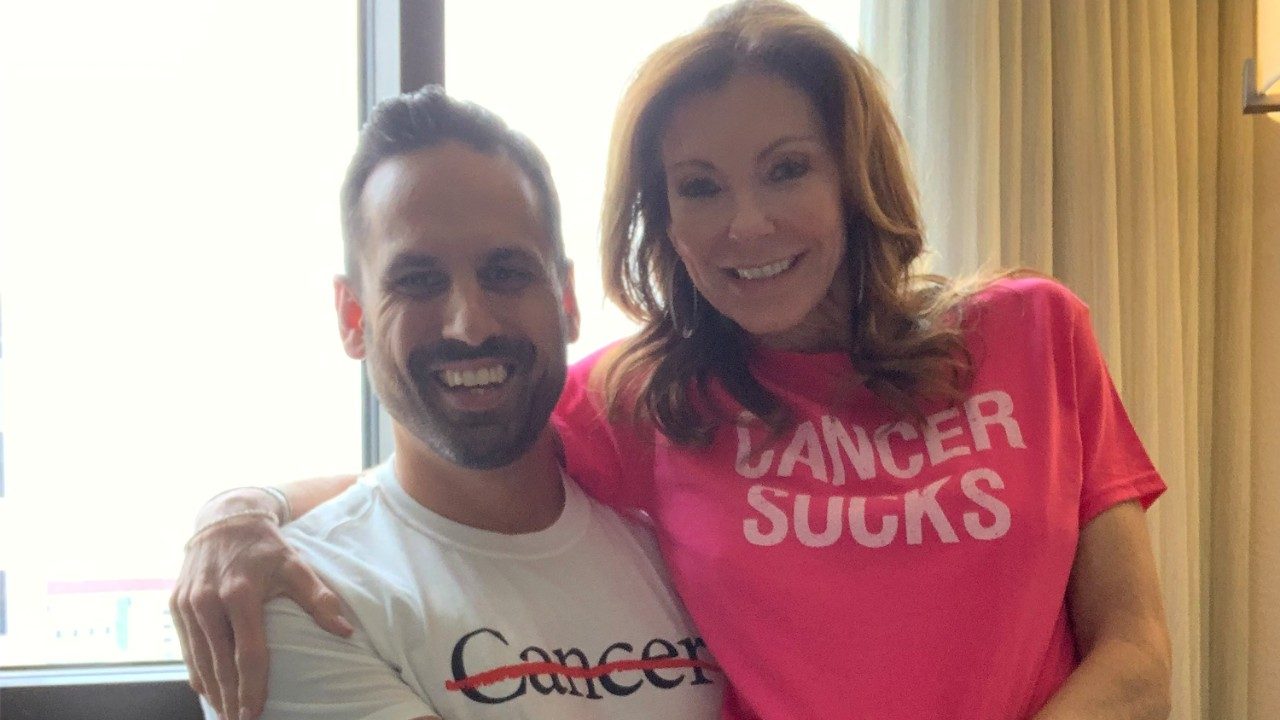
Testicular cancer survivor: Renewed perspective helped me heal
I was blindsided by my stage I testicular cancer diagnosis at age 42. It was the fall of 2020, and I had just moved to a new city, started a new career and, along with everyone else, was dealing with the day-to-day challenges of the COVID-19 pandemic.
Once I digested the news, my fiancée and I determined that going to MD Anderson was the obvious choice. Although I had never dealt with cancer, it didn’t take much digging to uncover MD Anderson’s No. 1 reputation in the field.
My testicular cancer treatment
Matthew Campbell, M.D., oversaw my treatment, which included an orchiectomy performed by Jose Karam, M.D., in November 2020. Dr. Campbell, along with the rest of my MD Anderson team, provided exceptional care. Not only did they heal my body, but they shepherded me through the mental challenges of dealing with cancer.
After weighing additional options after I’d recovered from surgery, Dr. Campbell, Dr. Karam and I decided active surveillance would be safer and more beneficial than chemotherapy or radiation therapy. I got the all-clear about a year later and am now celebrating more than two years cancer-free.
Testicular cancer gave me a new perspective
Before my testicular cancer diagnosis, I spent much of my time building, growing and chasing. But after my recovery, my focus shifted from the pursuit of happiness to finding happiness in the pursuit. Cancer gave me an opportunity to reflect on who I want to be and how I want to approach life.
I don't know if the cancer will appear again, but I know this: I've shifted my focus from survival to a thriving mindset. Now, I’m in the giveback stage – and let me tell you, that’s where the really good stuff is. The giveback stage is where you get to make an impact on other people's lives. You get to apply the lessons you've learned.
Gratitude turned to motivation
As I approached two years cancer-free, I returned to endurance training to improve my health. I was starting to feel better than I had in a while. It had been 10 years since I participated in a half-IRONMAN triathlon, but I wanted to participate in one again. I found an IRONMAN 70.3 event in Jones Beach, New York. It felt like kismet since the race was happening around the time of my two-year anniversary and was the closest IRONMAN 70.3 race to the town where I grew up.
But just doing the race didn’t seem like enough. I reached out to Dr. Campbell and told him I wanted to raise funds to support others dealing with cancer, but that I had no idea where to start. He put me in touch with MD Anderson’s Philanthropy team, and they set me up with a personal fundraising page. They explained that 100% of the funds raised would support Dr. Campbell’s testicular cancer research and directly help others.
Once I started fundraising, I decided to share my story more publicly via email and social media. My friends and family responded with an outpouring of financial and emotional encouragement, and my colleagues, former colleagues and distant friends did the same.
Sharing my journey also gave others permission to be open about theirs. Others reached out with stories of how cancer had touched them or their loved ones. I heard stories of perseverance, challenges and loss. They made me even more grateful for where I was, the gifts that had been bestowed upon me and the new perspective I had gained.
The night before the race, a friend reminded me that these stories would push me forward. He told me not to focus on my race time, but rather on showing up for those people in a way that honored their trust in me. I carried that motivation with me.
Persevering with purpose
On race day, Tropical Storm Ophelia hit the East Coast. It was raining sideways with temperatures in the low 50s. And if that didn’t present enough of a challenge, I broke my right clavicle in a bike accident around mile 20!
I told myself that while I might not finish the race, I could finish the next mile, then the next. As I carried on, the pain I felt was overshadowed by one thought — I had gotten exactly what I asked the universe for. To me, there was no better way to honor all those who’d supported me than by persevering through adversity.
All those who shared their stories gave me such a purpose. They made my decision to continue the race easy, despite the physical pain.
Crossing that finish line was a very emotional experience. At some point, we are all going to be tested. Some of us put ourselves in a position where we are asking to be tested, and some of us have no control over when those moments arise. All we really can control is how we are going to show up.
In those moments when you feel the world is against you and everything may seem to be working against you, try to remember that you do have a choice, even if it’s just to see things through a different lens. When you allow yourself to do so and couple it with a purpose bigger than yourself, you might accomplish something you didn’t think was possible.
Gratitude for those who got me here
None of this would have been possible without the support, guidance and love of my fiancée, Charlotte. She was there for me during the darkest days of my diagnosis and showered me with love and support during times of triumph.
Thanks to the incredible support from my family, friends, acquaintances and even strangers, we raised more than $160,000 for Dr. Campbell’s testicular cancer research. I wasn't expecting to raise this much, but I am so grateful that, together, we can help make someone else’s journey a little bit easier.
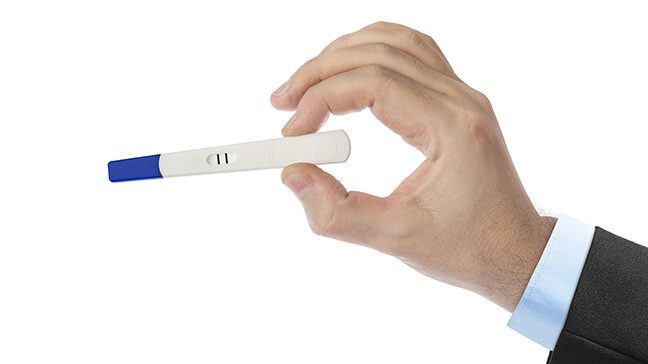
Can a pregnancy test predict testicular cancer?
A social media post about a man’s positive pregnancy test reportedly led to his testicular cancer diagnosis.
The man jokingly took the test which an ex-girlfriend had left behind in his medicine cabinet. He shared the surprising “positive” result with a friend, who shared the news on social media, carefully shielding the test-taker’s name to protect his privacy. The post quickly went viral and drew more than 1,600 comments.
“If this is true, you should check yourself for testicular cancer. Seriously. Google it,” read one of the comments.
A trip to the doctor revealed the male pregnancy-test-taker did, in fact, have testicular cancer.
Not all testicular cancers are alike
Pregnancy tests work by detecting human chorionic gonadotropin (HCG), a hormone in the blood and urine produced by the developing placenta.
It turns out that some types of testicular cancer make the same hormone.
So, is it worth running out to buy a pregnancy test to check for testicular cancer?
“There’s no advantage to relying on a pregnancy test to self-diagnose testicular cancer. It’s even dangerous to do so,” says urologist Christopher Wood, M.D. “Some forms of testicular cancer cause elevated HCG levels, but others don’t. Someone could get false reassurance from a negative test or could have elevated HCG levels for another reason altogether.”
Instead, Wood says men should see a doctor if they notice testicular cancer symptoms or unusual changes, including a lump or enlargement in either testicle, a sensation of heaviness in the scrotum, or a sharp pain or discomfort in the scrotum or testicle.
He recommends performing a self-exam in the shower once a month, starting in puberty.
“Testicular cancer manifests itself most commonly as a painless scrotal mass,” Wood says, “so check yourself, know your body and see a doctor if you detect anything suspicious.”
Testicular cancer risk factors
Compared to other types of cancer, testicular cancer is rare, accounting for just 1% of all cancers that occur in men. Yet it’s the most common cancer in males ages 15 to 35.
“This is a disease of the young,” Wood explains. “The typical patient is in his 20s or 30s, though we’ve seen patients as young as 15 and as old as 55.”
The disease occurs when cells in the testicles grow and multiply out of control, causing tissue damage and disrupting the normal function of the testicle.
The exact causes of testicular cancer are unknown, but a number of factors have been identified that increase a man’s risk of developing the disease, including undescended testicles at birth, a family history of testicular cancer, or a previous testicular cancer diagnosis.
How is testicular cancer diagnosed?
A scrotal ultrasound is usually the first step in diagnosing testicular cancer. It’s a painless procedure that gives a clear indication of whether a mass in the testicle is solid or filled with fluid. A fluid-filled lump is usually harmless. A more solid lump may signal that the swelling is cancerous.
The next step is a blood test. Many testicular cancers make high levels of certain proteins called tumor markers such as HCG and alpha-fetoprotein (AFP), which are both associated with pregnancy. When these tumor markers are in the blood, it suggests that there's a testicular tumor.
Rises in levels of HCG or AFP can also help doctors tell which type of testicular cancer it might be.
A testicular tumor might also increase the levels of an enzyme called lactate dehydrogenase (LDH). A high LDH level often, but not always, indicates widespread disease. But, LDH levels can also be increased with some non-cancerous conditions.
How is testicular cancer treated?
The first treatment for all cases of testicular cancer, whatever the stage, is an orchidectomy – a surgical procedure to remove the testicle.
“By removing the entire affected testicle, your chances of making a full recovery are greatly improved,” Wood explains. “Removing only the tumor may result in the cancer spreading.”
Sex life and the ability to father children are typically not affected, he says.
After surgery, doctors monitor HCG level to determine if the cancer is gone.
“If the patient had elevated levels of HCG before surgery, you would expect those level to return to normal after surgery,” Wood says. “If they don’t, it means there are residual cancer cells that have to be treated with chemotherapy or radiation.”
Testicular cancer survival rates
Testicular cancer is highly treatable, even when cancer has spread beyond the testicle.
“While a cancer diagnosis is always serious,” Wood says, “the good news about testicular cancer is that the vast majority of cases – even if they're caught further along – are still very curable.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Why choose MD Anderson for testicular cancer treatment?
At MD Anderson's Genitourinary Cancer Center, a team of experts targets each patient's testicular cancer, providing customized care to match your unique disease and circumstances. These highly focused physicians, as well as a specially trained support staff, personalize your care to ensure the most-advanced treatments with the least impact on your body.
As one of the nation's most active cancer centers, MD Anderson sees many more patients with testicular cancer than does the average oncologist. This translates to an extraordinary level of expertise, which can mean higher chances for successful treatment.
And at MD Anderson you're surrounded by the strength of one of the nation's largest and most experienced comprehensive cancer centers, which has all the support and wellness services needed to treat the whole person – not just the disease.
Knowledge and experience
Treatment for testicular cancer frequently requires surgery. Procedures, especially those to remove lymph glands, are delicate and require a high level of skill.
Our surgeons are among the most experienced in testicular cancer in the nation. They employ the latest techniques, which may mean less recovery time, fewer side effects, and faster healing for many patients. MD Anderson surgeons also have extensive experience in advanced nerve-sparing techniques.
If testicular cancer spreads, strong doses of chemotherapy may be needed. Our experienced oncologists take great care in selecting the best treatment for you. If a stem-cell transplant is necessary, MD Anderson offers one of the premier programs in the nation.
Pioneering research
As one of the world's largest cancer research centers, MD Anderson is leading investigations into new methods of testicular cancer diagnosis and treatment. You benefit from the most advanced research, and we're able to offer clinical trials (research studies) of new therapies for testicular cancer.
From the moment my brother received his diagnosis, I promised I would fight for him.
Cora Connor
Caregiver

How a testicular cancer diagnosis led me to Mt. Kilimanjaro
Before scaling Mt. Kilimanjaro in June 2018, I’d never climbed a real mountain. I live in Beaumont, Texas, which is only around 30 feet above sea level. So, getting to the top of Kilimanjaro (19,341 feet) was going to be a real challenge.
But after seeing two-time cancer survivor Sean Swarner’s story on TV while recovering from testicular cancer treatment myself last year, I was determined to go on a trip of my own one day to celebrate beating this disease.
Paying it forward
That trip actually came about in a funny way. After watching a video about Sean’s accomplishments, I’d sent him an email saying how much he’d inspired me. Because not only did he defy the odds by beating two different types of cancer considered terminal, he also completed the “Explorer’s Grand Slam,” in which a person scales the highest peaks on seven continents and visits both the North and South Poles. And he did it all with only one lung.
A few days later, Sean emailed me back. He said he’d always wanted to return to Nepal, and he invited me to go with him as part of a joint fundraiser. My sights were set on going to Mt. Everest Base Camp at the time, so that sounded great. I agreed.
Unfortunately, we ended up not meeting our fundraising goals, so we didn’t make it to the Mt. Everest Base Camp. But, each year, Sean takes one cancer survivor to the top of Mt. Kilimanjaro for free through his foundation. And this year, he took me. To pay it forward, I set up another fundraiser that benefitted Sean’s foundation. The proceeds will help pay for the next survivor to go on the trip in 2019.
What my trip meant to me
Sean takes a special flag with him on every adventure. On it, is the word “HOPE,” along with names of people whose lives have been touched by cancer. On this trip, my dad’s name was on there, along with my grandparents’ names and my name.
The climb was not easy. In fact, it was one of the most difficult things I’ve ever done. The combination of altitude, low oxygen, little sleep, and long days made it really tough. But I did make it to the top, and I had that flag with me. I was holding it as I walked to the summit.
I left the flag attached to the sign that everyone takes a picture with. It might have just been a piece of cloth with some names scribbled on it in black marker to some people, but it meant so much more than that. I wasn’t just climbing this mountain for me. I was doing it for the people whose names were on that flag, so that all of Africa could see what cancer survivors are able to do.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Treatment at MD Anderson
Testicular cancer is treated in our Genitourinary Center.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients, family members and loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.


