Research
Our faculty investigators and researchers in Radiation Oncology focus on some of the most innovative discoveries and impactful areas in oncology to help bring quality treatment care options to our patients.
We have a broad-ranging clinical research portfolio of approximately 74 therapeutic trials, many that are supported by federal and state sponsors, industry partners, philanthropy and institutional awards.
Our research areas align with our clinical priorities and expertise, including but not limited to:
- Proton Therapy
- Stereotactic Body Radiation Treatment (SBRT)
- Brachytherapy
- Accelerated Partial Breast Irradiation
- Stereotactic Radiosurgery
- Immuno-Radiation Therapy
- Chemo-Radiation Therapy
Radiation Oncology Strategic Initiatives

The MD Anderson Radiation Oncology division faculty leadership have prioritized several key discovery and educational areas to focus, guide and advance translational research toward improving radiation therapies.
This is represented in the Radiation Oncology Strategic Initiatives (ROSI), which comprises six pillars: Advanced Imaging, Global Radiation Treatment Access, Immuno-Radiation Therapy, Particle Therapy, FLASH Radiation Therapy and Metastatic Disease Radiation Treatment.
These priority pillars are supported by six cross-cutting infrastructure platforms: data access, computational modeling and artificial intelligence, predictive biomarkers, clinical trials, education, and value, access and quality.
Radiation Oncology Clinical Research Council
Our clinical research portfolio management and study prioritization for the division is guided by the specialty sections’ leadership and the Clinical Research Council (CRC), co-chaired by Zhongxing Liao, M.D., professor in the Radiation Oncology department, and Sam Beddar, Ph.D., professor in the Radiation Physics department.
Access to Clinical Trials
Our experienced and compassionate clinical research teams support Radiation Oncology trials at the main campus, as well as in the Houston Area Locations (HALs) including West Houston, Sugar Land, The Woodlands, League City and UTMB Galveston.
Patients who are interested in participating in a clinical trial should contact their provider for guidance and additional information.
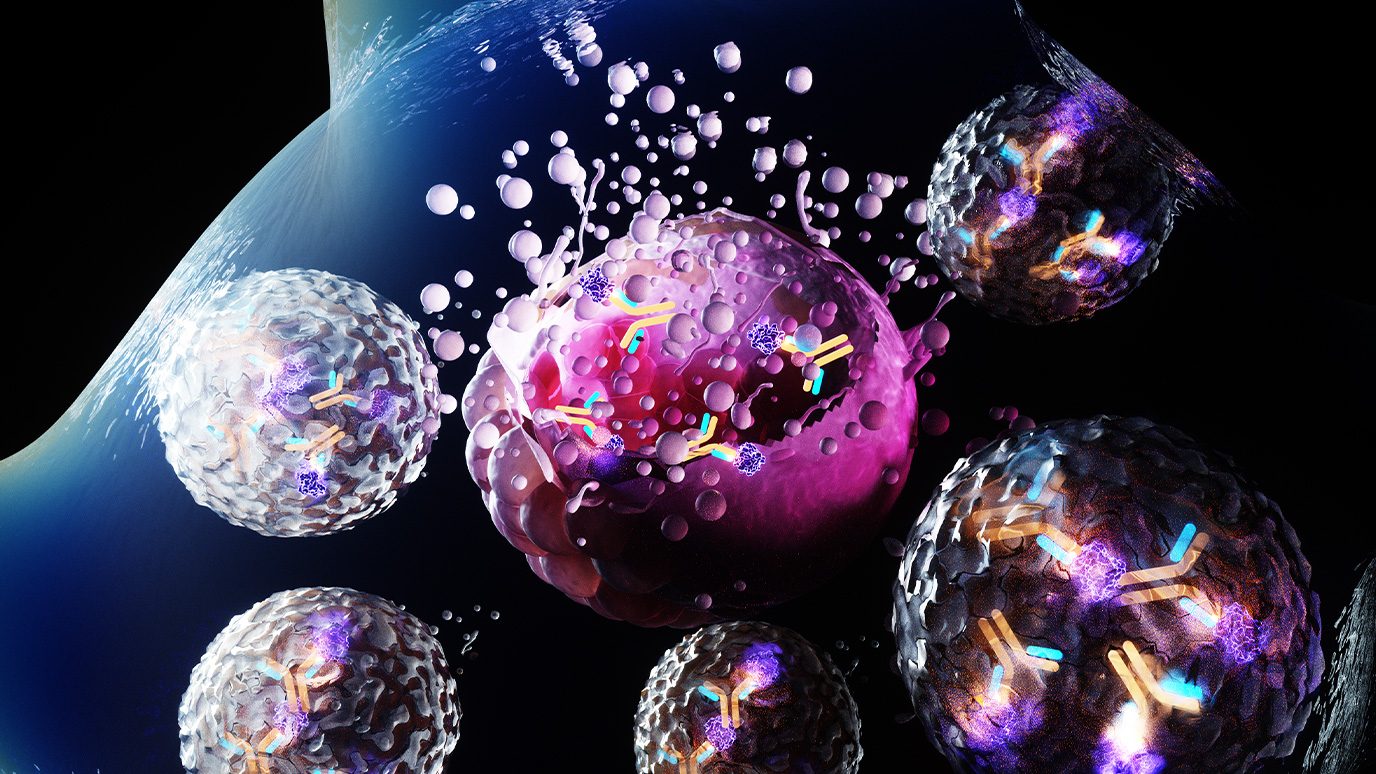
MD Anderson researchers develop novel antibody-toxin conjugate
Researchers at The University of Texas MD Anderson Cancer Center have developed a novel antibody-toxin conjugate (ATC) designed to stimulate immune-mediated eradication of tumors. According to preclinical results published today in Nature Cancer, the new approach combined the benefits of more well-known antibody-drug conjugates (ADCs) with those of immunotherapies.
ADCs have emerged as a breakthrough in recent years due to their modular design, which enables precise delivery of therapies to tumors by targeting specific proteins expressed on cancer cells. These conjugates use their tumor-targeting ability to deliver a payload, usually a chemotherapy, directly to the cancer cells, resulting in their destruction.
According to corresponding author Wen Jiang, M.D., Ph.D., associate professor of Radiation Oncology, the ATC differs in that it’s not designed to kill the cancer cells directly.
“Effective ADCs are designed to destroy tumor cells, but they often do so incompletely, leading to resistance and recurrence,” Jiang said. “With this new ATC approach, we aim to trigger the body’s natural immune response. This should not only limit side effects but also allow the immune system to attack tumors throughout the body and potentially prevent their recurrence.”
Many solid tumors express the CD47 protein on their surface, which serves as a “don’t eat me” signal to the body’s immune system, allowing the tumor to evade detection. The antibody in this ATC targets CD47, but instead of delivering a chemotherapy payload to destroy the tumor, it delivers a bacterial toxin.
Simplified, the CD47 antibody binds to cancer cells, marking them to be eaten by the body’s immune cells. Once the immune cells engulf the tumor, the toxin is released inside, becoming activated and creating pathways that allow tumor DNA and protein fragments, which are usually destroyed, to escape. These materials are then processed to help the immune cell better recognize and mount its own antitumor defense.
“This design was inspired by bacteria, which have an incredible ability to escape from cells’ internal traps, multiply and spread, all while keeping the host cell alive and functional,” Jiang said. “We’re harnessing that same ability to shuttle intact tumor material to the right places within immune cells. Instead of being destroyed, the tumor material teaches the body to better recognize tumor cells.”
In preclinical models of breast cancer and melanoma, this approach demonstrated multiple benefits. By educating the immune system to recognize unique signatures of cancer cells that distinguish them from normal tissues, the new ATC was more effective at triggering an antitumor immune response. This allowed immune cells to eliminate tumors throughout the body.
The T cells created by this process also remained after two months, suggesting a memory effect to this approach that could prevent tumor recurrence.
“We hope this new design opens up an entirely new avenue for research that expands the possibilities for ATCs,” said first author Benjamin Schrank, M.D., Ph.D., resident physician in Radiation Oncology. “We want to train the immune system to recognize and respond to these tumors so it can continue fighting cancer even after the treatment is completed.”
This method also has potential as to be combined with conventional therapies, especially with radiation therapy. Many solid tumors respond to radiation therapy by trying to shield themselves with proteins, including CD47. This upregulation of CD47 would make them even more susceptible to the ATC.
“This immune-stimulating ATC concept extends beyond CD47, and we are already developing projects that target other tumor-specific receptors to create ADCs that enable the body to target a wide range of difficult-to-treat cancers,” said Betty Kim, M.D., Ph.D., professor of Neurosurgery and co-lead of the study. “Our goal is to have the first of these ready for clinical testing within the next three to five years.”
This work was supported in part by the National Institutes of Health (R01NS117828, P30CA016672) and the American Cancer Society (RSG-22-052-01-IBCD, PF-24-1156745-01-ET), the Radiological Society of North America (RR1644), the SITC-Merck Cancer Immunotherapy Clinical Fellowship, and the American Society of Clinical Oncology Young Investigator Award (2024YIA-0832385427).
Radiation Oncology Strategic Initiatives
The Division of Radiation Oncology launched the ROSI Seed Award Program in 2017, to provide critical infrastructure and resources toward the acceleration of breakthroughs in radiation oncology research.
Clinical Trials
Our patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Physician Scientist and Translational Research Group
The Radiation Oncology division supports the Physician-Scientist and Translational Science Program, which bridges research efforts from diverse departments to translate to the clinic.
We facilitate robust collaboration between the clinical departments Breast Radiation Oncology, Central Nervous System Radiation Oncology, Gastrointestinal (GI) Radiation Oncology, Genitourinary (GU) Radiation Oncology and Radiation Oncology, along with the departments of Radiation Physics and other departments to bring exciting discoveries to our patients.
Beyond expanding our research efforts, the program provides mentorship to trainees, residents and junior faculty to grow their research careers. This includes providing senior mentorship and more granular assistance with grants and administration. An overarching goal of the program is to serve as a beacon of excellence for translational research in Radiation Oncology, not only for our institution, but also for the global community.
This program is deeply connected to the institution’s mission to end cancer through innovative basic and translational research done both in parallel and embedded in cutting-edge clinical trials.
Physician-Scientists Group Interests
Microbiome
Investigators are exploring how the microbiome may influence the ability of the body’s own immune system to attack HPV-laden cancer cells. Our physician scientists are assessing how changes in the microbiome affect patient outcomes to cancer therapy, such as radiation therapy. Their findings raise the possibility of manipulating the microbiome to “engineer” health and to improve responses to cancer therapies.
Immune System
Radiation therapy has been shown to negatively affect the immune system. Conversely, radiation therapy has also been shown to enhance positive responses to immunotherapy. Research on the immune-modulating effects of radiation therapy on tumors will ultimately lead to new combinations of cancer treatments and treatment regimens.
Radiation Treatment Modalities
Standard and emerging treatment modalities of radiation therapy delivery, including particle therapy (e.g., proton therapy), Gamma Knife®, brachytherapy, stereotactic body radiation treatment (SBRT), which was pioneered by our physician scientist Albert Koong, M.D., Ph.D. for treating pancreatic cancer; intensity modulated radiation therapy (IMRT), volumetric modulated arc therapy (VMAT), and FLASH radiation therapy. This research will help overcome significant hurdles for cancer patient’s well-being and life-extending treatment options.
FLASH Radiation Therapy
One of the latest advances in radiation therapy, FLASH delivers radiation at ultra-high dose rates, which are approximately 100 times faster than conventional radiation therapy delivery methods. FLASH radiation therapy may be one of the greatest breakthroughs in radiation therapy in decades. FLASH radiation therapy research will facilitate the translation of this paradigm-shift radiation therapy delivery method to the clinic.
Particle Therapy
Using high-energy charged particles, such as protons, in radiation therapy is considered cutting-edge due to its healthy tissue-sparing effects. It is an attractive therapeutic option for many cancer patients. A wide variety of cancers can be treated with proton therapy. MD Anderson Cancer Center was the first institution in the United States and second in the world to implement intensity modulated proton therapy (IMPT).
Predictive Biomarkers
Biomarkers can be used to diagnose cancer as well as to predict cancer patient outcomes. Research on biomarkers will help identify which type of radiation therapy is best for each patient. Biomarker research in the division will lead to planning safer and more efficacious radiation therapy for cancer patients and more precisely diagnose cancer subtypes.