- Research Resources
- Excellence in Science
- Excellence in Science FY21
Fiscal Year 2021 Awardees
Research is a cornerstone of MD Anderson’s quest to end cancer. The Excellence in Science program is the online showcase for the Wall of Science, our quarterly program for honoring outstanding primary research selected from among publications in top journals by MD Anderson’s world-renowned scientists.
Quarter 1 (September–November 2020)
Qing Deng, Ph.D., Guangchun Han, Ph.D., Sattva S. Neelapu, M.D., Linghua Wang, Ph.D., and Michael Green, Ph.D.
Nature Medicine
Characteristics of anti-CD19 CAR T cell infusion products associated with efficacy and toxicity in patients with large B cell lymphomas

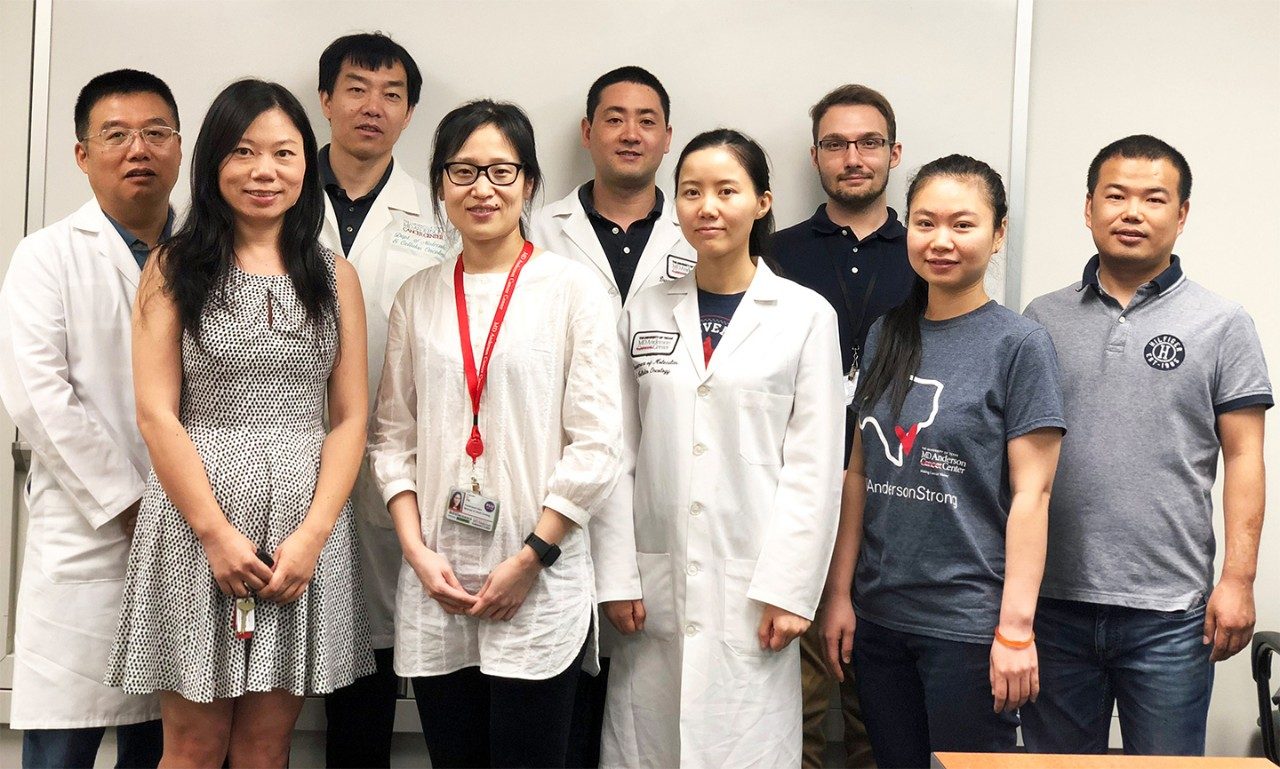
Top row, left to right: Qing Deng and Michael R. Green
Middle row, left to right: Guangchun Han and Sattva S. Neelapu
Bottom row: Linghua Wang
Co-authors not pictured: Nahum Puebla-Osorio, Man Chun John Ma, Paolo Strati, Beth Chasen, Enyu Dai, Minghao Dang, Neeraj Jain, Haopeng Yang, Yuanxin Wang, Shaojun Zhang, Ruiping Wang, Runzhe Chen, Jordan Showell, Sreejoyee Ghosh, Sridevi Patchva, Qi Zhang, Ryan Sun, Frederick Hagemeister, Luis Fayad, Felipe Samaniego, Hans C. Lee, Loretta J. Nastoupil, Nathan Fowler, R. Eric Davis and Jason Westin

Qing Deng, Ph.D.
Instructor
Lymphoma-Myeloma

Guangchun Han, Ph.D.
Postdoctoral Fellow
Genomic Medicine

Sattva Neelapu, M.D.
Professor
Lymphoma/Myeloma

Linghua Wang, M.D., Ph.D.
Assistant Professor
Genomic Medicine

Michael Green, Ph.D.
Associate Professor
Lymphoma-Myeloma & Genomic Medicine
Courtney DiNardo, M.D., and Marina Konopleva, M.D., Ph.D.

Courtney DiNardo, M.D.
Associate Professor
Leukemia
Associate Chair, Institutional Review Board

Marina Konopleva, M.D., Ph.D.
Deputy Chair, Leukemia
Professor, Leukemia & Stem Cell Transplantation
Frances King Black Memorial Professorship for Cancer Research
New England Journal of Medicine
Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia
Jianjun Gao, M.D., Ph.D., and Padmanee Sharma, M.D., Ph.D.
Nature Medicine
Neoadjuvant PD-L1 plus CTLA-4 blockade in patients with cisplatin-ineligible operable high-risk urothelial carcinoma
Authors
Jianjun Gao, Neema Navai, Omar Alhalabi, Arlene Siefker-Radtke, Matthew T. Campbell, Rebecca Slack Tidwell, Charles C. Guo, Ashish M. Kamat, Surena F. Matin, John C. Araujo, Amishi Y. Shah, Pavlos Msaouel, Paul Corn, Jianbo Wang, John N. Papadopoulos, Shalini S. Yadav, Jorge M. Blando, Fei Duan, Sreyashi Basu, Wenbin Liu, Yu Shen, Yuwei Zhang, Marc Daniel Macaluso, Ying Wang, Jianfeng Chen, Jianhua Zhang, Andrew Futreal, Colin Dinney, James P. Allison, Sangeeta Goswami and Padmanee Sharma

Jianjun Gao, M.D., Ph.D.
Associate Professor
Genitourinary Medical Oncology

Padmanee Sharma, M.D., Ph.D.
Professor
Genitourinary Medical Oncology and Immunology
Associate Vice President, Immunobiology
T.C. and Jeanette Hsu Endowed Chair in Cell Biology
Vivek Subbiah, M.D.

Vivek Subbiah, M.D.
Associate Professor
Investigational Cancer Therapeutics and Pediatrics
Chair, GMEC Curriculum Subcommittee
Clinical Medical Director, Clinical Center for Targeted Therapy
Executive Director, Cancer Medicine Research
New England Journal of Medicine
Efficacy of Selpercatinib in RET Fusion–Positive Non–Small-Cell Lung Cancer
Yaohua Zhang, Ph.D., Chunru Lin, Ph.D., and Liuqing Yang, Ph.D.
Nature Cell Biology
The lncRNA H19 alleviates muscular dystrophy by stabilizing dystrophin
Left to right: Ke Liang, Chunru Lin, Liuqing Yang, Yajuan Li, Qingsong Hu, Jianjun Jiang, Sergey D. Egranov, Tina Nguyen and Yaohua Zhang
Co-authors not pictured: Yutao Xi, Zhen Xing, Zhao Zhang, Lisa Huang, Jianbo Wu, Chengcao Sun, Zilong Zhao, David H. Hawke, Jin Li, Deqiang Sun, Jean J. Kim, Ping Zhang, Jie Cheng, Abid Farida, Mien-Chie Hung, Leng Han and Radbod Darabi
Yaohua Zhang, Ph.D.
Postdoctoral Fellow
Molecular & Cellular Biology

Chunru Lin, M.D., Ph.D.
Associate Professor
Molecular and Cellular Oncology

Liuqing Yang, Ph.D.
Associate Professor
Molecular & Cellular Biology
Di Zhao, Ph.D., Li Cai, Ph.D., Y. Alan Wang, Ph.D., and Ronald A. DePinho, M.D.

Di Zhao, Ph.D.
Assistant Professor
Experimental Radiation Oncology

Li Cai, Ph.D.
Graduate Research Assistant
Cancer Biology

Y. Alan Wang, Ph.D.
Associate Professor
Cancer Biology

Ronald A. DePinho, M.D.
Professor
Cancer Biology and Genomic Medicine Research
Harry Graves Burkhart III Distinguished University Chair in Cancer Research
Cancer Discovery
Chromatin Regulator CHD1 Remodels the Immunosuppressive Tumor Microenvironment in PTEN-Deficient Prostate Cancer

Left to right: Ke Liang, Chunru Lin, Liuqing Yang, Yajuan Li, Qingsong Hu, Jianjun Jiang, Serey Egranov, Tina Nguyen and Yaohua Zhang
Co-authors: Di Zhao, Li Cai, Xin Lu, Xin Liang, Jiexi Li, Peiwen Chen, Michael Ittmann, Xiaoying Shang, Shan Jiang, Haoyan Li, Chenling Meng, Ivonne Flores, Jian H. Song, James W. Horner, Zhengdao Lan, Chang-Jiun Wu, Jun Li, Qing Chang, Ko-Chien Chen, Guocan Wang, Pingna Deng, Denise J. Spring, Y. Alan Wang and Ronald A. DePinho
Quarter 2 (December 2020–February 2021)
Han Chen, Ph.D., and Han Liang, Ph.D.
Cancer Cell
A High-Resolution Map of Human Enhancer RNA Loci Characterizes Super-enhancer Activities in Cancer

Han Chen, Ph.D.
Postdoctoral Fellow
Bioinformatics and Computational Biology

Han Liang, Ph.D.
Deputy Chair, Bioinformatics and Computational Biology
Professor
Bioinformatics and Computational Biology & Systems Biology
Barnhart Family Distinguished Professorship in Targeted Therapies
John Victor Heymach, M.D., Ph.D.

John V. Heymach, M.D., Ph.D.
Chair, Thoracic/Head and Neck Medical Oncology
Professor, Cancer Biology
David Bruton, Jr. Chair
Authors
JP Robichaux, X Le, RSK Vijayan, JK Hicks, S Heeke, YY Elamin, HY Lin, H Udagawa, F Skoulidis, H Tran, S Varghese, J He, F Zhang, MB Nilsson, L Hu, A Poteete, W Rinsurongkawong, X Zhang, C Ren, X Liu, L Hong, J Zhang, L Diao, R Madison, AB Schrock, J Saam, V Raymond, B Fang, J Wang, MJ Ha, JB Cross, JE Gray, and JV Heymach
Nature
Structure-based classification predicts drug response in EGFR-mutant NSCLC
Jun Li, Ph.D., and Han Liang, Ph.D.
Cancer Cell
Large-Scale Characterization of Drug Responses of Clinically Relevant Proteins in Cancer Cell Lines
Authors
W Zhao, J Li, MJM Chen, Y Luo, Z Ju, NK Nesser, K Johnson-Camacho, CT Boniface, Y Lawrence, NT Pande, MA Davies, M Herlyn, T Muranen, IK Zervantonakis, E von Euw, A Schultz, SV Kumar, A Korkut, PT Spellman, R Akbani, DJ Slamon, JW Gray, JS Brugge, Y Lu, GB Mills and H Liang

Jun Li, Ph.D.
Assistant Professor
Bioinformatics and Computational Biology

Han Liang, Ph.D.
Deputy Chair, Bioinformatics and Computational Biology
Professor
Bioinformatics and Computational Biology & Systems Biology
Barnhart Family Distinguished Professorship in Targeted Therapies
Nicholas Navin, Ph.D.

Nicholas Navin, Ph.D.
Professor
Genetics and Bioinformatics and Computational Biology
Director, CPRIT Single Cell Sequencing Core
The Grady F. Saunders, PhD Distinguished Professorship for Molecular Biology
Nature Biotechnology
Delineating copy number and clonal substructure in human tumors from single-cell transcriptomes
Authors
Ruli Gao, Shanshan Bai, Ying C. Henderson, Yiyun Lin, Aislyn Schalck, Yun Yan, Tapsi Kumar, Min Hu, Emi Sei, Alexander Davis, Fang Wang, Simona F. Shaitelman, Jennifer Rui Wang, Ken Chen, Stacy Moulder, Stephen Y. Lai and Nicholas E. Navin
Shao-Cong Sun, Ph.D.
Nature Immunology
NF-κB-inducing kinase maintains T cell metabolic fitness in antitumor immunity

Shao-Cong Sun, Ph.D.
Professor and Deputy Chair, of Immunology
Administrative Director, South Campus Research Bldg
Moshe Talpaz Endowed Chair in Immunology
Ruiping Wang, Ph.D., Jaffer A. Ajani, M.D., and Linghua Wang, Ph.D.

Ruiping Wang, Ph.D.
Postdoctoral Fellow
Genomic Medicine

Jaffer A. Ajani, M.D.
Professor
GI Medical Oncology
Committee Chair, Institutional Review Board

Linghua Wang, M.D., Ph.D.
Assistant Professor
Genomic Medicine
Nature Medicine
Single-cell dissection of intratumoral heterogeneity and lineage diversity in metastatic gastric adenocarcinoma

Top row, left to right: Ruiping Wang, Linghua Wang and Minghao Dang
Middle row, left to right: Guangchun Han, Dapeng Hao and Jaffer A. Ajani
Bottom row, left to right: Shumei Song, Namita D Shanbhag and Melissa Pool Pizzi
Co-authors not pictured: K Harada, F Wang, M Zhao, G Tatlonghari, S Zhang, Y Lu, S Zhao, BD Badgwell, MB Murphy, JS Estrella, S Roy-Chowdhuri, AAF Abdelhakeem, Y Wang, G Peng, S Hanash, GA Calin, X Song, Y Chu, J Zhang, M Li, K Chen, AJ Lazar, A Futreal
Sriram Yennu, M.D., and Eduardo Bruera, M.D.
JAMA Oncology
Frequency of and Factors Associated With Nonmedical Opioid Use Behavior Among Patients With Cancer Receiving Opioids for Cancer Pain
Authors
Sriram Yennurajalingam, Joseph Arthur, Suresh Reddy, Tonya Edwards, Zhanni Lu, Aline Rozman de Moraes, Susamma M. Wilson, Elif Erdogan, Manju P. Joy, Shirley Darlene Ethridge, Leela Kuriakose, Jimi S. Malik, John M. Najera, Saima Rashid, Yu Qian, Michal J. Kubiak, Kristy Nguyen, Jimin Wu, David Hui and Eduardo Bruera

Sriram Yennurajalingam, M.D., M.S.
Professor
Palliative, Rehabilitation and Integrative Medicine

Eduardo Bruera, M.D.
Professor and Chair, of Palliative Care, Rehabilitation and Integrative Medicine
Frank T. McGraw Memorial Chair in the Treatment of Cancer
Quarter 3 (March–May 2021)
James Allison, Ph.D.
Cancer Discovery
A Genetic Mouse Model Recapitulates Immune Checkpoint Inhibitor-Associated Myocarditis and Supports a Mechanism-Based Therapeutic Intervention

James Allison, Ph.D.
VP and Chair, Immunobiology
Regental Professor
Immunology and Cancer Biology
Olga Keith Wiess Distinguished University Chair for Cancer Research
Authors
Spencer C. Wei, Wouter C. Meijers, Margaret L. Axelrod, Nana-Ama A.S. Anang, Elles M. Screever, Elizabeth C. Wescott, Douglas B. Johnson, Elizabeth Whitley, Lorenz Lehmann, Pierre-Yves Courand, James J. Mancuso, Lauren E. Himmel, Benedicte Lebrun-Vignes, Matthew J. Wleklinski, Bjorn C. Knollmann, Jayashree Srinivasan, Yu Li, Oluwatomisin T. Atolagbe, Xiayu Rao, Yang Zhao, Jing Wang, Lauren I.R. Ehrlich, Padmanee Sharma, Joe-Elie Salem, Justin M. Balko, Javid J. Moslehi, and James P. Allison
Tina Cascone, M.D., Ph.D., John V. Heymach, M.D., Ph.D., and Boris Sepesi, M.D.

Tina Cascone, M.D., Ph.D.
Assistant Professor
Thoracic Head & Neck Medical Oncology

John V. Heymach, M.D., Ph.D.
Chair, Thoracic/Head and Neck Medical Oncology
Professor, Cancer Biology
David Bruton, Jr. Chair

Boris Sepesi, M.D.
Associate Professor
Thoracic and Cardiovascular Surgery
Nature Medicine
Neoadjuvant nivolumab or nivolumab plus ipilimumab in operable non-small cell lung cancer: the phase 2 randomized NEOSTAR trial
Authors
Tina Cascone, William N. William Jr, Annikka Weissferdt, Cheuk H. Leung, Heather Y. Lin, Apar Pataer, Myrna C. B. Godoy, Brett W. Carter, Lorenzo Federico, Alexandre Reuben, Md Abdul Wadud Khan, Hitoshi Dejima, Alejandro Francisco-Cruz, Edwin R. Parra, Luisa M. Solis, Junya Fujimoto, Hai T. Tran, Neda Kalhor, Frank V. Fossella, Frank E. Mott, Anne S. Tsao, George Blumenschein Jr, Xiuning Le, Jianjun Zhang, Ferdinandos Skoulidis, Jonathan M. Kurie, Mehmet Altan, Charles Lu, Bonnie S. Glisson, Lauren Averett Byers, Yasir Y. Elamin, Reza J. Mehran, David C. Rice, Garrett L. Walsh, Wayne L. Hofstetter, Jack A. Roth, Mara B. Antonoff, Humam Kadara, Cara Haymaker, Chantale Bernatchez, Nadim J. Ajami, Robert R. Jenq, Padmanee Sharma, James P. Allison, Andrew Futreal, Jennifer A. Wargo, Ignacio I. Wistuba, Stephen G. Swisher, J. Jack Lee, Don L. Gibbons, Ara A. Vaporciyan, John V. Heymach, and Boris Sepesi
Natasha M. Flores, Ph.D., and Pawel K. Mazur, Ph.D.
Nature
Elevated NSD3 histone methylation activity drives squamous cell lung cancer

The Mazur Lab 2021/2022 (from left to right): Pawel K. Mazur (center), Liyong Zeng, Simone Hausmann, Mary Fuentes, Marcello Caporicci, Jibo Wu, Xiaojie Yang, Xiaoyin Lu, Ana Morales Benitez, Natasha Flores
Co-authors not pictured: Gang Yuan, Shane M. Lofgren, Vladlena Kharchenko, Maria Angulo-Ibanez, Deepanwita Sengupta, Iwona Czaban, Dulat Azhibek, Silvestre Vicent, Wolfgang Fischle, Mariusz Jaremko, Bingliang Fang, Ignacio I. Wistuba, Katrin F. Chua, Jack A. Roth, John D. Minna, Ning-Yi Shao, Łukasz Jaremko and Or Gozani

Natasha M. Flores, Ph.D.
Postdoctoral Fellow
Experimental Radiation Oncology

Pawel K. Mazur, Ph.D.
Assistant Professor
Experimental Radiation Oncology
Carl M. Gay, M.D., Ph.D., and Lauren Averett Byers, M.D.

Carl M. Gay, M.D., Ph.D.
Assistant Professor
Thoracic Head & Neck Medical Oncology

Lauren Averett Byers, M.D.
Associate Professor
Thoracic Head & Neck Medical Oncology
Cancer Cell
Patterns of transcription factor programs and immune pathway activation define four major subtypes of SCLC with distinct therapeutic vulnerabilities

Left to right: Lauren Averett Byers Byers, Carl Gay and John V Heymach
Co-authors not pictured: CA Stewart, EM Park, L Diao, SM Groves, S Heeke, BY Nabet, J Fujimoto, LM Solis, W Lu, Y Xi, RJ Cardnell, Q Wang, G Fabbri, KR Cargill, NI Vokes, K Ramkumar, B Zhang, CM Della Corte, P Robson, SG Swisher, JA Roth, BS Glisson, DS Shames, II Wistuba, J Wang, V Quaranta and J Minna
Michael Kim, M.D., and Guillermina Lozano, Ph.D.
Cancer Discovery
Oncogenic KRAS Recruits an Expansive Transcriptional Network through Mutant p53 to Drive Pancreatic Cancer Metastasis

Left to right: Xinqun Li, Michael P. Kim and Jenying Deng
Co-authors not pictured: Yun Zhang, Bingbing Dai, Kendra L. Allton, Tara G. Hughes, Christian Siangco, Jithesh J. Augustine, Ya'an Kang, Joy M. McDaniel, Shunbin Xiong, Eugene J. Koay, Florencia McAllister, Christopher A. Bristow, Timothy P. Heffernan, Anirban Maitra, Bin Liu, Michelle C. Barton, Amanda R. Wasylishen, Jason B. Fleming and Guillermina Lozano

Michael Kim, M.D.
Assistant Professor
Surgical Oncology
Genetics

Guillermina Lozano, Ph.D.
Chair and Professor, Genetics
Administrative Director, George and Cynthia Mitchell Basic Sciences Research Building
Hubert L. Olive Stringer Distinguished Chair in Oncology in Honor of Sue Gribble Stringer
Scott Kopetz, M.D., Ph.D.

Scott Kopetz, M.D., Ph.D.
Professor, GI Medical Oncology
Del and Dennis McCarthy Distinguished Professorship in Gastrointestinal Cancer Research
Middle Row: Tracy Trevino (left) and Jamie Farber (right)
Bottom Row: Alex Sorokin
Journal of Clinical Oncology
Encorafenib Plus Cetuximab as a New Standard of Care for Previously Treated BRAF V600E–Mutant Metastatic Colorectal Cancer: Updated Survival Results and Subgroup Analyses from the BEACON Study
Chao Mao, Ph.D., and Boyi Gan, Ph.D.
Nature
DHODH-mediated ferroptosis defence is a targetable vulnerability in cancer

Chao Mao, Ph.D.
Postdoctoral Fellow
Experimental Radiation Oncology

Boyi Gan, Ph.D.
Professor
Experimental Radiation Oncology and Molecular & Cellular Oncology
Director, Radiation and Cancer Metabolism Research Program
Darlan Conterno Minussi, Hanghui Ye, and Nicholas Navin, Ph.D.

Darlan Conterno Minussi
Graduate Research Assistant
Genetics

Hanghui Ye
Graduate Research Assistant
Genetics

Nicholas Navin, Ph.D.
Professor
Genetics and Bioinformatics and Computational Biology
Director, CPRIT Single Cell Sequencing Core
The Grady F. Saunders, PhD Distinguished Professorship for Molecular Biology
Nature
Breast tumours maintain a reservoir of subclonal diversity during expansion
Authors
Darlan C. Minussi, Michael D. Nicholson, Hanghui Ye, Alexander Davis, Kaile Wang, Toby Baker, Maxime Tarabichi, Emi Sei, Haowei Du, Mashiat Rabbani, Cheng Peng, Min Hu, Shanshan Bai, Yu-wei Lin, Aislyn Schalck, Asha Multani, Jin Ma, Thomas O. McDonald, Anna Casasent, Angelica Barrera, Hui Chen, Bora Lim, Banu Arun, Funda Meric-Bernstam, Peter Van Loo, Franziska Michor, and Nicholas E. Navin
Wenyi Wang, Ph.D.
Cell
Characterizing genetic intra-tumor heterogeneity across 2,658 human cancer genomes

Wenyi Wang, Ph.D.
Professor
Bioinformatics & Comp Biology
Quarter 4 (June–August 2021)
Jaffer A. Ajani, M.D.
The Lancet
First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial

Jaffer A. Ajani, M.D.
Professor
GI Medical Oncology
Committee Chair, Institutional Review Board
Mauro Di Pilato, Ph.D.
Cell
CXCR6 positions cytotoxic T cells to receive critical survival signals in the tumor microenvironment
Nathan Fowler, M.D.
Cancer Cell
Conserved pan-cancer microenvironment subtypes predict response to immunotherapy

Nathan Fowler, M.D.
Clinical Professor
Lymphoma-Myeloma
Cara Haymaker, Ph.D., and Adi Diab, M.D.

Cara Haymaker, Ph.D.

Adi Diab, M.D.
Authors
Cara Haymaker, Daniel H. Johnson, Ravi Murthy, Salah Eddine Bentebibel, Marc I. Uemura, Courtney W. Hudgens, Houssein Safa, Marihella James, Robert H.I. Andtbacka, Douglas B. Johnson, Montaser Shaheen, Michael A. Davies, Shah Rahimian, Srinivas K. Chunduru, Denái R. Milton, Michael T. Tetzlaff, Willem W. Overwijk, Patrick Hwu, Nashat Gabrail, Sudhir Agrawal, Gary Doolittle, Igor Puzanov, Joseph Markowitz, Chantale Bernatchez and Adi Diab
Cancer Discovery
Tilsotolimod with Ipilimumab Drives Tumor Responses in Anti–PD-1 Refractory Melanoma

Left to right: Adi Diab, Cara Haymaker and Chantale Bernatchez
Chi-Lin Tsai, Ph.D., and John Tainer, Ph.D.
Molecular Cell
EXO5-DNA structure and BLM interactions direct DNA resection critical for ATR-dependent replication restart
Authors
Shashank Hambarde, Chi Lin Tsai, Raj K. Pandita, Albino Bacolla, Anirban Maitra, Vijay Charaka, Clayton R. Hunt, Rakesh Kumar, Oliver Limbo, Remy Le Meur, Walter J. Chazin, Susan E. Tsutakawa, Paul Russell, Katharina Schlacher, Tej K. Pandita and John A. Tainer

Chi-Lin Tsai, Ph.D.

John Tainer, Ph.D.
Zu Ye, Ph.D., John Tainer, Ph.D., and Zamal Ahmed, Ph.D.

Zu Ye, Ph.D.

John Tainer, Ph.D.

Zamal Ahmed, Ph.D.
Science Advances
GRB2 enforces homology-directed repair initiation by MRE11

Left to right: Zu Ye, Zamal Ahmed and John A. Tainer
Co-authors not pictured: Shengfeng Xu, Yin Shi, Albino Bacolla, Aleem Syed, Davide Moiani, Chi Lin Tsai, Qiang Shen, Guang Peng, Paul G. Leonard, Darin E. Jones and Bin Wang
Shuxing Zhang, Ph.D., Pharm.D., Chunru Lin, M.D., Ph.D., and Liuqing Yang, Ph.D.
Science
A noncoding RNA modulator potentiates phenylalanine metabolism in mice
Authors
Yajuan Li, Zhi Tan, Yaohua Zhang, Zhao Zhang, Qingsong Hu, Ke Liang, Yao Jun, Youqiong Ye, Yi Chuan Li, Chunlai Li, Lan Liao, Jianming Xu, Zhen Xing, Yinghong Pan, Sujash S. Chatterjee, Tina K. Nguyen, Heidi Hsiao, Sergey D. Egranov, Nagireddy Putluri, Cristian Coarfa, David H. Hawke, Preethi H. Gunaratne, Kuang Lei Tsai, Leng Han, Mien Chie Hung, George A. Calin, Fares Namour, Jean Louis Guéant, Ania C. Muntau, Nenad Blau, V. Reid Sutton, Manuel Schiff, François Feillet, Shuxing Zhang, Chunru Lin, Liuqing Yang

Shuxing Zhang, Ph.D., Pharm.D.

Chunru Lin, M.D., Ph.D.
Molecular and Cellular Oncology

Liuqing Yang, Ph.D.
Molecular and Cellular Oncology
Give Now
Research Areas
Find out about the four types of research taking place at UT MD Anderson.

