- Research Resources
- Excellence in Science
- Excellence in Science FY19
Fiscal Year 2019 Awardees
Research is a cornerstone of MD Anderson’s quest to end cancer. The Excellence in Science program is the online showcase for the Wall of Science, our quarterly program for honoring outstanding primary research selected from among publications in top journals by MD Anderson’s world-renowned scientists.
Quarter 1 (September–November 2018)
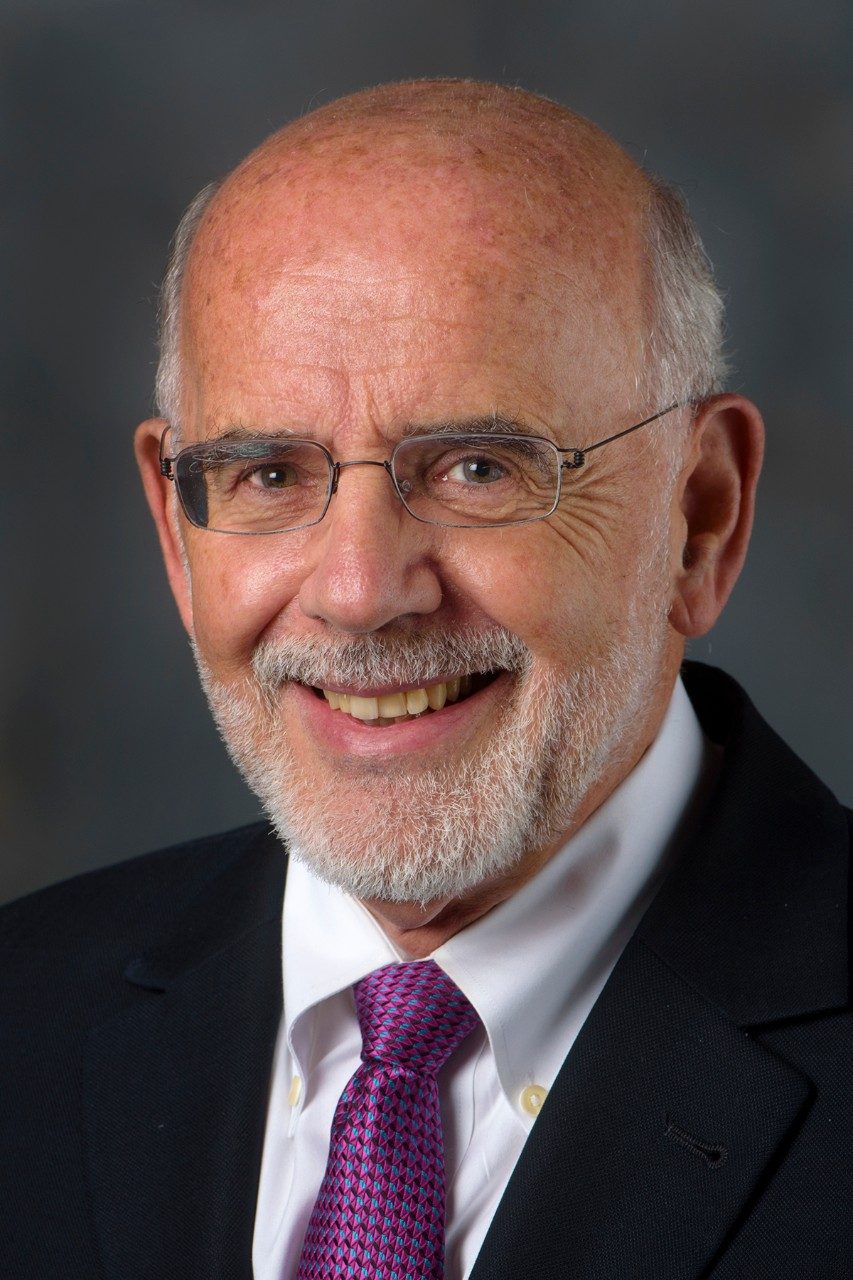
Don Lynn Gibbons, M.D., Ph.D.

Don Lynn Gibbons, M.D., Ph.D.
Associate Professor
Thoracic/Head and Neck Medical Oncology
Molecular & Cellular Oncology
Director, THNMO Translational Genetic Models Laboratory
Cancer Discovery
CD38-Mediated Immunosuppression as a Mechanism of Tumor Cell Escape from PD-1/PD-L1 Blockade

Left to right: Roxsan Manshouri, Limo Chen, Jared Fradette, Rakhee Bajaj, Don L. Gibbons, Samrat Kundu, Aparna Padhye, Laura Gibson, David Peng, Jessica Konen, Bertha Leticia Rodriguez, Pierre-Olivier Gaudreau and Joshua Kapere Ochieng
Co-authors not pictured: Lixia Diao, Yongbin Yang, Xiaohui Yi, B. Leticia Rodriguez, Yanli Li, Pamela A. Villalobos, Tina Cascone, Xi Liu, Lin Tan, Philip L. Lorenzi, Anfei Huang, Qiang Zhao, Di Peng, Christin Ungewiss, Jonathon Roybal, Pan Tong, Junna Oba, Ferdinandos Skoulidis, Weiyi Peng, Brett W. Carter, Carl M. Gay, Youhong Fan, Caleb A. Class, Jingfen Zhu, Jaime Rodriguez-Canales, Masanori Kawakami, Lauren Averett Byers, Scott E. Woodman, Vassiliki A. Papadimitrakopoulou, Ethan Dmitrovsky, Jing Wang, Stephen E. Ullrich, Ignacio I. Wistuba, John V. Heymach, F. Xiao-Feng Qin
Camilo Jimenez, M.D.
Journal of Nuclear Medicine
Efficacy and Safety of High-Specific-Activity 131I-MIBG Therapy in Patients with Advanced Pheochromocytoma or Paraganglioma

Camilo Jimenez, M.D.
Professor
Endocrine Neoplasia and Hormonal Disorders

Front row, left to right: Dao Le, Danielle Litofsky, Camilo Jimenez, Damaris Cruz-Goldberg, Gera Santiago
Back row, left to right: Bill Erwin and Mouhammed Habra
Pedro Tomas Ramirez, M.D.

Pedro Tomas Ramirez, M.D.
Professor
Gynecological Oncology & Reproductive Medicine
David M. Gershenson, M.D., Distinguished Professorship for Ovarian Cancer Research
New England Journal of Medicine
Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer
Katy Rezvani, M.D., Ph.D.

Katy Rezvani, M.D., Ph.D.
Professor, Stem Cell Transplantation
Chief, Section of Cellular Therapy Medical
Director, GMP Cell Therapy Laboratory
Director, Translational Research

Left to Right: Amanda Olson, Richard Champlin, Elizabeth J. "EJ" Shpall, Victor Mulanovich, Katayoun Rezvani, Indresh Kaur, Sudhakar Tummala and T. Linda Chi
Co-authors not pictured: Muharrem Muftuoglu, David Marin, Sairah Ahmed, Alessandra Ferrajoli and Li Li
New England Journal of Medicine
Allogeneic BK Virus–Specific T Cells for Progressive Multifocal Leukoencephalopathy
Koichi Takahashi, M.D., Ph.D.
Cell Stem Cell
PPM1D Mutations Drive Clonal Hematopoiesis in Response to Cytotoxic Chemotherapy

Koichi Takahashi, M.D.
Assistant Professor
Leukemia and Genomic Medicine
Authors
Joanne I. Hsu, Tajhal Dayaram, Ayala Tovy, Etienne De Braekeleer, Mira Jeong, Feng Wang, Jianhua Zhang, Timothy P. Heffernan, Sonal Gera, Jeffrey J. Kovacs, Joseph R. Marszalek, Christopher Bristow, Yuanqing Yan, Guillermo Garcia-Manero, Hagop Kantarjian, George Vassiliou, P. Andrew Futreal, Lawrence A. Donehower, Koichi Takahashi and Margaret A. Goodell
Quarter 2 (December 2018–February 2019)
Shaobo Dai, Ph.D., and Xiaodong Cheng, Ph.D.

Shaobo Dai, Ph.D.
Postdoctoral Fellow
Epigenetics and Molecular Carcinogenesis

Xiaodong Cheng, Ph.D.
Professor
Epigenetics and Molecular Carcinogenesis
Authors
Alex W. Wilkinson, Jonathan Diep, Shaobo Dai, Shuo Liu, Yaw Shin Ooi, Dan Song, Tie-Mei Li, John R. Horton, Xing Zhang, Chao Liu, Darshan V. Trivedi, Katherine M. Ruppel, José G. Vilches-Moure, Kerriann M. Casey, Justin Mak, Tina Cowan, Joshua E. Elias, Claude M. Nagamine, James A. Spudich, Xiaodong Cheng, Jan E. Carette and Or Gozani
Nature
SETD3 is an actin histidine methyltransferase that prevents primary dystocia
Simone Hausmann, Ph.D., and Pawel K. Mazur, Ph.D.
Cell
METTL13 Methylation of eEF1A Increases Translational Output to Promote Tumorigenesis

Pawel Karol Mazur, Simone Hausmann, Natasha Flores, Xiaoyin Lu, Jibo Wu, Liyong Zeng, Shane Lofgren, Mary Fuentes, Xiaoyi Huang and Marcello Caporicci
Co-authors not pictured: Shuo Liu, Scott Moore Carlson, Joel William Francis, Renjitha Pillai, Laura Hulea, Kristofferson Tandoc, Jiuwei Lu, Ami Li, Nicholas Dang Nguyen, Michael Paul Kim, Anirban Maitra, Huamin Wang, Ignacio Ivan Wistuba, John Anthony Porco Jr., Michael Cory Bassik, Joshua Eric Elias, Jikui Song, Ivan Topisirovic, Capucine Van Rechem and Or Gozani

Simone Hausmann, Ph.D.
Postdoctoral Fellow
Experimental Radiation Oncology

Pawel K. Mazur, Ph.D.
Assistant Professor
Experimental Radiation Oncology
Li Ma, Ph.D.

Li Ma, Ph.D.
Associate Professor
Experimental Radiation Oncology

Yutong Sun, Ashley Siverly, Li Ma, Zhenna Xiao, Sarah Lawhon, Zhicheng Zhou, Peijing Zhang, Fan Yao, Jongchan Kim
Co-authors not pictured: Hai-Long Piao, Beom-Jun Kim, Zhenbo Han, Yumeng Wang, Baochau N. Ton, Hyemin Lee, Boyi Gan, Shinichi Nakagawa, Matthew J. Ellis, Han Liang, Mien-Chie Hung and M. James You
Nature Genetics
Long noncoding RNA MALAT1 suppresses breast cancer metastasis
Nizar Tannir, M.D., Giulio Draetta, M.D., Ph.D., and Giannicola Genovese, M.D.
Cancer Cell
p53 Is a Master Regulator of Proteostasis in SMARCB1-Deficient Malignant Rhabdoid Tumors

Pictured: Edoardo Del Poggetto, Sanjana Srinivasan, Alessandro Carugo, Frederick Scott Robinson, Giulio F. Draetta, Rosalba Minelli, Giannicola Genovese, Nizar M. Tannir, Pavlos Msaouel, Melinda Soeung, Jose A. Karam, Federica Carbone
Co-authors not pictured: Luigi Sapio, James Tepper, Ziheng Chen, Sara Lovisa, Maria Svelto, Samirkumar Amin, Sara Loponte, Francesca Puca, Prasenjit Dey, Gabriel G. Malouf, Xiaoping Su, Liren Li, Dolores Lopez-Terrada, Dinesh Rakheja, Alexander J. Lazar, George J. Netto, Priya Rao, Alessandro Sgambato, Anirban Maitra, Durga N. Tripathi, Cheryl L. Walker, Timothy P. Heffernan, Andrea Viale, Charles W.M. Roberts

Nizar Tannir, M.D., F.A.C.P.
Professor and Chair ad interim
Genitourinary Medical Oncology
Ransom Horne, Jr. Professorship for Cancer Research

Giulio Draetta, M.D., Ph.D.
Senior Vice President, Chief Scientific Office
Professor, Genomic Medicine and Molecular & Cellular Oncology
Sewell Family Chair in Genomic Medicine in honor of Lynda Chen, M.D.

Giannicola Genovese, M.D.
Assistant Professor
Genitourinary Medical Oncology and Genomic Medicine Research
Yinghong Wang, M.D., Ph.D., and Beth Helmink, M.D., Ph.D.

Yinghong Wang, M.D., Ph.D.
Associate Professor
Gastroenterology Hepatology & Nutrition

Beth Helmink, M.D., Ph.D.
Fellow
Surgical Oncology
Nature Medicine
Fecal microbiota transplantation for refractory immune checkpoint inhibitor-associated colitis

Front row, left to right: Yinghong Wang, John R. Stroehlein and Beth Helmink
Back row, left to right: Alexander J. Lazar, Gottumukkala S. Raju, Jennifer A. Wargo, Robert R. Jenq and Chia-Chi Chang
Co-authors not pictured: Diana H. Wiesnoski, Vancheswaran Gopalakrishnan, Kati Choi, Hebert L. DuPont, Zhi-Dong Jiang, Hamzah Abu-Sbeih, Christopher A. Sanchez, Edwin R. Parra, Alejandro Francisco-Cruz, Matthew T. Campbell, Jianjun Gao, Sumit K. Subudhi, Dipen M. Maru, Jorge M. Blando, James P. Allison, Padmanee Sharma and Michael T. Tetzlaff
Quarter 3 (March–May 2019)
Moran Amit, M.D., Ph.D.
Journal of Clinical Oncology
Induction Chemotherapy Response as a Guide for Treatment Optimization in Sinonasal Undifferentiated Carcinoma
Authors
Moran Amit, Ahmed S. Abdelmeguid, Teemaranawich Watcherporn, Hideaki Takahashi, Samantha Tam, Diana Bell, Renata Ferrarotto, Bonnie Glisson, Michael E. Kupferman, Dianna B. Roberts, Shirley Y. Su, Shaan M. Raza, Franco DeMonte and Ehab Y. Hanna
Lauren Averett Byers, M.D.

Lauren Averett Byers, M.D.
Associate Professor
Thoracic/Head & Neck Medical Oncology

Left to Right: Bertha Leticia Rodriguez, John V. Heymach, Lauren A. Byers, Junya Fujimoto, Don L. Gibbons, Limo Chen and Jing Wang
Co-authors not pictured: Triparna Sen, Carminia M. Della Corte, Naoto Morikawa, Sandra Cristea, Thuyen Nguyen, Lixia Diao, Lerong Li, Youhong Fan, Yongbin Yang, Bonnie S. Glisson, Ignacio I. Wistuba, Julien Sage
Cancer Discovery
Targeting DNA Damage Response Promotes Antitumor Immunity through STING-Mediated T-cell Activation in Small Cell Lung Cancer
Michael A. Davies, M.D., Ph.D.
Cancer Discovery
Molecular Profiling Reveals Unique Immune and Metabolic Features of Melanoma Brain Metastases

Michael A. Davies, M.D., Ph.D.
Chair, Melanoma Medical Oncology
Professor
Melanoma Medical Oncology, Systems Biology & Translational Molecular Pathology

Lab Members: Wanleng Deng, Barbara Knighton, Y. N. Vashisht Gopal, Sruthy Varghese, Snigda Pramanik, Lauren Haydu, Debora Ledesma, Jennifer L. McQuade, Michael T. Tetzlaff, Grant M. Fischer, Renato Guerrieri and Michael A. Davies
Co-authors not pictured: Ali Jalali, David A. Kircher, Won-Chul Lee, Aron Y. Joon, Alexandre Reuben, Mariana P. de Macedo, Fernando C. L. Carapeto, Chendong Yang, Anuj Srivastava, Chandrashekar R. Ambati, Arun Sreekumar, Courtney W. Hudgens, Sherise D. Ferguson, Hussein A. Tawbi, Isabella C. Glitza, Jeffrey E. Gershenwald, Patrick Hwu, Jason T. Huse, Jennifer A. Wargo, P. Andrew Futreal, Nagireddy Putluri, Alexander J. Lazar, Ralph J. DeBerardinis, Joseph R. Marszalek, Jianjun Zhang and Sheri L. Holmen
Jo Ishizawa, M.D., Ph.D., and Michael Andreeff, M.D., Ph.D.
Michael Andreeff, M.D., Ph.D.
Professor
Leukemia and Stem Cell Transplantation
Paul and Mary Hass Chair in Genetics in Honor of Amanda White

Jo Ishizawa, M.D., Ph.D.
Assistant Professor
Leukemia
Cancer Cell
Mitochondrial ClpP-Mediated Proteolysis Induces Selective Cancer Cell Lethality

Left to right: Vivian Ruvolo, Ran Zhao, Michael Andreeff, Jo Ishizawa and Yuki Nishida
Co-authors not pictured: Sarah F. Zarabi, R. Eric Davis, Ondrej Halgas, Takenobu Nii, Yulia Jitkova, Jonathan St-Germain, Lauren E. Heese, Grace Egan, Samir H.Barghout, Rose Hurren, Wencai Ma, Marcela Gronda, Todd Link, Keith Wong, Mark Mabanglo, Kensuke Kojima, Gautam Borthakur, Neil MacLean, Man Chun John Ma, Andrew B. Leber, Mark D. Minden, Walid Houry, Hagop Kantarjian, Martin Stogniew, Brian Raught, Emil F. Pai and Aaron D. Schimmer
Naveen Pemmaraju, M.D.
New England Journal of Medicine
Tagraxofusp in Blastic Plasmacytoid Dendritic-Cell Neoplasm

Naveen Pemmaraju, M.D.
Associate Professor
Leukemia

Left to right: Marina Konopleva, Vicki Jeanis (Research Nurse) and Naveen Pemmaraju
Co-authors not pictured: Andrew A. Lane, Kendra L. Sweet, Anthony S. Stein, Sumithira Vasu, William Blum, David A. Rizzieri, Eunice S. Wang, Madeleine Duvic, J. Mark Sloan, Sharon Spence, Shay Shemesh, Christopher L. Brooks, John Balser, Ivan Bergstein, Jeffrey E. Lancet and Hagop M. Kantarjian
Jordi Rodon Ahnert, M.D., Ph.D., Apostolia Maria Tsimberidou, M.D., Ph.D., and Jiun-Kae Jack Lee, Ph.D.

Jordi Rodon Ahnert, M.D., Ph.D.
Associate Professor, Investigational Cancer Therapeutics & Genomic Medicine
Research Associate Medical Director, Institute for Personalized Cancer Therapy
Clinical Co-Director, Precision Oncology Decision Support Team

Apostolia Maria Tsimberidou, M.D., Ph.D.
Professor, Investigational Cancer Therapeutics
Past MD Anderson's official Representative and Head, Membership Committee of the WIN Consortium
Past Chair, Clinical Research Committee, American Society of Clinical Oncology

Jiun-Kae Jack Lee, Ph.D.
Associate Vice President, Quantitative Sciences
Professor, Basic Science
John G. and Marie Stella Kenedy Memorial Foundation, Chair
Authors
Jordi Rodon, Jean-Charles Soria, Raanan Berger, Wilson H. Miller, Eitan Rubin, Aleksandra Kugel, Apostolia Tsimberidou, Pierre Saintigny, Aliza Ackerstein, Irene Braña, Yohann Loriot, Mohammad Afshar,Vincent Miller, Fanny Wunder, Catherine Bresson, Jean-François Martini, Jacques Raynaud, John Mendelsohn, Gerald Batist, Amir Onn, Josep Tabernero, Richard Schilsky, Vladimir Lazar, J. Jack Lee and Razelle Kurzrock
Nature Medicine
Genomic and transcriptomic profiling expands precision cancer medicine: the WINTHER trial
Y. Alan Wang Ph.D., and Ronald A. DePinho, M.D.
Cancer Cell
KRAS-IRF2 Axis Drives Immune Suppression and Immune Therapy Resistance in Colorectal Cancer

Co-authors: Wenting Liao, Michael J Overman, Adam T Boutin, Xiaoying Shang, Di Zhao, Prasenjit Dey, Jiexi Li, Guocan Wang, Zhengdao Lan, Jun Li, Ming Tang, Shan Jiang, Xingdi Ma, Peiwen Chen, Riham Katkhuda, Krittiya Korphaisarn, Deepavali Chakravarti, Andrew Chang, Denise J Spring, Qing Chang, Jianhua Zhang, Dipen M Maru, Dean Y Maeda, John A Zebala, Scott Kopetz, Y Alan Wang and Ronald A DePinho

Y. Alan Wang, Ph.D.
Associate Professor
Cancer Biology
Laboratory Director, DePinho Laboratory

Ronald A. DePinho, M.D.
Past President
Professor
Cancer Biology
Harry Graves Burkhart III Distinguished University Chair in Cancer Research
Wangtong Yao, Ph.D., and Giulio Draetta, M.D., Ph.D.

Wangtong Yao, Ph.D.
Assistant Professor
Translational Molecular Pathology

Giulio Draetta, M.D., Ph.D.
Senior Vice President, Chief Scientific Office
Professor, Genomic Medicine and Molecular & Cellular Oncology
Sewell Family Chair in Genomic Medicine in honor of Lynda Chen, M.D.
Authors
Wantong Yao, Johnathon L. Rose, Wei Wang, Sahil Seth, Hong Jiang, Ayumu Taguchi, Jintan Liu, Liang Yan, Avnish Kapoor, Pingping Hou, Ziheng Chen, Qiuyun Wang, Luigi Nezi, Zhaohui Xu, Jun Yao, Baoli Hu, Piergiorgio F. Pettazzoni, I Lin Ho, Ningping Feng, Vandhana Ramamoorthy, Shan Jiang, Pingna Deng, Grace J. Ma, Peter Den, Zhi Tan, Shu Xing Zhang, Huamin Wang, Y. Alan Wang, Angela K. Deem, Jason B. Fleming, Alessandro Carugo, Timothy P. Heffernan, Anirban Maitra, Andrea Viale, Haoqiang Ying, Samir Hanash, Ronald A. DePinho and Giulio F. Draetta
Nature
Syndecan 1 is a critical mediator of macropinocytosis in pancreatic cancer
Sitting, left to right: Giulio Draetta, Wantong Yao, Hong Jiang
Quarter 4 (June–August 2019)
Li-Chuan Chan, Ph.D., and Liuqing Yang, Ph.D.
Ke Liang, Chunru Lin, Liuqing Yang, Yajuan Li, Qingsong Hu, Jianjun Jiang, Sergey Egranov, Tina Nguyen and Yaohua Zhang
Co-authors not pictured: Youqiong Ye, Li-Chuan Chan, Aifu Lin, Weiya Xia, Jing Gong, Yinghong Pan, Sujash S. Chatterjee, Jun Yao , Kurt W. Evans, Peter K. Park, Jiewei Liu, Cristian Coarfa, Sri Ramya Donepudi, Vasanta Putluri, Nagireddy Putluri, Arun Sreekumar, Chandrashekar R. Ambati, David H. Hawke, Jeffrey R. Marks, Preethi H. Gunaratne, Abigail S. Caudle , Aysegul A. Sahin , Gabriel N. Hortobagyi , Funda Meric-Bernstam , Lieping Chen, Dihua Yu , Mien-Chie Hung, Michael A. Curran and Leng Han

Li-Chuan Chan, Ph.D.
Postdoctoral Fellow
Molecular & Cellular Oncology

Liuqing Yang, Ph.D.
Associate Professor
Molecular & Cellular Biology
Nature Immunology
Oncogenic lncRNA downregulates cancer cell antigen presentation and intrinsic tumor suppression
Peiwen Chen, Ph.D., Y. Alan Wang, Ph.D., and Ronald A. DePinho, M.D.

Peiwen Chen, Ph.D.
Postdoctoral Fellow
Cancer Biology

Y. Alan Wang, Ph.D.
Associate Professor
Cancer Biology
DePinho Laboratory Director

Ronald A. DePinho, M.D.
Past President
Professor
Cancer Biology
Harry Graves Burkhart III Distinguished University Chair in Cancer Research
Cancer Cell
Symbiotic Macrophage-Glioma Cell Interactions Reveal Synthetic Lethality in PTEN-Null Glioma
Second row, left to right: Prasenjit Dey, Peiwen Chen, Di Zhao, Andrew Chang, Denise Spring and Abhishek Dasgupta
Third row, left to right: Jasper R. Chen, Sagar Shah, Carolyn Guan, Rumi Lee, Y. Alan Wang and Hong Seok Shim
Filippo G. Giancotti, M.D., Ph.D.

Filippo G. Giancotti, M.D., Ph.D.
Professor, Cancer Biology
Olla S. Stribling Distinguished Chair in Cancer Research
Scientific Director, David H. Koch Center for Applied Research of GU Cancers
Cancer Cell
The Polycomb Repressor Complex 1 Drives Double-Negative Prostate Cancer Metastasis by Coordinating Stemness and Immune Suppression
Nitin Jain, M.B.B.S., Varsha Gandhi, Ph.D., and William Wierda, M.D., Ph.D.

Nitin Jain, M.B.B.S.
Associate Professor
Leukemia

Varsha Gandhi, Ph.D.
Professor, Departments of Experimental Therapeutics & Leukemia
Chair Ad Interim, Department of Experimental Therapeutics
Faculty Liaison, Office of Postdoctoral Affairs and Development

William Wierda, M.D., Ph.D.
Professor and Deputy Chair
Leukemia
Center Medical Director, Leukemia Center
Executive Director, Inpatient Medical Operations
New England Journal of Medicine
Ibrutinib and Venetoclax for First-Line Treatment of CLL
Florencia McAllister, M.D.
Cell
Tumor Microbiome Diversity and Composition Influence Pancreatic Cancer Outcomes
Authors
Erick Riquelme, Yu Zhang, Liangliang Zhang, Maria Montiel, Michelle Zoltan, Wenli Dong, Pompeyo Quesada, Ismet Sahin, Vidhi Chandra, Anthony San Lucas, Paul Scheet, Hanwen Xu, Samir M. Hanash, Lei Feng, Jared K.Burks, Kim-Anh Do, Christine B. Peterson, Deborah Nejman, Ching-Wei D. Tzeng, Michael P. Kim, Cynthia L. Sears, Nadim Ajami, Joseph Petrosino, Laura D. Wood, Anirban Maitra, Ravid Straussman, Matthew Katz, James Robert White, Robert Jenq, Jennifer Wargo and Florencia McAllister

Florencia McAllister, M.D.
Assistant Professor
Clinical Cancer Prevention & GI Medical Oncology
Xiaofei Zhou, Ph.D., and Shao-Cong Sun, Ph.D.

Xiaofei Zhou, Ph.D.
Instructor
Immunology

Shao-Cong Sun, Ph.D.
Deputy Chair, Immuology
Administrative Director, South Campus Research Bldg
Moshe Talpaz Endowed Chair in Immunology
Left to right: Xuhong Cheng, Shao-Cong Sun and Xiaofei Zhou
Co-authors not pictured: Jiayi Yu, Baoyu Zhao, Ganiraju C. Manyam, Li Zhang, Kimberly Schluns, Pingwei Li and Jing Wang
Nature Immunology
The deubiquitinase Otub1 controls the activation of CD8+ T cells and NK cells by regulating IL-15-mediated priming
Give Now
Research Areas
Find out about the four types of research taking place at UT MD Anderson.

