Food on the brain: Internal mechanisms behind obesity
Has the thought of consuming a bag of chocolate chip cookies or a bag of chips ever hijacked your brain? Well, you might be partially right in that assessment, according to a theory that has prompted an MD Anderson cancer prevention study.
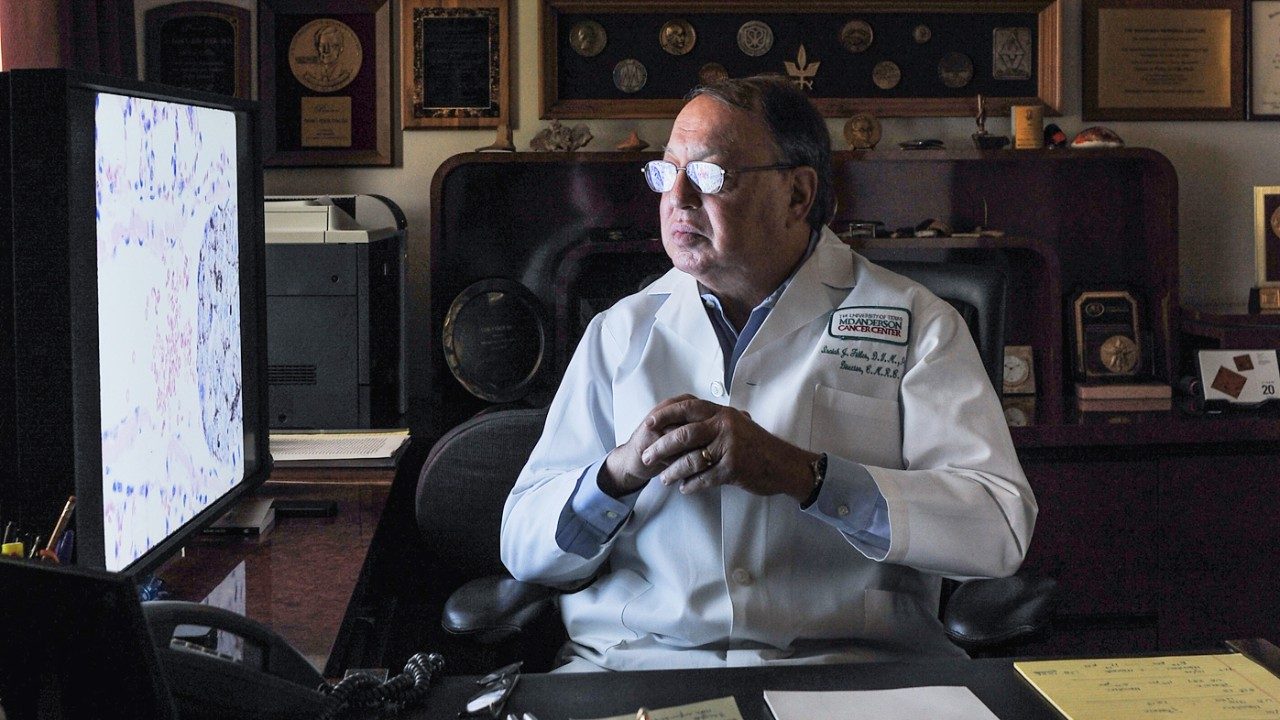
Susan Schembre, Ph.D., and Francesco Versace, Ph.D., assistant professors in Behavioral Science at MD Anderson, have teamed up to explore whether excessive eating is linked to neurological mechanisms — brain-reward responses — similar to those associated with substance-use disorders. They’re guided by recent smoking research in Versace’s lab. Findings there have shown that certain patterns of brain responses to emotional cues or rewards may be key to understanding smoking behavior, cessation and relapse.
In other words, neurological responses may trigger something in our brain that’s responsible for why we overeat. Schembre and her group are using the drug-addiction framework to investigate cognitive and psychological factors that promote excessive weight gain.
Getting to the why of weight gain
“There’s plenty of research on diet and physical activity as an important part of losing and maintaining weight loss,” Schembre says. “There’s less research investigating the reasons why some people overeat and gain or regain an excessive amount of weight.”
For the majority of overweight people, dieting is ineffective. In fact, 80% to 90% of people who lose weight cannot maintain any significant loss. While research shows that a combination of healthy eating and physical activity is the way to weight loss, for most people, sustaining these behaviors can be difficult, leading to weight regain.
Schembre’s new research study, Project Weight, is investigating whether there are differences in brain-reward responses to images of food similar to other emotionally pleasant images among three groups: obese people, obese people in a weight-loss program and lean people with no prior weight issues.
“Our goal is to find a new way to conceptualize strategies and interventions to help people make behavioral changes and live a healthy life at a healthy weight without taking part in popular dieting trends or drastic measures like surgery,” Schembre says.
The facts are daunting
More than one-third of U.S. adults are obese with medical costs of $147 billion in 2008 alone.
Yet, according to the Centers for Disease Control and Prevention, obesity-related conditions — heart disease, stroke, type 2 diabetes and certain types of cancer — cause deaths that might have been prevented.
At MD Anderson, the condition, increasingly referred to as a disease itself, is being addressed on several fronts by behavioral scientists, epidemiologists and clinical cancer prevention experts.
Related stories: