Enhanced Surgery Recovery Program
Surgery for Cancer
About 60% of patients will undergo some type of surgery to treat their cancer. In some cases, surgery is the only treatment required. It may also be combined with chemotherapy or radiation as part of an overall treatment plan.
There are several types of cancer surgery:
Curative surgery simply involves removal of a cancerous tumor. It works best on localized cancers that haven't yet spread to other parts of the body, and is often followed by radiation therapy or chemotherapy to make sure all cancerous cells have been removed.
Preventive surgery is used to keep cancer from occurring. Many colon cancers can be prevented by removing precancerous polyps before they become malignant. Women at high risk for breast cancer due to family history or genetic mutations may decide to have their breasts removed to prevent cancer from occurring. Preventive surgery is also known as prophylactic surgery.
Reconstructive surgery returns the body to normal or near-normal appearance or function following cancer treatment. The most common is breast reconstruction surgery after a mastectomy (breast removal). Facial reconstruction and testicular implants are other examples of reconstructive surgery.
Staging surgery determines the extent of cancer. Staging surgery can sometimes be done without an incision by using an endoscope to view the suspicious area and take a tissue sample. For abdominal tumors, a laparoscope is used to view the area, a procedure that involves a small incision in the abdominal cavity done under general anesthesia.
Supportive surgery is used to help with other cancer treatments. For example, some chemotherapy devices require a port (connecting device) to be inserted under the skin.
Palliative surgery is used to improve a patient’s quality of life by easing pain or other symptoms caused by advanced or untreatable cancer. Palliative surgery is not a cure or anti-cancer treatment.
Minimally invasive surgery employs advanced techniques to remove tumors through tiny incisions. Minimally invasive procedures can also be performed by robotic arms controlled by surgeons. Read more about minimally invasive surgery.
Preparing for surgery
Get information on surgery report times, visitor information, patient discharge and more.
Enhanced Surgery Recovery Program
Research from a worldwide clinical study has found that it takes patients more time to recover from preparing for surgery than from the procedure itself.
For decades, standard practice has required patients to stop eating and drinking up to 12 hours before surgery and to undergo bowel preparation. This results in dehydration and hunger before surgery even begins. Much of a patient's recovery time is spent getting over the side effects of completely stopping the digestive process.
The enhanced surgery recovery program at MD Anderson completely eliminates the need for bowel preparation. Food is allowed until midnight the day before the procedure, and clear liquids can be taken up to two hours before surgery.
After surgery, patients are encouraged to get on their feet that same day, and urinary catheters are removed as soon as possible.
Patients in the program have enjoyed shorter hospital stays, decreased pain, and a quicker return to normal. Ask your care team if enhanced surgical recovery is right for you.
Featured Articles
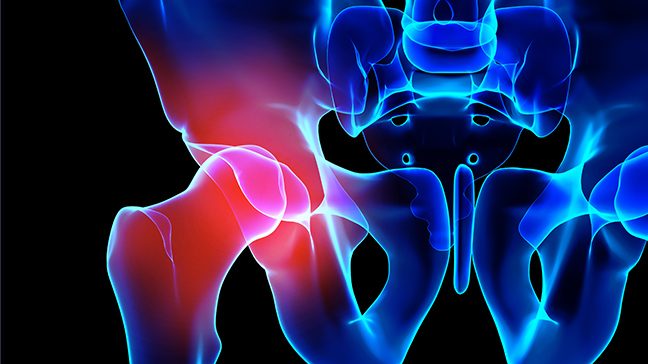
What is a hemipelvectomy?

Surgical drains 101: What to know about their use, care and removal

Stage IV lung cancer survivor: Targeted therapy and surgery left me cancer-free

Fasting before anesthesia: 4 myths, busted

Caring for scar tissue after cancer surgery

One-of-a-kind titanium ribs give chondrosarcoma survivor his life back
request an appointment online.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
