Sections
Section of Molecular Hematology and Therapy
The Molecular Hematology and Therapy section, working closely with other investigators at MD Anderson, primarily conducts basic and translational research in cancer and leukemia. Our basic research programs are supported by funding from the National Institutes of Health (NIH).
Molecular Hematology and Therapy is also the site of the NIH-funded core lab that provides Confocal Microscopy / Image Analysis and Flow Cytometry / Cell Sorting services to researchers at MD Anderson. Three physicians in the section are participating in treating patients with hematopoietic malignancies — in particular, patients with leukemia and patients receiving marrow and stem cell transplants.
Contact Us
Call for assistance: 713-745-2471
Address:
John Mendelsohn Faculty Center (FC3.3038)
1515 Holcombe Blvd. Unit 0425
Houston, TX 77030
Research
Welcome to the Section of Molecular Hematology and Therapy (MHT), Director Michael Andreeff M.D., Ph.D. Molecular changes causing hematological malignancies, including acute myeloid leukemia (AML), are being identified at an unprecedented pace. With this molecular knowledge, we now have the opportunity to develop novel diagnostic and therapeutic tools, which can be translated for clinical use. Members of MHT have made major contributions to the elucidation of critical mechanisms through which tumors develop, and consequently how they can be treated. We work closely with other investigators at MD Anderson to conduct basic and translational cancer research that is envisioned to eradicate AML and other types of cancer.
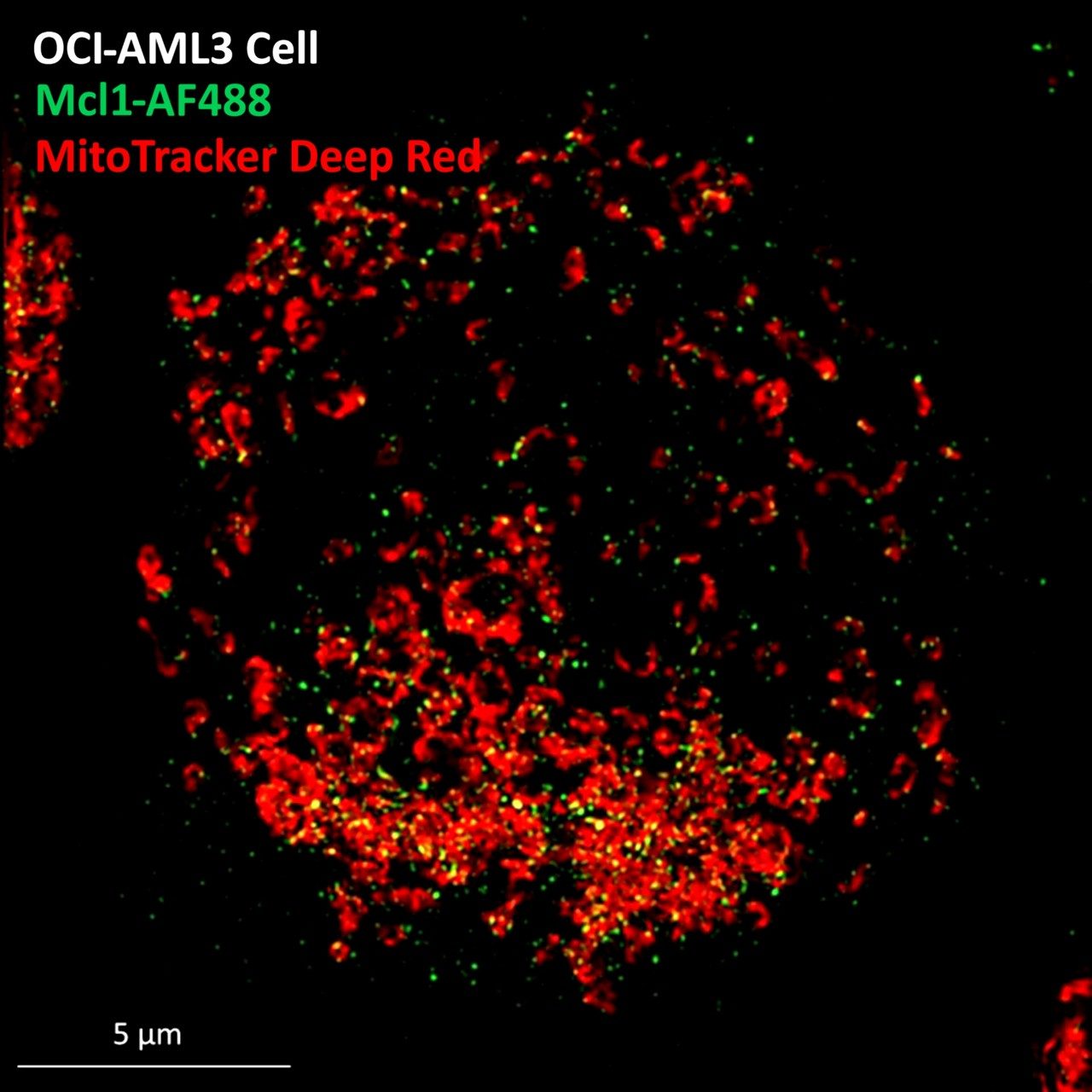
The primary research focus in MHT has been to identify and overcome mechanisms of drug resistance in leukemias. We are investigating and targeting two principal mechanisms: 1) apoptosis-related and 2) microenvironment-mediated drug resistance in AML. For example, we were first to discover that the pro-apoptotic Bcl-2 family member BAD was invariably phosphorylated in all patients with AML, and it functions as an anti-apoptotic protein. Based on this finding that Bcl-2 family members are selectively overexpressed in AML stem cells, and clinical trials with molecular therapeutics targeting these apoptosis regulators are now in progress at MD Anderson and world-wide. In 2006, we published a seminal paper on Bcl-2 inhibitors in Cancer Cell, which facilitated the development of ABT-737, 263, and 199. ABT-199 (venetoclax) has shown over 80% response rate in relapsed/refractory CLL and received FDA approval as a result. Our group then developed ABT-199 (venetoclax) for AML therapy, alone and in combination with demethylating agents (HMAs). We showed pronounced pre-clinical activity, conducted the first clinical trial, and are now engaged in combinatorial trials with MAPK, or other broad-spectrum kinase inhibitors, exportin 1 (XPO1) inhibitors, or MDM2 inhibitors, for which we have considerable pre-clinical validation. In fact, we published a seminal paper in Cancer Cell that showed superior treatment efficacy of the ABT-199 and RG7388, an MDM2 inhibitor, combination against AML, which is being validated in clinical trials. The combination of venetoclax and HMAs has already revolutionized the treatment of AML and is yielding response rates of >90% in patients unfit for conventional therapy. The venetoclax/HMA combination for AML was also FDA approved. As another mechanism-based evolutionary step, we have investigated combinations of Bcl-2 and Mcl-1 inhibitors, which shows pronounced synergism, which is also being tested clinically.
We have further pioneered the development of MDM-2 inhibitors to activate, in a non-genotoxic manner, p53 signaling in cancer cells. From their inception, we worked closely with industry collaborators on these inhibitors and conducted the first successful MDM-2 inhibitor trial in leukemias, published in Clinical Cancer Research. We have now developed extensive pre-clinical and in vivo rationale for combinatorial Bcl-2 (i.e., apoptosis sensitization) and MDM-2 (i.e., p53 activation) inhibition, which addresses molecular shortcomings of each individual targeted therapy, and clinical trials examining these treatments are ongoing.
Recently, MHT faculty described the atypical mitochondrial integrated stress response that allows p53 mutation-independent killing of leukemia and lymphoma cells (Science Signaling, 2016). They also identified drugs that activate this pathway, imipridones (e.g., ONC 201 and ONC 212), which are now in clinical trials for numerous tumor types. This work identified a novel target in cancer therapy; activation of the mitochondrial protease ClpP. The close collaboration between the MHT faculty at MD Anderson and scientists at Princess Margaret Research Institute in Toronto resulted in five top-tier publications (Science Signaling, 2016, Oncotarget, 2016, Neoplasia, 2017, Leukemia, 2019, and Cancer Cell, 2019).
Thirty percent of AMLs overexpress the tyrosine kinase FLT3. We were first to identify, in the laboratory and then in the clinic, the tyrosine kinase inhibitor sorafenib (a drug originally developed as a Raf inhibitor for renal cancers) as a highly effective inhibitor of FLT3 ITD in AML. This bench to bedside project exemplifies MHT’s approach to cancer care and the cure of AML. Sorafenib is used world-wide for this purpose, while other more targeted FLT3 inhibitors are being developed. We are also currently developing a multi-kinase inhibitor, CG’806, a first-in-class, small molecule that blocks FLT3/BTK/Aurora kinases, to overcome or prevent FLT3 inhibitor resistance in AML.
Studies conducted during the past two decades have shed light on the understanding of the genetic basis for AML. However, the mechanisms by which AML blasts create an immune-privileged niche and suppress immune responses to evade a patient’s immune system are poorly understood. More recently, new biological insights have been provided supporting the notion that, along with the leukemic cell autonomous defects, cell-extrinsic microenvironmental factors have a crucial role in leukemogenesis and maintenance. In particular, inflammatory networks acting in the milieu surrounding the leukemia blasts appear to play a crucial role in leukemia initiation and progression, as well as in their response to chemotherapy. To better understand the complex microenvironmental relationships in leukemogenesis and therapy, the group recently received a five-year Cancer Prevention and Research Institute of Texas MIRA Program Project Grant to investigate the hypoxic immunosuppressive microenvironment in AML. This project is supported by cutting-edge technologies like time-of-flight mass cytometry (CyTOF) and intravital imaging available from the Confocal Microscopy/ Image Analysis and Flow Cytometry/Cell Sorting Core Laboratory and the Advanced Microscopy Core (Director: Dr. M. Andreeff).
In the area of stem cell research, we established NOD/scid and PDX models of human hematopoiesis, leukemogenesis, and microenvironment, and conducted investigations into the role of the chemokine receptor CXCR4 for engraftment of human leukemic cells in these model systems. Inhibition of CXCR4 with small peptides and chemical inhibitors has promise for the improved collection of normal stem cells by apheresis and also for the prevention of bone metastases of breast cancer cells. In particular, a study of the CXCR4 inhibitor AMD3465 in a metastatic breast cancer model in vitro and in vivo was particularly illuminating and therapeutically promising. As such, it now has become among the top 25% most cited articles in PLOS ONE. Furthermore, inhibition of CXCR4 may facilitate deregulation of let-7a to overcome chemoresistance in AML. This extensive preclinical rationale supports the concept that CXCR4 inhibition in leukemias will be the first step in sensitizing leukemic stem cells to mobilization and chemotherapy and it is envisioned to overcome the microenvironment-mediated resistance mentioned previously. Clinical trials with novel CXCR4 inhibitors are ongoing, highly promising and showing clinical efficacy. In addition to CXCR4, E-selectin and arginase are promising new targets for AML therapy.
MHT members are also currently investigating single-cell DNA and RNA analysis as part of a program titled “Targeting Minimal Residual Disease and Stem-like Cells in High-Risk AML,” which focuses on the molecular characterization of minimal residual disease in p53-mutated AML. The project aims to functionally-identify subsets of leukemia cells that persist in remission and expanded at relapse, characterize their genetic (single cell DNA sequencing), transcriptomic (single-cell RNA sequencing) and proteomic (single cell CyTOF mass spec) signatures, to identify novel targets in these patient fate-determining cells and generate novel CAR T-cells, monoclonal antibodies and pathway modulators that effectively eliminate these AML leukemia relapse-initiating MRD cell subpopulations.
We further discovered that bone marrow-derived mesenchymal stromal cells (MSC) home to the stroma of hematologic malignancies, solid tumors and their metastases, and can be used to produce anti-tumor agents in situ. We discovered that systemic infusion of MSC) that were genetically modified to secrete interferon or other therapeutic cytokines could interfere with the growth and metastasis of a broad range of cancers. This is an exciting strategy for producing therapeutic proteins in the microenvironment of cancers. These groundbreaking approaches are now being used in human cancer therapy that includes an FDA-approved trial for ovarian cancer.
Finally, based on studies of epithelial-to-mesenchymal transition in solid tumors, we identified the first breast cancer stem cell marker the gangliosde GD-2. We are now establishing a program to target GD-2 with small molecule inhibitors, antibodies, and CAR-T-cells. This discovery is patented and offers great potential for the cure of breast cancer and perhaps other epithelial cancers.
All of these innovative programs are supported by funding from the Institution, National Institutes of Health, and the Cancer Prevention and Research Institute of Texas, Leukemia Society, Breast Cancer Research Foundation and other sources. MHT is also the home of the National Institutes of Health-funded Core Laboratory, Dr. Andreeff, Director, which provides confocal microscopy, image analysis, flow cytometry, and cell sorting services, including CyTOF mass cytometry and imaging, to researchers at MD Anderson, and the Advanced Microscopy Core which provides super-resolution, 2-photon intra-vital and soon light sheet imaging.
MHT integrates the work of more than 50 scientists and has a well-established infrastructure that helps young investigators to advance and become independent.
Recent Publications
- An ARC-Regulated IL1β/Cox-2/PGE2/β-Catenin/ARC Circuit Controls Leukemia-Microenvironment Interactions and Confers Drug Resistance in AML.
- BETP degradation simultaneously targets acute myelogenous leukemia stem cells and the microenvironment.
- Mitochondrial ClpP-Mediated Proteolysis Induces Selective Cancer Cell Lethality.
- LGALS3 is connected to CD74 in a previously unknown protein network that is associated with poor survival in patients with AML.
- Concomitant targeting of BCL2 with venetoclax and MAPK signaling with cobimetinib in acute myeloid leukemia models.
- Imipridone ONC212 activates orphan G protein-coupled receptor GPR132 and integrated stress response in acute myeloid leukemia.
- Prognostic significance of baseline FLT3-ITD mutant allele level in acute myeloid leukemia treated with intensive chemotherapy with/without sorafenib.
- Combined inhibition of MDM2 and Bcr-Abl tyrosine kinase targets chronic myeloid leukemia stem/progenitor cells in a murine model.
- Updates on the hematologic tumor microenvironment and its therapeutic targeting.
- Bone marrow niches in haematological malignancies.
- Fatty Acid Metabolism, Bone Marrow Adipocytes, and AML.
- MDM2 inhibition: an important step forward in cancer therapy.
- At the bedside: Profiling and treating patients with CXCR4-expressing cancers.
- Combinatorial Inhibition of Focal Adhesion Kinase and BCL-2 Enhances Antileukemia Activity of Venetoclax in Acute Myeloid Leukemia.
- Targeting MCL-1 dysregulates cell metabolism and leukemia-stroma interactions and resensitizes acute myeloid leukemia to BCL-2 inhibition.
- LGALS1 acts as a pro-survival molecule in AML.
- Phase 1 study of combinatorial sorafenib, G-CSF, and plerixafor treatment in relapsed/refractory, FLT3-ITD-mutated acute myelogenous leukemia patients.
- Combined inhibition of MDM2 and BCR-ABL1 tyrosine kinase targets chronic myeloid leukemia stem/progenitor cells in a murine model.
- Bone marrow stromal cells induce an ALDH+ stem cell-like phenotype and enhance therapy resistance in AML through a TGF-β-p38-ALDH2 pathway.
- BL-8040 CXCR4 antagonist is safe and demonstrates antileukemic activity in combination with cytarabine for the treatment of relapsed/refractory acute myelogenous leukemia: An open-label safety and efficacy phase 2a study.
- First Report of Sorafenib in Patients With Acute Myeloid Leukemia Harboring Non-Canonical FLT3 Mutations.
See also the complete list of PubMed articles, which are among 705 peer-reviewed publications and reviews, and the textbook Targeted Therapy of Acute Myeloid Leukemia (Springer), which has been downloaded more than 75,000 times.
Our Investigators
Andreeff, Michael
Professor and Section Chief
mandreef@mdanderson.org
Borthakur, Gautam
Professor
GBorthak@mdanderson.org
Carter, Bing
Professor
bicarter@mdanderson.org
Ishizawa, Jo
Assistant Professor
JIshizawa@mdanderson.org
Kojima, Kensuke
Adjunct Professor
k-koji@kochi-u.ac.jp
Kornblau, Steven
Professor
skornblau@mdanderson.org
