Radiation Therapy
in the School of Health Professions
Log in to our secure, personalized website to manage your care (formerly myMDAnderson).
If you are ready to make an appointment, select a button on the right. If you have questions about UT MD Anderson’s appointment process, our information page may be the best place to start.
Appointment Informationin the School of Health Professions
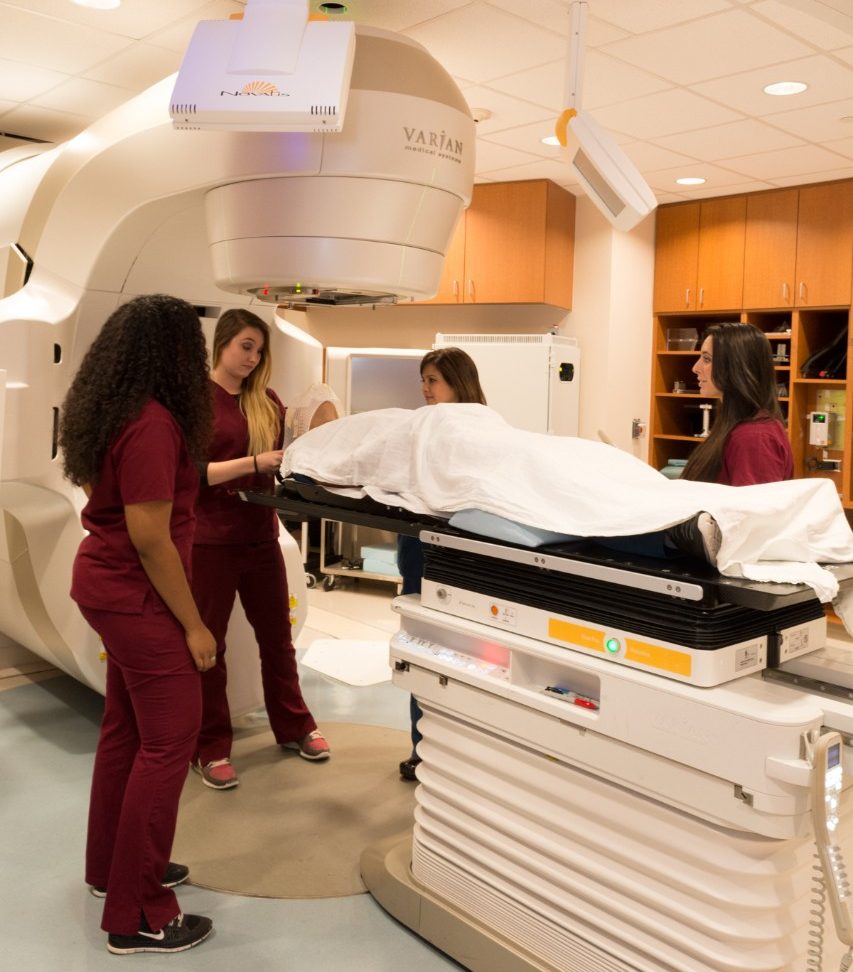
In the School of Health Professions, the Program in Radiation Therapy is designed to prepare students for the technical, theoretical, and psychological aspects of this career.
You can find out more about the radiation therapy professional's role at the ASRT's Careers in Radiologic Technology site.
View the 2025 Radiation Therapy Virtual Brochure (pdf)
The program offers a two-year track with two educational delivery options leading to the Bachelor of Science degree. See the prerequisites and FAQs (pdf).
Students are educated in our state-of-the-art radiation oncology center, where more than 4,000 new patients are treated each year.





Program Director Shaun T. Caldwell, Ed.D.
Associate Program Director Sandra John-Baptiste, M.Ed.
Executive Advisor
Eric A. Strom, M.D., F.A.C.R.
Professor, Department of Radiation Oncology
Division of Radiation Oncology
MD Anderson Cancer Center
The Radiation Therapy program is accredited by the Joint Review Committee on Education in Radiologic Technology (JRCERT). The program’s current award is accreditation for a period of 8 years. General program accreditation information and the current accreditation award letter can be found on the JRCERT web page.
JRCERT
20 N. Wacker Dr., Ste 2850
Chicago, IL 60606-3182
Phone 312-704-5300
Email mail@jrcert.org
Upon completion of the program, students will qualify for examination and certification from the American Registry of Radiologic Technologists (ARRT).
The Radiation Therapy Program is a rigorous six-semester commitment including summer semesters. Students must demonstrate the knowledge and skills gained in the classroom to treat patients in the clinical environment. Clinical education requires students to demonstrate competency, continued competency, and professional growth/professionalism in our designated Radiation Oncology centers. The Radiation Therapy Program faculty take a personal interest in the success of every student. Students admitted to the Program receive a Student Handbook of policies and procedures, routine academic and professional advising, and tutoring is available on request.
Students must attend all didactic and clinic courses assigned. Student schedules require attendance two consecutive 8-hour days in the clinic and three days in class during the Program's first year. During the second year of the Program, students attend clinical education three days (24 hours) each week in the clinical setting and two days in the classroom. Typically, the didactic courses are from 9:00 am-4:00 pm, and clinical education is from 7 a.m.-4 p.m. on non-class days. Some classes may be offered in the evenings or online. In this situation, students are notified in advance.
Students must complete the courses in order as published in the Radiation Therapy Curriculum and are required to earn a C grade or higher in every class to progress to the next academic semester.
Throughout the two years, students must attend experience at various clinical locations. Therefore, students must have reliable transportation to travel up to 50 miles for clinical education.
Students must attend all class activities and clinical education as scheduled. Unfortunately, the Program cannot make accommodations for student working schedules. In other words, students must make arrangements with their employers so that they can adhere to class and clinic schedules.
The mission of the Radiation Therapy Program is to provide the highest quality of education to radiation therapy students through formal didactic and state-of-the-art clinical experiences that prepare the student to deliver superior patient care and treatment in all aspects of radiation therapy.
We shall be the premier provider of education for radiation therapy professionals based on best practices and research in radiation oncology.
Goal 1. Students will be clinically competent.
Student Learning Outcomes
1. Students will accurately assess the patient's status prior to discharge from their care.
2. Students will demonstrate reproduction of the patient's initial setup.
3. Students will demonstrate superior paitent care skills.
Goal 2. Students will display critical thinking skills.
Student Learning Outcomes
1. Students will evaluate and interpret data.
2. Students will recognize discrepancies in treatment.
3. Students will develop solutions to clinical situations.
Goal 3. Students will display effective communication skills.
Student Learning Outcomes
1. Students will communicate with patients.
2. Students will demonstrate written communication skills.
3. Students will demonstrate oral presentation skills.
Goal 4. Students will demonstrate professionalism.
Student Learning Outcomes
1. Students will discuss patient information and setup out of hearing of inappropriate people.
2. Students will assume full responsibility for their actions.
3. Students will accept constructive criticism.
The program has developed affiliations with medical institutions across the United States, so that students will develop expertise in a variety of settings and experience the breadth of opportunity available to a certified radiation therapist. During the clinical phase of instruction, training and supervision are provided in affiliated hospitals and clinical laboratories.
Affiliated clinics for distance-learning students.
The goal of Radiation Therapy is to deliver a high dose of radiation to a tumor while sparing the normal tissues. The Radiation Therapist is an integral part of the health care team. Radiation Therapists have significant patient interaction daily. A Radiation Therapist plans, delivers, records and monitors radiation therapy treatments.
According to The Practice Standards for Medical Imaging and Radiation Therapy (pdf) published by the American Society of Radiologic Technologists (ASRT),
“Radiation therapy integrates scientific knowledge, technical competence and patient interaction skills to provide safe and accurate treatment with compassion. A radiation therapist recognizes patient conditions essential for the successful completion of simulation and treatment.
Radiation therapists must demonstrate an understanding of human anatomy, human physiology, pathology and medical terminology.
In addition, comprehension of oncology, radiobiology, radiation physics, radiation oncology techniques, radiation safety and the psychosocial aspects of cancer are required. They must maintain a high degree of accuracy in positioning and treatment techniques. Radiation therapists must possess, use and maintain knowledge about radiation protection and safety. Radiation therapists assist the radiation oncologist to localize the treatment area, participate in treatment planning and deliver high doses of ionizing radiation as prescribed by the radiation oncologist.
Radiation therapists are the primary liaison between patients and other members of the radiation oncology team. They also provide a link to other health care providers, such as social workers and dietitians. Radiation therapists must remain sensitive to the needs of the patient through good communication, patient assessment, patient monitoring, and patient care skills. Radiation therapy often involves daily treatments extending over several weeks using highly sophisticated equipment. It requires thorough initial planning as well as constant patient care and monitoring. As members of the health care team, radiation therapists participate in quality improvement processes and continually assess their professional performance.
Radiation therapists think critically and use independent, professional and ethical judgments in all aspects of their work. They engage in continuing education, to include their area of practice, to enhance patient care, radiation safety, public education, knowledge and technical competence.” (ASRT, 2017, p. RT3).
The following is the most current program effectiveness data. Our programmatic accreditation agency, the Joint Review Committee on Education in Radiologic Technology (JRCERT), defines and publishes this information. Click here to go directly to the JRCERT webpage.
Credentialing Examination: The number of students who pass, on the first attempt, the American Registry of Radiologic Technologists (ARRT) certification examination, or an unrestricted state licensing examination, compared with the number of graduates who take the examination within six months of graduation. The five-year average benchmark established by the JRCERT is 75%.
| Credentialing Examination Rate | number passed on 1st attempt divided by number attempted within 12 months of graduation |
|---|---|
| Year | Results |
| Year 1 - 2021 | 23 of 23 - 100% |
| Year 2 - 2022 | 16 of 17 - 94% |
| Year 3 - 2023 | 22 of 23 - 96% |
| Year 4 - 2024 | 14 of 17 - 82% |
| Year 5 - 2025 | 21 of 22 - 96% |
| Program 5-Year Average | 96 of 102 - 94% |
Job Placement: The number of graduates employed in the radiologic sciences compared to the number of graduates actively seeking employment in the radiologic sciences within twelve months of graduating. The five-year average benchmark established by the JRCERT is 75%.
| Job Placement Rate | number employed divided by number actively seeking employment within 12 months of graduation |
|---|---|
| Year | Results |
| Year 1 - 2021 | 18 of 18 - 100% |
| Year 2 - 2022 | 17 or 17 - 100% |
| Year 3 - 2023 | 23 of 23 - 100% |
| Year 4 - 2024 | 17 of 17 - 100% |
| Year 5 - 2025 | 22 of 22 - 100% |
| Program 5-Year Average | 102 of 102 - 100% |
Program Completion: The number of students who complete the program within the stated program length. The annual benchmark established by the program is 80%.
| Program Completion Rate | number enrolled divided by number of graduates |
|---|---|
| Year | Results |
| Year 1 - 2025 | 22 of 25 |
| Annual Completion Rate | 88% |
Shaun Caldwell
713-792-3455
SCaldwell@mdanderson.edu
School of Health Professions
713-745-1205
askSHP@mdanderson.edu
Learn more about our faculty and research taking place in our labs.
View conferences available for continuing education credit.